* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Thyroid Gland Lecture
Survey
Document related concepts
Transcript
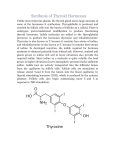
Ms Veena Shriram Introduction Described first by Thomas Wharton (1616-1673) Largest Endocrine Gland Weighing 15 – 20 g Highly Vascular ( 5 ml / g / min ). Veena Functional Anatomy •Thyroid : shield • Two lobes are connected by isthmus infront of the larynx •Receives highest rate of blood flow per gram of tissue •Histologicaly made up of multiple of closed follicles (acini): 100 – 300 µm. Veena Contd. .. THYROID GLAND HISTOLOGY Veena http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/thyroid/anatomy.html • Follicles are lined with single layer of cuboidal epithelial cells, which secrete into interior . • Filled with proteinaceous matter: colloid, made up of large glycoprotein thyroglobulin containing thyroid hormones within it. Inactive gland: Follicles - large Colloid – abundant Cells lining are flat Veena Active gland: Follicles - small Cells lining are cuboid Reabsorption lacunae seen Fetal Thyroid From 12th week of gestation fetal thyroid begins to secrete hormones. Th. Hormones (T. H.) are essential for normal growth & development of fetal CNS , skeletal systems. Maternal TSH & thyroxine cannot cross placental barrier, however iodine can cross the barrier. Fetal T. H. production depends on ant. pituitary & fetal hypothalamus. Veena THYROID HORMONES OH OH I I I I I O O NH2 I O Thyroxine (T4) Veena OH NH2 I O OH 3,5,3’-Triiodothyronine (T3) Synthesis & secretion of T. H. 1. Iodide Trapping 2. Formation & secretion of thyroglobulin 3. Oxidation of iodide ions 4. a) Iodination of tyrosine b) Organification of TG 5. Storage of TG 6. Release of T.H. : T4 & T3 Veena 93 % hormone secreted by T. gland is Thyroxine (T4). 7 % is triiodothyronine (T3). T3 is: 4 times more potent than T4 present in smaller quantities Persists for shorter time than T4 Veena Iodine Metabolism Iodine is a raw material for T. H. synthesis. Ingested iodine is converted into iodide Daily avg. intake of iodine is 500 µg/ day . Min. daily intake to maintain normal T. function 150 µg/ d Normal plasma iodine level is about 0.3 µg/ dL . To prevent iodine deficiency common table salt is iodized with 1 part Na iodide to every 1,00,000 parts of NaCl. Fate of Ingested iodides: absorbed from GIT into blood. 1/5th is taken up by T. gland and rest is excreted by kidneys. Veena 1. Iodide Pump (Iodide Trapping) Food iodide from blood is , taken up by the follicular cells of thyroid – a process called iodide trapping. Thyroid cells RMP is -50 mV compared to interstitial fluid & luminal colloid. The T. cell membrane facing capillaries contain a + - symporter or iodide pump : Na / I symporter (NIS) It works against electrochemical gradient & traps iodide by secondary active transport mechanism. It concentrates the iodide 30 – 250 times than in the blood. Veena 2. Formation & secretion of thyroglobulin T. cells are typical protein secreting glandular cells. ER & GA synthesize & secrete into the follicles, a large glycoprotein molecule : thyroglobulin (TG - with MW 3,35,o00) TG contains about 70 tyrosine amino acids. Tyrosine combines with iodide to form T. H. ( within TG molecule). Veena 3. Oxidation of Iodide ions Conversion of the iodide ions to an oxidized form of iodine (either nascent iodine, I0 or I-3) by the enzyme peroxidase in presence of H2O2. Peroxidase is attached to apical membrane of the cell. This oxidized form of iodine can combine with the a. a. tyrosine. Veena 4. a) Organification of thyroglobulin 1. Organification of thyroglobulin (TG): The binding of iodine with TG molecule is called organification. 2. Oxidized iodine in presence of enzyme iodinase binds very rapidly with thyroglobulin. Veena ION TRANSPORT BY THE THYROID FOLLICULAR CELL ClO4 -, SCN- Perchlorate, thiocynate depress I transport by competitive inhibition BLOOD I- I- NaI symporter (NIS) Thyroid peroxidase (TPO) Veena organification COLLOID Propylthiouracil (PTU) blocks iodination of thyroglobulin 4. b) Iodination of Tyrosine Tyrosine + oxidized iodine monoiodotyrosine(MIT) I0 or I-3 diiodotyrosin (DIT) Coupling :- Veena MIT + DIT Triiodotyrosine (T3) DIT + MIT RT3 Biosynthesis of TH . qq qq Organification IApical membrane Peroxidase I- Golgi I- E.R. I- trap Basal membrane Veena I- . Storage & Release of TG 5. STORAGE After synthesis of TH , TG molecules contain up to 30 molecules of T4 & few molecules of T3 2-3 months requirement is stored. 6. RELEASE The follicle cells engulf a little TG (containing T4 & T3) by endocytosis (by formation of reabsorption lacunae). TG is digested by proteinase and T4 & T3 are set free After cleaving of T4 & T3 from TG, free H is released into capillaries. Veena Synthesis & Release Veena 3/4th of iodinated tyrosine in the TG never becomes TH, but remains MIT, DIT. During digestion of TG for release of T4 & T3 , iodinated tyrosins are also freed from TG, but not released into blood Instead I is cleaved by deiodinase enzyme. Thus recycling I. Congenital absence of this enzyme lead to I deficiency. Veena Daily Rate of Secretion 93 % T4 7% T3 is released. Later half of the T4 is slowly deiodinated to T3 Finally T3 is mainly delivered to & used by tissues, a total about 35 µg / d. Veena Transport of TH In The Blood Approximately 99 % of T4 is bound to 3 plasma proteins: Thyroxine binding globulin (TBG) ~75%; Thyroid binding prealbumin (TBPA or transthyretin) 1520 %; albumin ~5-10 % Only ~0.02% of the total T4 in blood is unbound or free. Only ~0.4% of total T3 in blood is free. Veena Slow release of T4 & T3 to the tissues T4 & T3 are released slowly to the tissues because of high affinity with TBG of T4 Half quantity of T4 is released in 6 days and that of T3 in 1 day After entering tissues again it binds with protein & used slowly. Veena Slow onset & long duration of action This is due to binding with proteins both in plasma & tissue cells, and due to the way they act. T3 is 4 times rapid than T4 . Veena Mechanism of Action transcription of large no. of genes, therefore large no. of proteins, enzymes, & other substances are synthesized. generalized in functional activity High affinity of intracellular TH receptor for T3 TH activate nuclear receptors (TRα on gene 17 & TRβ R on gene 3 ) & initiate the transcription process. mRNA formation, then RNA translation Veena Mechanism of Action Veena