* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 8. Anti-diabetics
Discovery and development of integrase inhibitors wikipedia , lookup
Discovery and development of dipeptidyl peptidase-4 inhibitors wikipedia , lookup
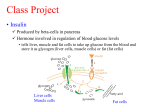
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
DRUGS FOR THE TREATMENT OF DIABETES MELLITUS 1 • One of the leading cause of death by diseases (cardiovascular problems, stroke) • One of the leading cause of blindness • One of the leading cause of renal failure • One of the leading cause of impotence (males) • Risk of foot amputation 2 Types of diabetes Type I (formally IDDM or juvenile). Type II (formally NIDDM or adult). Secondary diabetes(occur only if there is an underlying disease) e,g,: cushing disease, pancreatectomy, growth hormone tumor. Gestational diabetes. N.B. IDDM: insulin dependent diabetes mellitus. NIDMM: non-insulin dependent diabetes mellitus. 3 Characteristic Type 1 ( 10% ) Type 2 (90%) Onset (Age) Usually < 30 Usually > 40 Type of onset Abrupt Gradual Nutritional status Usually thin Usually obese Clinical symptoms Polydipsia, polyphagia, polyurea, weight loss Often asymptomatic due to insulin’s presence Ketosis Frequent (acetone aroma) Usually absent Endogenous insulin Absent Present, but relatively ineffective Related lipid abnormalities Hypercholesterolemia frequent, all lipid fractions elevated in ketosis Cholesterol & triglycerides often elevated; carbohydrateinduced hypertriglyceridemia Insulin therapy Required Hypoglycemic drugs Should not be used Required in 20 - 30% of patients (for postprandial hyperglycemia) Clinically indicated Diet Mandatory with insulin Mandatory with or without drug (can be controlled by diet & exercise) 4 carbohydrates • ↑glucose uptake. • ↑glycogen synthesis (↑storage). • ↑glycolysis (in muscles). • ↑conversion of cyrbohydrate to fat (lypogenesis). • ↓gluconeogenesis. fat • ↑lypolysis. protein • ↑amino acid uptake (protein synthesis). potassium • ↑ K+ uptake to cells. ↓ glucose uptake hyperglycemia ↑amino acid mobilization ↑ lipolysis glycosuria ↑plasma amino acid ↑ plasma free fatty acid ketosis dehydration Amino acid glucose (gluconeogenesis) acidosis Some notes: Glucose is reabsorbed in the kidney tubules in the form of glucose 6 phosphate. In diabetic patients glucose filtration floods the renal tubules exceeding 180 g/dl, threshold for glucose’s reabsorption, leading to the appearance of glucose in the urine (glucosuria). This results in osmotic dragging of water into the tubules resulting in polyuria with subsequent polydypsia. 7 Insulin Degradation Hydrolysis of the disulfide linkage between α & β chains. Metabolism of insulin: Endogenous: 60% in liver & 40% in kidney (because it goes directly to the liver by the portal circulation). Exogenous: 60% kidney & 40% liver Half-Life 5-7min (endogenous insulin) Delayed-release form( injected one) • Pregnant women with type II or gestational DM should take insulin by injection and avoid taking oral hypoglycemics. 8 cont’d Upper arm (intermediate action) Site of injection Abdomen (fast action) Thigh (slow action) Category B (not teratogenic) The site of injection should be changed every once in a while, (Injection in same place hypertrophy to subcutaneous tissue ↓ absorption) Should be stored in refrigerator & warm up to room temp before use. Must be used within 30 days. 9 Fast action of insulin in the abdomen 10 TYPES OF INSULIN PREPARATIONS A) Insulin used to control postprandial (after meals) hyperglycemia and emergency ketoacidosis 1. Ultra-short-acting ( e.g. insulin lispro, insulin aspart) 2. Short-acting -Regular- (e.g. Novolin R, Humulin R) Clear liquid B) Insulin used for maintenance treatment of type I DM 3. Intermediate-acting (NPH, Lente insulin) Turbid suspension عكر 4. Long-acting (Glargine ,Ultralente ) N.B. NPH = Neutral protamine Hagedorn 11 Short-acting (regular) insulins e.g. Humulin R, Novolin R Ultra-Short acting insulins e.g. Lispro, aspart, glulisine Uses Designed to control postprandial hyperglycemia & to treat emergency diabetic ketoacidosis Similar to regular insulin but designed to overcome the limitations of regular insulin Physical characteristics Clear solution at neutral pH Clear solution at neutral pH Chemical structure Hexameric analogue dimeric monomeric Monomeric analogue Route & time of administration S.C. 30 – 45 min before meal I.V. in emergency (e.g. diabetic ketoacidosis) S.C. 5 min (no more than 15 min) before meal I.V. in emergency (e.g. diabetic ketoacidosis) Onset of action 30 – 45 min ( S.C ) 0 – 15 min ( S.C ) Peak serum levels 2 – 4 hr 30 – 90 min Duration of action 6 – 8 hr (thus creating a risk of nocturnal hypoglycemia) 3 – 4 hr (less risk of nocturnal hypoglycemia) Usual administration 2 – 3 times/day or more or when you need 2 – 3 times / day or more or when 12 you need Advantages of Insulin Lispro (ultrashort) vs Regular Insulin (short acting) : Rapid onset of action ( patients will not wait long before they eat ). 2) Its duration of action is no longer than 3-4 hrs regardless of the dose. 3) Decreased risk of postprandial hypoglycemia 4) Decreased risk of hyperinsulinemia 1) 13 In emergency you can use either ultra-short or regular insulin (no difference in the duration of action because it is given IV) Ultra-short has less duration of action no hypoglycemia قواعد جوهرية In postprandial hyperglycemia you can use both but Use ultra-short, wait for 5 minutes before having a meal while in regular, wait for 30 minutes 14 3. Intermediate - acting insulins Isophane (NPH) (Humulin N; Novolin N, etc.) • Turbid suspension (shaken before use) • Injected S.C. (Only) • Onset of action 1 - 2 hr • Peak serum level 5 - 7 hr • Duration of action 13 - 18 hr Insulin mixtures Isophane (NPH) Ultra-short or short acting 75/25 70/30 50/50 ( mix isophane with ultra-short or short acting insulin). Insulin mixture is given to patients with high postprandial hyperglycemia (contd.) Lente insulin (Humulin L; Novolin L). Turbid suspension Mixture of 30% semilente insulin small crystals rapidly acting 70% ultralente insulin large crystals slow acting with prolonged duration Injected S.C. (only) Onset of action 1 - 3 hr Peak serum level 4 - 8 hr Duration of action 13 - 20 hr 16 Cont’d Lente and NPH insulins • have the same effect. • given once or twice a day. N.B: They are not used during emergencies (e.g. diabetic ketoacidosis). 17 4. Long – acting insulins e.g. Glargine ( Lantus ) Insulin glargine Onset of action: 2 hr Absorbed less rapidly than NPH or Lente insulins Duration of action up to 24 hr Designed to overcome the disadvantages of intermediately acting insulins Advantages 1. 2. Constant circulating insulin over 24 hr with no pronounced peak (see next slide) Safer than NPH & Lente insulins ( less risk of nocturnal hypoglycemia) Nocturnal = أثناء النوم 3. Clear solution (does not require resuspension before administration) 18 Profile of Insulin Glargine vs NPH NPH Glargine glargine (plateau ) 19 In the previous figure NPH gives a peak hypoglycemia But glargine doesn’t give a peak hypoglycemia risk of risk of N.B: intermediate & long acting use for maintenance of blood sugar during 24 hr in type I DM 20 Glargine 21 Methods of Adminisration Insulin Syringes (most common) Pre-filled insulin pens (expensive) External insulin pump Under Clinical Trials Oral tablets 2. Inhaled aerosol (still undergoing trials) 3. Intranasal, Transdermal 4. Insulin Jet injectors (needle less) 5. Ultrasound pulses 1. 22 COMPLICATIONS OF INSULIN THERAPY 1. Severe Hypoglycemia (< 50 mg/dl ) life-threatening Treatment of hypoglycemia Occurs in Overdose of insulin Excessive exercise A meal is missed Give sugar IV (dextrose) Give glucagon 2. Weight gain 23 Cont’d 3. Local or systemic allergic reactions (rare) 4. Insulin resistance (when the patient needs more than 200 units/day) (IgG anti-insulin antibodies, infection, expired insulin(rare)). 5. Lipohypertrophy at injection sites 6. Hypokalemia N.B. In infection (stress); there is an increase catecholamine, corticosteroid leading to insulin resistance. 24 Severe insulin reaction (Hypoglycemic Shock) Diabetic coma (Diabetic Ketoacidosis) Onset Rapid Slow- Over several days Insulin Excess Too little Acidosis & dehydration No Ketoacidosis Signs and symptoms B.P. Normal or elevated Subnormal or in shock Respiration Normal or shallow Deep & air hunger Skin Pale & Sweating Hot & dry CNS Tremors, mental confusion, General depression sometimes convulsions Blood sugar Lower than 70 mg/100cc Elevated above 200 mg/100cc Ketones Normal Elevated 25 Oral Hypoglycemics All taken orally in the form of tablets. Patients with type II diabetes have two physiological defects: 1. 2. Abnormal insulin secretion (most important) Resistance to insulin action in target tissues associated with decreased number of insulin receptors 26 Oral Anti-Diabetic Agents 1. 2. 3. 4. 5. 6. Sulfonylureas e.g. Tolbutamide, Glyburide. Meglitinides e.g. Repaglinide, Nateglinide. Biguanides e.g. Metformin. Alpha-glucosidase inhibitors e.g. Acarbose. Thiazolidinediones e.g. Pioglitazone. Dipeptidyl peptidase-4 inhibitors e.g. Sitagliptin, vildagliptin 27 sulfonylureas Second generation First generation Short acting tolbutamide Intermediate acting Acetohexamide tolazamide More selective an smaller dose Long acting chlorpropamide Short acting Glipizide gliclazide Long acting Glyburide (glibenclamide) glimepiride FIRST GENERATION SULPHONYLUREA COMPOUNDS Tolbutamide short-acting Acetohexamide intermediateacting Tolazamide intermediateacting Well Well Slow Well Metabolism Yes Yes Yes Yes/no*** Metabolites Inactive* Active +++ ** Active ++ ** Inactive ** Half-life 4 - 5 hrs 6 – 8 hrs 7 hrs 24 – 40 hrs Duration of action Short (6 – 8 hrs) Intermediate (12 – 20 hrs) Intermediate (12 – 18 hrs) Long ( 20 – 60 hrs) Excretion Urine Urine Urine Urine Absorption Chlorpropamide long- acting (not preferred) * Good for patients with renal impairment ** Patients with renal impairment can expect long t1/2 *** Chlorpropamide isn’t well metabolized st N.B. All 1 G Metabolized in liver. 29 SECOND GENERATION SULPHONYLUREA COMPOUNDS Glipizide Shortacting Absorption Metabolism Metabolites Half-life Well Yes Inactive 3 – 4 hrs Glibenclamide (Glyburide) Long-acting Well Yes Inactive Less than 3 hrs Glimepiride Long-acting Well Yes Inactive 5 - 9 hrs (hit and run) Duration of action Excretion 10 – 16 hrs 12 – 24 hrs 12 – 24 hrs Urine Urine Urine 30 MECHANISM OF ACTION OF SULPHONYLUREAS (SU) 1) Release of insulin from β-cells* (hence, no use in type 1 DM). 2) Reduction of serum glucagon concentration.(in long term use) 3) Potentiation of insulin action on target tissues. - SU’s binds to k+ channel no efflux depolarization Opening of voltage gated Calcium channel insulin release 31 Sulphonylureas ( Cont.) CLINICAL USE: Approved for monotherapy and in combination with metformin or thiazolidinediones in type II DM Taken before each meal, 1-2 times/day 32 SIDE EFFECTS OF SULPHONYLUREAS 1) Nausea, vomiting, abdominal pain, diarrhea 2) Hypoglycaemia 3) Dilutional hyponatraemia & water intoxication (Chlorpropamide) because it ↑ADH 4) Disulfiram*-like reaction with alcohol (Chlorpropamide) “contain sulfur” Disulfiram R: Ingestion of chlorpropamide with alcohol hyperemic flush 5) Weight gain alcoholism * Disulfiram is a drug used to support the treatment of chronic alcoholism by producing an acute sensitivity to alcohol. 33 CONTRAINDICATIONS OF SULPHONYLUREAS 1) Type 1 DM ( insulin dependent) 2) Parenchymal disease of the liver or kidney. metabolism excretion 3) Pregnancy, lactation (due to the physiologic stress, not teratogenicity) 4) Major stress. 34 DRUGS THAT AUGMENT THE HYPOGLYCEMIC ACTION OF SULPHONYLUREAS Sulfonamides (increase insulin secretion) Warfarin (displace the drugs ↑t1/2 ) Salicylates (displace the drugs ↑t1/2 ) Propranolol (mask the hypoglycemia) Alcohol (acute) Liver enzymes inhibitors ↑SU conc. 35 DRUGS THAT ANTAGONIZE THE HYPOGLYCEMIC ACTION OF SULPHONYLUREAS Thiazide diuretics (a K+ opener hyperpolarization no release of insulin) Corticosteroids ↓sensitivity of insulin Epinephrine Liver enzymes inducers e.g. alcohol (in chronic alcohlic patients ) 36 MEGLITINIDES e.g. Repaglinide, Nateglinide (SU without sulfur) PKs: Taken orally Rapidly absorbed ( Peak approximately 1hour ) Metabolized by liver t1/2 = 1 hr Duration of action 4-5 hr 37 MEGLITINIDES (Contd.) MECHANISM OF ACTION Bind to the same KATP Channel as do Sulfonylureas, to cause insulin release from β-cells. They bind to K channels no K efflux depolarization of β cells opens Ca channel influx release of insulin 38 MEGLITINIDES (Contd.) CLINICAL USE Approved for monotherapy and in combination with metformin in type 2 diabetes Taken before each meal, 3 times / day Does not offer any advantage over sulfonylureas We can use it if the patient is allergic to sulfonylurea SIDE EFFECTS: Hypoglycemia Weight gain( less than sulfonylureas ) Caution in patients with renal & hepatic impairement. 39 BIGUANIDES e.g. Metformin PKs: Given orally Do not bind to plasma proteins Not metabolized Excreted unchanged in urine t 1/2 2 hr 40 BIGUANIDES (Contd.) MECHANISM OF ACTION 1. Increase peripheral glucose utilization (increase insulin receptor sensitivity thus is insulin dependent) 2. Inhibits gluconeogenesis 3. Impaired absorption of glucose from the gut 41 Advantages of Metformin over SUlfonylurea Does not cause hypoglycemia because they don’t stimulate the release of insulin from pancreas no hypoglycemia Does not result in weight gain because they ↓appetite. 42 BIGUANIDES (Contd.) SIDE EFFECTS 1. Metallic taste in the mouth 2. Gastrointestinal (anorexia, nausea, vomiting, diarrhea, abdominal discomfort) 3. Vitamin B 12 deficiency (prolonged use) 4. Lactic acidosis ( rare – 01/ 30,000-exclusive in renal failure) (they ↑anerobic glycolysis ↑lactic acid) this phenomenon is treated with NaHCO3. 43 BIGUANIDES (Contd.) CONTRAINDICATIONS 1. Hepatic impairment 2. Heart failure In these situations the body is more sensitive to lactic acidosis 3. Renal impairment 4. Alcoholism 44 BIGUANIDES (Contd.) INDICATIONS 1. Obese patients with type II diabetes 2. Alone or in combination with sulfonylureas or meglitinides. 45 α-GLUCOSIDASE INHIBITORS e.g. Acarbose PKs: • Given orally. • Not absorbed from intestine except small amount (hence, no systemic effect). • t1/2 3 - 7 hr. • Excreted with stool. 46 α-GLUCOSIDASE INHIBITORS (Contd.) MECHANISM OF ACTION They inhibit α glucosidase Disaccharides will not be converted to monosacchari de With the use of drugs, there is no sharp rise in blood sugar (مايشطح السكر )بعد األكل Delay absorption of glucose ↓post prandial increase in blood glucose They delay the absorption but don’t inhibit it 47 α-GLUCOSIDASE INHIBITORS (Contd.) It is a competitive inhibitor of glucosidase enzyme (has more affinity than sugar ). It used as supportive not as treatment . Also can be used in border line patients. It can be use with type I DM but not alone. 48 α-GLUCOSIDASE INHIBITORS (Contd.) SIDE EFFECTS • Flatulence sugar fermentation • Loose stool or diarrhea results in gas formation • Abdominal pain • Alone does not cause hypoglycemia 49 α-GLUCOSIDASE INHIBITORS (Contd.) INDICATIONS Patients with Type II inadequately controlled by diet with or without other agents( SU, Metformin) Can be combined with insulin to reduce postprandial hyperglycemia Maybe helpful in obese Type II patients (similar to metformin) α-GLUCOSIDASE INHIBITORS can also be used with type I DM with meals. 50 THIAZOLIDINEDIONE DERIVATIVES e.g.: Pioglitazone PKs: 99% absorbed Metabolized by liver 99% of drug binds to plasma proteins T1/2 = 3 – 4 h Eliminated via the urine 64% and feces 23% 51 THIAZOLIDINEDIONE DERIVATIVES (Contd.) MECHANISM OF ACTION - Increase target tissue sensitivity to insulin by: reducing hepatic glucose output & increase glucose uptake & oxidation in muscles & adipose tissues. They do not cause hypoglycemia (similar to metformin and acarbose ) . 52 THIAZOLIDINEDIONE DERIVATIVES (Contd.) ADVERSE EFFECTS - Mild to moderate edema - Weight gain - Headache - Myalgia (muscle pain) - Hepatotoxicity ? Thus a liver function test is done before giving this drug. - Congestive heart failure? - Alone does not cause hypoglycemia. 53 THIAZOLIDINEDIONE DERIVATIVES (Contd.) INDICATIONS Type II diabetes alone or in combination with metformin , sulfonylurea or insulin in patients resistant to insulin treatment. 54 Dipeptidyl peptidase-4 inhibitors (DPP- 4 inhibitors) e.g. Sitagliptin, vildagliptin Mechanism of action Dipeptidyl pepidase (enzyme) DPP-4 inhibitors inactivate incretin 55 Clinical uses Used in type II DM as an adjunct to diet & exercise as a monotherapy or in combination with other antidiabetic drugs. Is also used in borderline patients. Adverse effects Nausea, abdominal pain, diarrhea Nasopharyngitis 56 57 If you have developed – Tachyphylaxis – from studying Pharma! then we recommend you to take some rest!!!!! Thank You! 58