* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download A. Thyroids Hormones
Survey
Document related concepts
Transcript
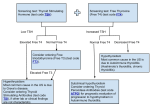
A. Thyroids Hormones Iodide : actively transported into the thyroid follicular cell -> Thyroid peroxide (TPO) oxidizes iodide near the cell-colloid surface & Incorporates it into tyrosyl residues within the thyroglobulin molecule result in the formation of monoiodotyrosine (MIT) & diiodotyrosine (DIT) Triiodothyronine (T3) & Thyroxine (T4) formed by secondary coupling of MIT & DIT catalyzed by TPO • TPO : membrane-bound, heme-containing oligomer, localized in rourg ER, Golgi vesicle & follicular cell surface • Thyroid antimicrosomal antibodies found in patients with autoimmune thyroid disease are directed against the TPO enzyme • Thyroid-stimulating hormone (TSH) : regulates thyroidal iodine metabolism by activation of adenylate cyclase --> facilitates endocytosis, digestion of thyroglobulincontaining colloid & release of thyroid hormones T4, T3, rT3 • Thyroid hormones - effects on cells include increased oxygen consumption, heat production, increased metabolism of fat, proteins & carbohydrate 1. Iodide Metabolism - Daily allowance : 150 ~ 300 g/day - Sufficiency of iodine : associated with development of autoimmune thyroid disorder. 2. Factors affecting Thyroid function - Iodide - Pollutants (plasticizers, polychlorinated bipheols & coal processing pollutants) - Ab to Yersinia enterocolitica. - Female hormonal milieu & its potential effects on immune surveillance B. Evaluation 1. Thyroid Function. ↑TBG conditions : pregnancy, oral pill, ERT, hepatitis, genetic abnormality of TBG, --> require measuring T3RU for clarification. FTI ( Free T4 Index ) : % free T4 ( T3RU ) × T4 total TSH measurement : best single screen for thyroid dysfunction. 2. Immunologic Abnormalities -Antithyroglobuliin Ab. : noncomplement-fixing IgG polyclonal antibodies, (+) in Hashimoto's thyroiditis, Graves' Dz, acute thyroiditis, nontoxic goiter, thyroid cancer, normal women. -Antimicrosomal antibody-direct against TPO : cytotoxic, complement fixing Ig G Ab (+) in Hashimoto's thyroiditis, Graves' disease & postpartum thyroiditis -Atibody to T3 & T4. : (+) in Hashimoto's thyroiditis & Graves' Dz. who have antithyroglobulin Antibody -Antibody to TSH receptor -TSAb. (Thyroid-stimulating Ab) or TSI (Thyroid stimulating Ig) : monoclonal or limited polyclonal --> mimic TSH action -TBII (TSH-binding Inhibitor Ig) -block TSH binding -block both pre-& postreceptor process -TGI (Thyroid Growth-promoting Ig) • - stimulate growth, but not hormone release. C. Autoimmune Thyroid Disease -Hypothyroidism > hyperthyroidism -F>M -Other autoimmune conditions associated with Graves' Dz. : Hashimoto's thyroiditis, Addison's Dz, ovarian failure, RA, Sjoren's SD, IDDM, vitiligo, pernicious anemia, MG, ITP... 1. Hashimoto's thyroiditis - Chronic lymphocytic thyroiditis - Present as hyperthyroidism, hypothyroidism, euthyroid goiter, or diffuse goiter. - High levels of anti-microsomal & antithyroglobulin Ab (+) - The composition of various Ab (TBII, TGI etc.) result in varied physical finding - Autoantibody TBII : causing the atophic form & congenital hypothyroidism in some neonates. TGI : causing the goitrous variety - 3 Classic types of autoimmune injury complement-mediated cytotoxicity Ab dependant cell mediated cytotoxicity stimulation or blockade of hormone receptor 1) Clinical Characteristics & Dx. - Mostly, relatively asymptomatic with painless goiter & hypothyroidism - Symptom : Cold intolerance, constipation, carotene deposition in the periorbital region, carpal tunnel syndrome, dry skin, fatigue, hair loss, lethargy, wt.gain. c.f Hashitoxicosis (<-- represent a variant of Graves' Dz.) - in 4~8% -Diagnosis ↑ TSH level during routine screening ↑ serum antithyroglobulin & antimicrosomal Ab ↑ ESR 2) Treatment Symptomatic hypothyroidism T4 replacement Goiter Can’t regress the size but prevent further growth of size Pregnant women with↑ TSH level L-thyroxine. :Can’t slow progression of the disease 6wks of Tx are necessary before the effect of the dose change 2. Reproductive effects of Hypothyroidism . - Hypothyroidism : a/w↓ fertility resulting from ovulatory difficulties and not spontaneous abortion. - Menorrhagia, amenorrhea, anovulation, luteal phase defect - TSH increase defective in Dopamine turnover Enhanced sensitivity of prolactin secreting cell hyperprolactinemia - Replacement therapy - reverse the hyperprolactinemia & correct ovulatory defect 3. Graves' Disease Heritable specific defect by suppressor T cell development of helper T cell react to thyroid antigen induce B-cell mediated response Result in the clinical feature of Graves’ dz HLA class II antigen DR, DP, DQ, DS can present antigen to T cell 1) Clinical Characteristics & Dx. Classical triad : Exophthalmos, goiter, & hyperthyroidism symptom :↑bowel movement, heat intolerance, irritability, nervousness, palpitation, tachycardia, tremor, wt.loss, lower external swelling. P/E : lidlag, nontender thyroid enlargement, onycholysis, palmar erythema, proptosis, staring gaze, thick skin... if. severe cases : acropachy, chemosis, clubbing, dermopathy, exophalmus with ophthalmoplegia, follicular conjunctivitis, pretibial myxedema, vision loss. Diagnosis T3 ↑, but T4 levels - mostly normal TSH↓ Antimicrosomal Ab (+) TSAb : useful in evaluating medical treatment, prognosis & potential fetal complication.. 2) Treatment Medication --> potentially harmful effects on the fetus, special attention must be given to the case of contraception & the potential for pregnancy. (1) 131I Ablation Effective care in about 80% of cases Most commonly utilized definitive Tx. in nonpregnant women Postablative hypothyroidism : 50% within 1st year. (2) Antithyroid Drugs (3) Surgery (4) β-blocker * Antithyroid Drugs 1. PTU & Methimazole Low doses : block the secondary coupling Rx. that form T3 & T4 from DIT & MIT. Higher doses --> block iodination of tyrosyl residues in thyroglobulin. 30% --> remission. 2. PTU (100mg, every 8 ~ 24hr) - block the intrathyroid synthesis of T3 & the pph conversion of T4 to T3. - not cross placenta. - drug of choice in pregnancy. 3. Methimazole (10mg, every 8 ~ 24hr) - not drug of choice in pregnancy , d/t not block pph conversion & cross placenta. 4. Iodide & Lithium. - reduce thyroid hormone release & inhibit the organification of iodine. * Surgery Subtotal thyroidectomy Ix. Medical Tx failed Hypersensitive to medical Tx. Risk Hypoparathyroidism Recurrent laryngeal n. paralysis Hypothyroidism. 4. Reproductive Effects of Hyperthyroidism • Most women. : ovulatory & fertile • Severe thyrotoxicosis : wt. loss, irregular mens, amenorrhea, ↑spontaneous abortion, ↑congenital anomalies. 5. Postpartum Thyroid Dysfunction • Often difficult to diagnose, • Sx. appear 1 ~ 8 months postpartum. • Incidence : 5 % -> 25% permanent hypothyroid • Histo : lymphocytic infiltration & inflammation. • Antimicrosomal Ab (+) 1) Clinical Characteristics & Dx. Symptom : Depression, fatigue, palpitation, at 6 ~ 12 wks. postpartum. c.f. postpartum thyroid dysfunction should be considered in all women with postpartum psychosis. Diagnosis : (-) of thyroid tenderness, pain, fever, ↑ESR, leucocytosis TSH, T4, T, T3RU, antimicrosomal Ab titer. 2) Treatment : mostly hypothyroid phase and require 6 ~ 12 months of T4 replacement if they are symptomatic. (c.f.. 10 ~ 30% --> permanent hypothyroidism) : rarely hyperthyroid phase : not routinely use of anti-thyroid medication, but propranolol for symptomatic relief.