* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ANTIHYPERLIPIDAEMIC DRUGS
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Toxicodynamics wikipedia , lookup
Plateau principle wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
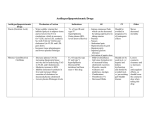
ANTIHYPERLIPIDAEMIC DRUGS BY DR/AZZA BARAKA Learning objectives Classify the antihyperlipidemic drugs. Explain the mechanism of action of drugs used in treatment of hypercholesterolemia & hypertriglyceridemia. Deduce the different antihyperlipidemic drugs in treatment of combined hyperlipidemia. Tabulate the difference between the different antihyperlipidemic drugs as regards; mechanism of action, side effects & therapeutic uses. Lipids originate from two sources: endogenous lipids, synthesized in the liver, and exogenous lipids, ingested and processed in the intestine. Dietary cholesterol and triglycerides are packaged into chylomicrons in the intestine, before passing into the bloodstream via lymphatics. Chylomicrons are broken down by lipoprotein lipase (LPL) in the capillaries of muscle and adipose tissue to fatty acids, which then enter the cells. The chylomicron remnants, which have lost much of their triglyceride content, are taken up by the liver for disposal. The liver synthesizes triglycerides and cholesterol, and packages them as VLDLs before releasing them into the blood. When VLDLs (which consist mainly of triglyceride) reach muscle and adipose blood vessels, their triglycerides are hydrolyzed by LPL to fatty acids. The fatty acids that are released are taken up by the surrounding muscle and adipose cells. During this process, the VLDLs become progressively more dense and turn into LDLs. While most of the resulting LDLs are taken up by the liver for disposal, some circulate and distribute cholesterol to the rest of the body tissues. HDLs, which are also secreted from the liver and intestine, have the task of preventing lipid accumulation. They remove surplus cholesterol from tissues and transfer it to LDLs that return it to the liver HYPERLIPIDEMIA Elevated concentrations of lipid (hyperlipidemia) can lead to the development of atherosclerosis and CAD. VLDLs and LDLs are atherogenic lipoproteins, whereas HDL concentrations are inversely related to the incidence of CAD. Hence, treatments for hyperlipidemia aim to reduce LDL levels and raise HDL levels. High density lipoprotiens Act as a reservoir for apoproteins which can be donated or received from other lipoproteins. Also play a vital role in scavenging “used” cholesterol (reverse cholesterol transport): apoproteins HDL HDL HDL receptor mediated endocytosis by liver HDL Liver “used” cholesterol transferred to HDL and converted to cholesterol ester Peripheral tissues LDL some cholesterol ester transferred to circulating VLDL VLDL LDLreceptor mediated endocytosis LDL Cholesterol can be converted to bile salts for excretion or repackaged in VLDL for redistribution Pharmacotherapeutic options in hyperlipidemia I-Agents targeting endogenous cholesterol: a-Statins. b-Fibrates. C-Nicotinic acid. II-Agents Targeting Exogenous Cholesterol a-Cholesterol Uptake Inhibitors, e.g. ezetemibe. b- Bile acid binding resins, e.g. colestipol & cholestyramine H M G – COA REDUCTASE INHIBITORS(STATINS) Lovastatin , fluvastatin , pravastatin , simvastatin ,atorvastatin and rosuvastatin. Pharmacokinetics: They are subjected to extensive first-pass metabolism by the liver. Greater than 95% of most of these drugs are bound to plasma proteins. All statins are taken orally at bedtime because of diurnal rhythm of cholesterol synthesis, except atorvastatin taken at any time because of its long half-life (14 hours). Mechanism of action These are potent reversible competitive inhibitors of 3-hydroxy 3-methyl glutaryl coenzyme A reductase, the rate-controlling enzyme in cholesterol biosynthesis. They are extremely effective in lowering plasma concentration of LDL-C. They act by inhibiting cholesterol synthesis in the liver, so they deplete the intracellular supply of cholesterol, which in turn triggers a compensatory up-regulation of hepatic LDL receptors, thus, causing increased clearance of plasma LDL . Pharmacological actions Effect on LDL-C: Statins decrease LDL-C by two mechanisms: Up-regulation of LDL-R with increase of clearance of LDL-C and decrease LDL-C. Decrease of very low density lipoprotein (VLDL) production because cholesterol is a required component of VLDL which is a precursor of LDL-C Effect on VLDL: Decreased VLDL production mediated by decreased C, a required component of VLDL. Effect on HDL-C: Statins induce modest increase in HDL-C, this might be due to the ability of statins to reduce plasma CETP activity (mediates the transfer of cholesteryl esters from HDL to apoB-containing lipoproteins in exchange for triglycerides). Adverse effects Hepatotoxicity (increased serum transaminase). Myopathy (increased creatine kinase) especially when combined with: 1. 2. other lipid lowering drugs: i)Fibrates. ii) Niacin. other drugs that are metabolized by 3A4 isoform of cytochrome P450 e.g.: erythromycin, cyclosporine, verapamil, ketoconazole. G.I.T upset. 4. Headache. N.B :liver transaminases and CK must be regularly measured during therapy with statins 3. Contraindications Pregnancy & lactation (Cholesterol is important for normal development, and it is possible that statins could cause serious problems). The effects of high cholesterol do not cause problems for many years or even decades. Therefore, if a woman does not take her statin or other cholesterol medications during breastfeeding, it will likely have only a minimal impact on her long-term risks. Therefore, it is best to wait until you have weaned your child before starting or resuming a statin medication 2. Active liver diseases. N.B. The American Academy of Pediatrics is recommending that kids as young as 8 years old be given cholesterol drugs in hope of preventing future heart disease. 1. Drug interactions Potentiate the action of oral anticoagulant and antidiabetic drugs (displacement from plasma protein binding sites). N.B. : Pravastatin and fluvastatin are the statins of choice to be given to a patient taking other drugs metabolized by cytochrome 3A4 system. FIBRIC ACID DERIVATIVE (Fibrates) Preparations: Gemfibrozil , fenofibrate , clofibrate . Mechanism of action: Ligand for the nuclear transcription regulator, peroxisome proliferatoractivated receptor-α (PPAR- α) in the liver, heart, kidney, & skeletal muscle. N.B The PPAR-a are a class of intracellular receptors that modulate fat metabolism. It is through PPAR-a that fibrates lead to: Increased LPL activity, which increases clearance of VLDL & chylomicron in plasma. Increased FFA uptake by the liver. Decreased VLDL due to increased fatty acid metabolism( beta oxidation), by inducing Acyl-coenzymeA synthetases , which is a crucial enzyme that facilitate the uptake and permit the metabolism of fatty acids. Increased LDL-C uptake by the liver. Raises HDL cholesterol levels (by increasing Apo A-I and II expression in hepatocytes). Increase excretion of hepatic cholesterol in bile , thus endogenous hepatic cholesterol synthesis may be decreased. PPARs PPARs functions as a ligand-activated transcription factor. Upon binding to hypolipidemic drugs, PPARs are activated. They then bind to peroxisome proliferator response elements, which are localized in numerous gene promoters. In particular, PPARs regulates the expression of genes encoding for proteins involved in lipoprotein structure and function. Several such genes have been identified, including those of apoC-III, apoA-I, apoA-II, apoA-IV, acyl coenzyme A oxidase, and possibly that of lipoprotein lipase. The transcriptional downregulation of apoC-III and the upregulation of lipoprotein lipase by fibrates enhance both the intravascular lipolysis of TG-rich lipoproteins as well as their tissue catabolism via apoE-mediated binding to specific cellular receptors. Adverse effects G.I.T upset,rash, urticaria Myopathy Since fibrates increase the cholesterol content of bile, they increase the risk for gallstones. Drug interactions Increased risk of myopathy when combined with statins. 2. Displace drugs from plasma proteins( e.g. oral anticoagulants and oral hypoglycemic drugs). Contraindications: 1- Patients with impaired renal functions. 2- Pregnant or nursing women. 3-Preexisting gall bladder disease. 1. NICOTINIC ACID(NIACIN) Mechanism of action: In adipose tissue: it binds to adipose nicotinic acid receptors, this will lead to decrease in free fatty acids mobilization from adipocytes to the liver resulting in TG and thus VLDL synthesis. 2. In liver: niacin inhibits hepatocyte diacylglycerol acyltransferase-2, a key enzyme for TG synthesis. Thus, it decreases VLDL production (decreased TG synthesis and estrification). 1. In plasma: it increases LPL activity that increases clearance of VLDL & chylomicron. 1. 2. Niacin also promotes hepatic apoA-I production and slows hepatic clearance of apoA-I and HDL through as-yet unknown mechanisms. Pharmacological actions Effect on VLDL: Decreased VLDL by: 1) decreased synthesis in liver; 2) increased clearance in plasma. 3) Decreasd mobilaization of free fatty acids from adipose tissue. Effect on LDL: Decreased LDL due to reduction in its precursor (VLDL). Effect on HDL: Induces modest increase in HDL-C (The catabolism of HDL can be inhibited by nicotinic acid through a mechanism that is largely unknown). Niacin also promotes hepatic apoA-I production and slows hepatic clearance of apoA-I and HDL through as-yet unknown mechanisms. Therapeutic Uses Niacin is the most effective medication for increasing HDL cholesterol levels and it has positive effects on the complete lipid profile. It is useful for patients with mixed dyslipidemias. Niacin appears to exert the greatest beneficial effects on the widest range of lipoprotein abnormalities Adverse effects 1. 2. 3. 4. 5. Pruritus, flushing The niacin flush results from the stimulation of prostaglandins D(2) and E(2) by subcutaneous Langerhans cells via the niacin receptor. This flush is avoided by low dose aspirin 325 mg ½ h before niacin. Reactivation of peptic ulcer (because it stimulates histamine release resulting in increased gastric motility and acid production . Hepatotoxicity. Hyperglycemia which is believed to be caused by an increase in insulin resistance. Increased uric acid level (due to decreased uric acid excretion). Contraindications 1. 2. 3. 4. Gout. Peptic ulcer. Hepatotoxicity. Diabetes mellitus. Ezetimibe Mechanism of action: - Impairs dietary and biliary cholesterol absorption at the brush border of the intestines without affecting fat-soluble vitamins. - Reducing the pool of cholesterol absorbed from the diet results in a reduced pool of cholesterol available to the liver. -The liver in turn will upregulate the LDL receptor, trapping more LDL particles from the blood and result in a fall in measured LDL cholesterol . Adapted from van Heek M et al Br J Pharmacol 2000;129:1748-1754. Pharmacokinetics Elimination half-life of approximately 22 hours Long half-life: 1. Permits once-daily dosing 2. May improve compliance ezetimibe BILE ACID BINDING RESINS(BAS) E.g. colestipol ,cholestyramine and Colesevelam Mechanism of action: 1- When resins are given orally, they are not absorbed, they bind to bile acids in the intestinal lumen, prevent their reabsorption and increase their excretion, thus interrupt the enterohepatic circulation of bile acids. 2-Since bile acids inhibit the enzyme that catalysis the rate limiting step in the conversion of cholesterol to bile acids, their removal results in increased breakdown of hepatic cholesterol. 3-However, a compensatory increase occurs in the rate of biosynthesis of cholesterol which is insufficient to compensate for the increased catabolism and up-regulation of LDL-R on hepatocytes thus the plasma and tissue cholesterol levels decrease. 4-In addition, since bile acids are required for intestinal absorption of cholesterol, these resins decrease cholesterol absorption from the G.I.T. Pharmacological actions Effect on LDL-C: It decreases cholesterol content of hepatocytes leading to upregulation of LDL-receptors with increased LDL-cholesterol clearance from blood and decreased LDL-cholesterol level. Effect on VLDL: It produces transient increase in TG level in normal subjects which return to base line. In borderline patient (e.g. TG >250 mg/dl), it produces marked increase in TG, which is dangerous. Effect on HDL-C: Increased HDL-C Side effects Constipation ,G.I.T complaints: heart burn, flatulence, dyspepsia. 2. Large doses may impair absorption of fats or fat soluble vitamins (A, D, E, and K) and other medications, particularly warfarin and statins, that are given concurrently. N.B. Patients on multiple drug regimens should be counseled to administer other medications one hour before or four hours after the BAS. Colesevelam has not been shown to interfere with the absorption of coadministered medications and is a better choice for patients on multiple drug regimens 1. May ↑ level of VLDL in border line patients. 2. Chronic use of cholestyramine resin may be associated with increased bleeding tendency due to hypoprothrombinemia associated with Vitamin K deficiency. 1. Contraindications 1- Complete biliary obstruction( BECAUSE BILE IS NOT secreted into the intestine). 2- Chronic constipation. 3-Severe hypertriglyceridemia(TG >400 mg/dL) Antihyperlipedemic combinations 1. 2. 3. 4. 5. Indications: Increased VLDL during treatment of hypercholesterolemia with resins. Combined increase in LDL & VLDL. High LDL or VLDL not normalized with a single drug. Severe hypertriglycerdemia or hypercholesterolemia. To take lower doses of each drug. Resin & Niacin: In combined hyperlipidemia. Advantages: No additional side effects. Resin decrease gastric irritation of niacin. May be given concomitantly. Resin & statin: (synergistic combination) why? Because adding statins block the compensatory increase that occurs in the rate of biosynthesis of cholesterol induced by resins. Statin & ezetimibe: (synergistic combination) why? Because statin blocks synthesis of endogenous cholesterol while ezetimibe blocks exogenous cholesterol. Niacin & Statins: -In severe LDL elevation. -In combined hyperlipidemia Statins & Fibrates: Contraindicated (in full dose) because the incidence of myopathy may increase so, use not more than ¼ maximum dose of statin and use pravastatin .