* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 21 Antimicrobial medications
Plateau principle wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Discovery and development of tubulin inhibitors wikipedia , lookup
Orphan drug wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
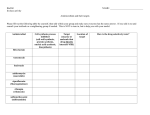
Chapter 21 Antimicrobial medications Biology 261 Prof. Santos Medgar Evers College • Chemotherapeutic- a chemical used to treat a disease • Antimicrobial drug- a chemical used to treat microbial infections History and development • 1- Paul Ehrlich developed Salvarsan to treat syphilis in laboratory animals. Discovery of Antibiotics • In 1928, Alexander Fleming discovered that the fungi Penicillium produces a chemical that kills bacteria. He called this substance penicillin. Features of Antimicrobial drugs 1- Made naturally by certain microorganisms. Many come from microorganisms that normally reside in soil. 2- Commercially they can be made in large numbers in a laboratory. 3- In a lab, they can be modified to alter their chemical and physical characteristics. • Antibiotics that have been chemically altered are called semi-synthetic. 4- selective toxicity • Useful antimicrobial drugs cause greater harm to microorganisms than to the human host. They do this by interfering with essential biological structures or pathways that are common in microorganisms but not humans. Therapeutic index • The toxicity of a given drug is expressed as its therapeutic index. • A high therapeutic index means that the drug is less toxic to a patient because the drug acts on a biochemical process of bacteria that is not found on humans. • A drug with a low therapeutic index must be carefully monitored in the patient’s blood to ensure toxic levels are not reach. 5- antimicrobial action Those drugs that inhibit bacterial growth are called bacterio-static. These drugs depend on the host’s natural immune system to clear the pathogen from the body. Sulfonamides, erythromycin, and tetracyclines are examples of bacteriostatic drugs. Antibiotics that actually kill bacteria are bacteriocidal. Those drugs that kill bacteria are called bactericidal. 6- Antimicrobial drugs that affect a wide range of bacteria are called broad spectrum antimicrobials. These are important during life threatening acute infections when there is no time to culture and identify the agent of disease. 7- Antimicrobials that affect a limited range of bacteria are called narrow-spectrum antimicrobials. 8- Combining drugs to fight infection must be carefully monitored. 3 situations to know! A- antagonistic when one drug interferes with the action of another. B- synergistic when one drug enhances the effectiveness of another drug C- Additive When the effect is neither antagonistic or synergistic 9- half-life • The rate of elimination of a drug in the body after it has been metabolize. The half life is the time required for the body to eliminate one half of the original concentration in the serum. • *Half life determines the size of dosage and frequency of the dosage. 10- Adverse effects Adverse effects include allergic reactions to medications, toxic effects, and the suppression of the normal flora. 11- Resistance to antimicrobial agents include innate resistance (inherited) and acquired through a mutation. **members of the genus Mycoplasma lack a cell wall so penicillin does not affect it. Mechanisms of action of antimicrobial drugs 1- inhibit cell wall synthesis 2- inhibit protein synthesis 3- inhibit nucleic acid synthesis 4- inhibit metabolic pathways 5- inhibit cell membrane integrity 6- special drugs used against Mycobacterium tuberculosis Cell wall synthesis • Antimicrobial drugs that inhibit cell wall synthesis include the penicillins, cephalosporins, and other beta lactam drugs. • The beta lactam drugs include penicillin, cephalosporin, monobactam, and carbapenem. • They all share a chemical structure called a beta lactam ring. • The beta lactam drugs competitively inhibit a group of enzymes that catalyze formation of peptide bridges between adjacent glycan strands in the final stages of peptidoglycan formation. Antibacterial Drugs That Inhibit Cell Wall Synthesis • Penicillins, Cephalosporins, other β-Lactam Drugs (cont…) – Interfere with peptidoglycan β-lactam drugs Vancomycin Competitively inhibit enzymes Binds to the amino acid side synthesis that help form peptide bridges chain of NAM molecules, between adjacent glycan blocking peptidoglycan chains. synthesis. – Weaken cell walls, leads to cell lysis Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Peptidoglycan (cell wall) Cytoplasmic membrane NAG NAM Bacitracin Interferes with the transport of peptidoglycan precursors across the cytoplasmic membrane. • Antibacterial Drugs That Inhibit Cell Wall Synthesis – Bacterial cell walls are unique, contain peptidoglycan • Great target for drugs: often have high therapeutic index • Penicillins, Cephalosporins, other β-Lactam Drugs – All have β-Lactam ring – Competitively inhibit enzymes that catalyze formation of peptide bridges between adjacent glycan strands; disrupt cell wall synthesis – Called penicillin-binding proteins (PBPs) since bind penicillin – Only effective against actively growing cells Antibacterial Drugs That Inhibit Cell Wall Synthesis Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Basic Structure Side Chain C • C CH2 The penicillins share basic structure – Side chain modified to create derivatives – Five general groups of penicillins • Natural are from Penicillium chrysogenum – Narrow-spectrum, act against Gram-positives and a few Gram-negatives • Penicillinase-resistant developed in response to S. aureus strains – Some now able to produce altered PBPs to which βlactam drugs do not bind (e.g., methicillin-resistant S. aureus, or MRSA) S NH CH C CH N O CH3 C CH3 COOH C H β-lactam ring Penicillin G OCH2 Penicillin V (acid-resistant) OCH3 Methicillin (penicillinase-resistant) OCH3 CI N CI O Dicloxacillin (acid- and penicillinase-resistant) CH3 Ampicillin (broad-spectrum and acid-resistant) CH NH2 HO Amoxicillin (like ampicillin but more active and requiring less frequent doses) CH NH2 CH S COONa CH NH C O O N N O C2 H5 Ticarcillin (more activity against Gramnegative rods, including Pseudomonas, but not as effective against some Gram-positive organisms) Piperacillin (like ticarcillin but a broader spectrum of activity) Antibacterial Drugs That Inhibit Cell Wall Synthesis Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Basic Structure Side Chain C • C CH2 The penicillins share basic structure – Side chain modified to create derivatives • Broad-spectrum act against Gram-positives and Gramnegatives due to modified side chain – Inactivated by many β-lactamases • Extended-spectrum have greater activity against Pseudomonas species – Reduced activity against Gram-positives; destroyed by many β-lactamases • Penicillins + β-lactamase inhibitor includes inhibitor to protect penicillin S NH CH C CH N O CH3 C CH3 COOH C H β-lactam ring Penicillin G OCH2 Penicillin V (acid-resistant) OCH3 Methicillin (penicillinase-resistant) OCH3 CI N CI O Dicloxacillin (acid- and penicillinase-resistant) CH3 Ampicillin (broad-spectrum and acid-resistant) CH NH2 HO Amoxicillin (like ampicillin but more active and requiring less frequent doses) CH NH2 CH S COONa CH NH C O O N N O C2 H5 Ticarcillin (more activity against Gramnegative rods, including Pseudomonas, but not as effective against some Gram-positive organisms) Piperacillin (like ticarcillin but a broader spectrum of activity) The cephalosporins • Contain the beta lactam ring! • Are grouped into 1st, 2nd, 3rd ,and 4th generation cephalosporins. • They include cephalexin, cephradine, ceflacor, cefibuten, and cefipime. Other b- lactam antibiotics • The carbapenems and monobactams are very resistant to lactamases. • Carbapenems are effective against both gram + and gram – bacteria. They include imipenem and meropenem. • The only monobactam used therapeutically is aztreonam. It is effective against species of the Enterobacteriaceae family. Vancomycin • Binds to the terminal amino acids of the peptide chain of NAM molecules that are being assembled to form glycan chains. By doing so it blocks the production of peptidoglycan. They do not cross the outer membrane of gram – bacteria so they are resistant. Vancomycin must be administered intravenously. Bacitracin • These drugs interfere with cell wall biosynthesis by interfering with the transport of precursors across the cytoplasmic membrane. • They are only used as topical ointments due to their toxicity. Inhibiting protein synthesis – All cells synthesize proteins – Can exploit differences between prokaryotic and eukaryotic ribosomes • Prokaryotes have 70S, eukaryotes have 80S ribosomes • Mitochondria also have 70S ribosomes Macrolides Prevent the continuation – May account for Streptogramins of protein synthesis. Each interferes with a some toxicity distinct step of protein Chloramphenicol synthesis. Prevents peptide of these drugs bonds from being Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Lincosamides Prevent the continuation of protein synthesis. formed. 50S 30S Tetracyclines and glycylcyclines Block the attachment of tRNA to the ribosome. Oxazolidinones Interfere with the initiation of protein synthesis. Aminoglycosides Block the initiation of translation and cause the misreading of mRNA. Drugs against nucleic acid synthesis 1- the fluoroquinolones inhibit the enzyme topoisomerase which helps maintain DNA in a supercoil state. 2- the Rifamycins block prokaryotic RNA Polymerase from initiating transcription. Drugs against metabolic pathways 1- sulfonamides block the action of an enzyme that normally binds to PABA, a substrate in the folate pathway. They closely resemble PABA, so the enzyme binds to it and the entire pathway is blocked. 2- trimethoprim These drugs inhibit the bacterial enzyme that catalyzes a metabolic step following the one inhibited by sulfonamides. Drugs that interfere with cell membrane integrity 1- polymyxin alters the permeability of the cell membrane leading to leakage and cell damage. 2-Daptomycin inserts into the membrane leading to cell damage and eventually death. Special medications against Mycobacterium 1- first line drug such as Isoniazid inhibits the synthesis of mycolic acid, an important component of the cell wall. 2- Ethambutol inhibits enzymes used to synthesize other cell wall components. 3- Rifampin, an antimicrobial drug used to block the process of transcription by blocking RNA Polymerase. 4- Ampicillin, a broad spectrum penicillin.