* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Levofloxacin wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
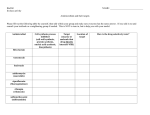
Protein Synthesis lnhibitors Ján Mojžiš Department of Pharmacology LF UPJŠ Košice PROTEIN SYNTHESIS INHIBITORS TETRACYCLINES Tetracycline, Doxycycline, Minocycline AMINOGLYCOSIDES Amikacin, Gentamicin, Neomycin, Netilmicin Streptomycin, Tobramycin MACROLIDES Erythromycin, Azithromycin, Clarithromycin CHLORAMPHENICOL CLINDAMYCIN LINEZOLID TETRACYCLINES CHLORTETRACYCLINE, OXYTETRACYCLINE, TETRACYCLINE, DEMECLOCYCLINE, METHACYCLINE, DOXYCYCLINE, MINOCYCLINE Mechanism of action They bind reversibly to the 30S subunit of the bacterial ribosome, thereby blocking access of the amino acyl-tRNA to the mRNAribosome complex at the acceptor site. Thus, bacterial protein synthesis is inhibited. Bacteriostatic Antibacterial spectrum Pharmacology 1. Absorption: - adequately but incompletely absorbed after p.o. - dairy foods in the diet decrease absorption because of the formation of nonabsorbable chelates of the tetracyclines with calcium ions. 2. Distribution: - concentration in the liver, kidney, spleen, and skin - bind to tissues undergoing calcification (e.g.,teeth, bones), or to tumors that have a high calcium content (e.g. gastric carcinoma). - penetration into body fluids is adequate. -CSF – only MINOCYCLINE enters the brain in the absence of inflammation -all TTCs cross the placental barrier and concentrate in fetal bones E. Adverse effects gastric discomfort: Epigastric distress commonly results from irritation of the gastric mucosa. This can be controlled if the drug is taken with foods oher than dairy products. effects on calcified tissues: Deposition in the bone and primary teeth occurs in growing children »»» discoloration and hypoplasia of the teeth Use in pregnancy and in children younger than 8 years (or before the second dentition) should be avoided !!! hepatotoxicity superinfections: these infections may occur with candida (e.g. in the vagina) or with resistant staphylococci in the intestine. Pseudomembranous colitis due to an overgrowth of Clostridium difficile was also reported. dysmicrobia, hypovitaminosis B and K AMINOGLYCOSIDES - mainstays of treatment of serious infections due to gram-negative bacilli. -use is limited by the occurrence of serious toxicities A. Mode of action - inhibit bacterial protein synthesis - they irreversibly bind to the 30S ribosomal subunit + misread the genetic code – production of „bad“ proteins . -they synergize with beta-Iactam ATBs (enhance diffusion of aminoglycosides into the cell). -all AMG are bactericidal Antibacterial spectrum Bactericidal, effective only against aerobic organisms Commonly used aminoglycosides: AMIKACIN, GENTAMICIN, TOBRAMYCIN and STREPTOMYCIN Further aminoglycosides: NEOMYCIN, NETILMICIN, KANAMYCIN D. Pharmacology Administration - parenterally AMG penetrate most body fluids well except for the CSF - may be administered intrathecally accumulation in the renal cortex and in the endolymph and perilymph of the inner ear »»» nephrotoxicity and ototoxicity Adverse effects The elderly are more susceptible to nephrotoxicity and ototoxicity !! Patients with myasthenia gravis are particularly at risk. MACROLIDE ANTIBIOTIC ERYTHROMYCIN, AZITHROMYCIN, CLARITHROMYCIN ERYTHROMYCIN - few indications where it is a drug of first choice, mostly as an alternative to penicillin in allergy to beta-lactam ATBs. Mechanism of action - inhibits protein synthesis by reversibly binding to the 50S ribosomal subunit - generally bacteriostatic (may be –cidal - depending on the concentration and on the type of microorganisms). Antibacterial spectrum D. Pharmacology ERY inhibits CYP-450 system Adverse effects LlNEZOLID New ATB; against resistant G+ organisms (e.g., methicillin- and vancomycin-resistant S. aureus, vancomycin-resistant Enterococcus faecium and Enterococcus faecalis, and PNCresistant streptococci). A. Mechanism of action Inhibition of bacterial protein synthesis by inhibiting the formation of the 70S initiation complex. It binds to a site on the 50S subunit near the interface with the 30S subunit. C. Antibacterial spectrum - primarily against G+ organisms (e.g., staphylococci, streptococci, and enterococci, as well as Corynebacterium species and Listeria monocytogenes) - its main clinical use. - moderately active against Mycobacterium tuberculosis. - bacteriostatic (cidal against the streptococci and C. perfringens). D. Pharmacokinetics Completely absorbed after oral administration; . I.v. is also available. - widely distributed in the body. -two metabolites -- one has antimicrobial activity. - excretion - renal and nonrenal routes. E. Adverse effects Well-tolerated. - GIT upset, nausea, and diarrhea - headache and rash -thrombocytopenia in cca 2 % (when longer than 2 weeks) reversible. - considered as a choice of last resort where every other antibiotic therapy has failed CHLORAMPHENICOL Adverse effects Anemia: Hemolytic anemia in patients with low levels of G6-PD Other types of anemia - include reversible anemia (is dose-related and occurs concomitantly with therapy) and aplastic anemia, which is idiosyncratic and usually fatal !!! Bone marow supression Potential teratogenic effects Gray baby syndrome LINCOSAMIDES CLINDAMYCIN Action - as that of erythromycin. Spectrum - Treatment of infections caused by anaerobic bacteria (e.g. Bacteroides fragilis). Also active against non-enterococcal, gram-positive cocci. Pharmacology Given orally (well absorbed) or parenterally; Distributes well into all body fluids except the CSF Adverse effects - skin rashes, GIT disturbances, impaired liver function - the most serious adverse effect is potentially fatal pseudomembranous colitis QUINOLONES FIRST GENERATION Nalidixic acid FLUOROQUINOLONES SECOND GENERATION Ciprofloxacin, Norfloxacin Ofloxacin THIRD GENERATION Gatifloxacin, Levofloxacin Moxifloxacin, Sparfloxacin FOURTH GENERATION Trovafloxacin FLUOROQUINOLONES Old drug, NALIDIXIC ACID and NORFLOXACIN - used mainly for recurrent urinary tract infections (UTIs). Newer fluorinated quinolones - greater potency, broader spectrum of antimicrobial activity, systemic effects. New compounds - more active against G+ organisms, yet retain favorable activity against G- microorganisms. A. Mechanism of action - they enter the bacterium by passive diffusion via water channels. - inhibit bacterial topoisomerases which are necessary for DNA synthesis DNA gyrase (TOPO II) – primary target for GTopoisomerase IV - primary target for G+ Since DNA gyrase is a bacteriospecific target for antimicrobial therapy, cross-resistance with other antimicrobial drugs is rare, but this is increasing in the case of multidrug-resistant organisms. Bactericidal Antimicrobial spectrum C. Examples of clinically useful fluoroquinolones Ciprofloxacin - frequently used. F. Adverse reactions - well tolerated Connective tissue problems: They should be avoided in pregnancy, in nursing mothers, and in children under 18 years - because articular cartilage erosion (arthropathy) SULFONAMIDES (SA) Structurally related to p-aminobenzoic acid (PABA). Seldom use alone. The introduction of trimethoprim in combination with sulfamethoxazole led to a renewed interest in sulfonamides. The SA inhibit the synthesis of folic acid. A. Mechanism of action Folic acid - synthesized from PABA, pteridine, and glutamate. - SA - analogs of PABA - SA compete with PABA for the bacterial enzyme, dihydropteroate synthetase – inhibition of the synthesis of bacterial FA. All sulfa drugs are bacteriostatic. B. Antibacterial spectrum -selected enterobacteriaceae, chlamydia, and nocardia. - SULFADIAZINE + pyrimethamine (dihydrofolate reductase inhibitor) is the preferred form of treatment for toxoplasmosis and chloroquine-resistant malaria. Individual sulfonamides: 1) Well absorbed orally, short-acting: Sulfadiazine, Sulfadimidine, Sulfisoxazole, Sulfamethoxazole 2) Well absorbed orally, long-acting: Sulfamethopyrazine 3) Poorly absorbed in GIT: Sulfasalazine 4) Used topically: Silver sulfadiazine E. Adverse effects Adequate hydration and alkalization of urine is necessary and prevent the crystalluria. Note: It is contraindicated to use acidic drugs (salicylates) or food (oranges etc.) which may lead to acidic pH of urine during therapy with sulfonamides !!! TRIMETHOPRIM inhibitor of bacterial dihydrofolate reductase; antibacterial spectrum similar to SA. Mostly compounded with sulfamethoxazole = co-trimoxazole. A. Mechanism of action The active form of folate - tetrahydroderivative (formed by reduction of dihydrofolate by dihydrofolate reductase). This enzymatic reaction is inhibited by trimethoprim - decreased availability of the tetrahydrofolate coenzymes required for purine, pyrimidine, and amino acid synthesis. Action of trimethoprim - much stronger for the bacterial reductase than for the mammalian enzyme CO-TRIMOXAZOLE Trimethoprim – mostly compounded with sulfamethoxazole. Sequential Blockade dTMP E. Adverse effects Dermatological: Reactions involving the skin are very common and may be severe in the elderly. GIT: Nausea, vomiting, glossitis, stomatitis - not unusual. Hematological: Megaloblastic anemia, leukopenia, thrombocytopenia - may be reserved by administration of FA. Hemolytic anemia - in patients with G6-PD Immunocompromised patients with pneumocystis pneumonia frequently drug-induced fever, rashes, diarrhea, and/or pancytopenia. Antibiotic use in orofacial dental infection MICROBIOLOGY • Most oral infections are mixed in origin consisting of aerobic and anaerobic gram positive and gram negative organisms • Anaerobes predominant (75%) Common Pathogens Necrotic pulp and apical abscesses Obligate anaerobic bacteria Gram negative rods Prevotella & porphyomonas spp. Fusobacterium spp. Campylobacter rectus Gram positive rods Eubacterium spp. Actinomycetes spp. Gram positive cocci Peptostreptococcus spp. Facultative anaerobic bacteria Gram positive cocci Strep and Entercoccus spp. Common Pathogens • Periodontal Diseases Gingivitis Fuso, strep, & actinomycetes Adult peritonitis Bacteroides, porphyomonas, peptostreptococcus & prevotella Acute necrotizing ulcerative gingivitis Spirochetes, prevotella, fuso Localized juvenile periodontitis Actinobacillus Common Pathogens • Fungal Infections Candida spp. Mucorales spp. COMMONLY USED ATB Penicillins • First choice for odontogenic infection • G+ cocci and rod, spirochetes, anaerobes • 0.7~10% hypersensitivity • Nature: penicillin G (IV), penicillin V (PO) • Penicillinase-resistant: oxacillin, dicloxacillin • Extended spectrum: ampicillin, amoxicillin • Combine β-lactamase inhibitor: augmentin Cephalosporins • More resistance to penicillinase • G+ cocci, many G- rods • Third generation: P. aeruginosa Clindamycin • G+ cocci • Bacteriostatic (bactericidal) • Second-line drug: should be held in reserve to treat those infections caused by anaerobes resistant to other antibiotics Aminoglycosides • G- aerobes, some G+ aerobes eg S. aureus • Poorly absorbed from GI tract • Adjustment of dosage in renal dysfunction • Drugs: Gentamicin, Amikacin • Combined with penicillin or cephalosporin Metronidazole • Only for obligate anaerobes • Can cross blood-brain barrier • To treat serious infections caused by anaerobic bacteria, combined with β-lactam ATB • Effective against Bacteroides species, esp. in periodontal infections • Avoid pregnant women Vancomycin • G+, most anaerobes, some G- cocci (Neisseria) • Given i.v. - BP should be monitored • Adjustment of dosage in renal dysfunction Erythromycin • G+ cocci, oral anaerobes • Bacteriostatic • Second choice for odontogenic infections • Indication for out-patients with mild infection • Drug resistence: 50% of S. aureus, Strep. viridans, Tetracycline • Only against anaerobes • Contraindications: pregnant women, children <12 • Limited usefulness in orofacial infection • Use as adjunctive therapy for refractory periodontitis • Most likely to cause superinfection Chloramphenicol • Wide spectrum, highly active against anaerobes • Limited to severe odontogenic infection threatening to the eye or brain • Severe toxicity • Empiric antibiotics in oral and maxillofacial infection ■ First-line Penicillin 3MU IV q6h -> Cefazolin 1000mg q6h Gentamycin 60-80mg IV q8h-q12h ■ Second line Amoxicillin + clavulanic a.1200mg q8h + amikacin 375mg q12h + metronidazole ■ Mild infection Amoxicillin 250mg PO q8h Clindamycin 300mg PO q6h Antifungals • Nystatin – MOA: inhibit cell wall synthesis – P.o.; topical – GI upset Antifungals • ketoconazole, fluconazole – MOA: inhibit cell wall synthesis – Drug interactions: major p-450 enzyme inhibitor, interactions with many drugs • ketoconazole - rare GI problems, skin intolerance