* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture
Biochemical cascade wikipedia , lookup
Cell culture wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Embryonic stem cell wikipedia , lookup
Microbial cooperation wikipedia , lookup
Hematopoietic stem cell wikipedia , lookup
FNA Mapping wikipedia , lookup
State switching wikipedia , lookup
Sperm competition wikipedia , lookup
Cell theory wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Somatic cell nuclear transfer wikipedia , lookup
Regeneration in humans wikipedia , lookup
Drosophila melanogaster wikipedia , lookup
Chimera (genetics) wikipedia , lookup
Fertilisation wikipedia , lookup
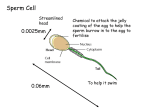
Lecture Reproduction & Development Sex in the animal kingdom • both sexual and asexual • sexual – fusion of haploid gametes to form a diploid zygote – gametes – egg and sperm – zygote can itself give rise to gametes via meiosis – zygote develops into an embryo via mitosis • asexual – generation of a new individual without the fusion of gametes – relies upon mitotic division Asexual reproduction • mechanisms: • 1. fission – separation of the parent into two equal sized individuals • 2. budding – new individuals arise as outgrowths from the parent • 3. fragmentation & regeneration – breaking of the body into several pieces • 4. parthenogenesis – egg develops without being fertilized – progeny is either haploid or diploid Sexual reproduction • sexual reproduction must enhance reproductive success • if not successful – it would not have evolved because asexual reproduction produces more individuals • advantages of sex? – diversity due to recombination of parental genes during meiosis and fertilization • sexual reproduction is advantageous when environmental conditions change rapidly and frequently Reproductive Cycles • most animals’ reproductive cycles coincide with the change of seasons – give birth when resources are plentiful and conditions favor the survival of their offspring • ovulation – mid-point in the reproductive cycle corresponding to the release of eggs • reproductive cycles not just restricted to animals who reproduce sexually • asexual reproduction cycles – some fishes, amphibians and reptiles can undergo periods of parthenogenesis – double their chromosome number to produce diploid offspring • reproductive cycles found in animals that have sexual and asexual cycles Mammalian Reproductive Cycles – most females undergo estrus = time during which the female is behaviorally and physiologically receptive to the male (fertile egg is produced) • complex series of hormonal changes that affect egg production, uterine and vaginal environments and sperm production – many mammals are monoestrus • • • • • only once a year strictly regulated by the environment e.g. wild dogs, bears and sea lions e.g. domestic dogs – biestrus other animals have cycles that can repeat on a cyclical basis – e.g. rats – every 4 to 6 days Hermaphrodism • happens when finding a sexual partner is difficult • rather common in sessile, aquatic animals and in parasites • both male and female reproductive organs (monoecious) • this means any two individuals can mate – one acts as a male, one acts as a female • some can self-fertilize Fertilization • union of egg and sperm • can either be: external or internal • external fertilization requires a moist habitat – prevents dessication of gametes – also allows the sperm to swim to the egg – clustering of animals in the same area for fertilization = spawning – when not synchronized within a population – mating pairs will undergo courtship behaviors to stimulate release of gametes – e.g. frogs – external fertilization with courtship behavior – locates breeding sites and potential mates Internal Fertilization • sperm deposited in or near the female reproductive tract – male copulatory organ deposits sperm – female can have a seminal receptacle for receipt and storage of sperm – then delivers it to the egg when needed – e.g. sharks – modified pelvic fins called claspers that are inserted into the female cloaca for sperm transfer • followed by internal fertilization – thus ensuring success • some sharks are viviparous – give birth to live young • fertilization occurs within the female’s reproductive tract – usually followed by internal embryonic development • • • • evolved because of dry, terrestrial habitats requires cooperative behavior requires compatible reproductive structures fewer gametes produced vs. external fertilization because the chances of successful fertilization are higher • mammalian fertilization: – in a few mammals – fertilization is delayed after coitus (delayed fertilization) • e.g. bats – coitus in fall, fertilization in spring – most mammals have direct fertilization after coitus • but development of the embryo can be arrested for one to two weeks = embryonic diapause • e.g. sea lions, bears and marsupials • may be due to presence of resources – allows mother time to feed before having to nurse • also allows young to be born during a time of good resources Care of Offspring • internal fertilization and gestation ensures better protection of offspring – against desiccation and physical damage • internal gestation done by placental mammals = eutherians – receive nourishment from the mother through the placenta • internal gestation for long periods of time is not necessary – marsupials – embryos crawl out of the uterus and complete development attached to a mammary gland located in a pouch Care of Offspring • alternative to internal gestation and development: development of the amniotic egg – egg laying animals – monotremes – birds and reptiles – protection of the developing embryo by a protective layer of calcium and proteins in the form of the shell – eggs of fish and amphibians are quite different – surrounded by a gelatinous material and they lack internal membranes Gamete production • gametes = egg and sperm • develop from a set of precursor cells called germ cells – develop during embryonic development and remain dormant until sexual maturity • e.g. humans • typical site for these germ cells and gamete production are the gonads – not required in simpler animals • more complex reproductive systems also have accessory organs in association with the gonads – seminal vesicles, prostate gland – seminal receptacles or spermathecae (in insects) Reproductive adaptations • same basic plan for all vertebrates • in many non-mammalian vertebrates – formation of a cloaca – combined opening for digestive, urinary and reproductive tracts – female mammals have separate openings for all three – male mammals combine the urinary and reproductive opening • many vertebrates have a uterus that is divided into two chambers • in mammals that produce only a few offspring at a time – uterus is a single structure • differences in the male reproductive system – in the copulatory organs – human penis is quite distinct from other mammals Male reproductive system • three accessory organs – seminal vesicle – prostate – bulbourethral glands (Cowper glands) • reproductive ducts – epididymus – vas deferens (ductus deferens) – urethra Reproductive Ducts -vas deferens: conducting tube from testis to urethra -epididymus – connection between the testis and the vas deferens -stores immature sperm -vas deferens + blood vessels + nerve = spermatic cord (passes through inguinal canal) -urethra: 3 sections: A. prostatic - runs through prostate B. membranous - between prostate and penis C. spongy - through penis • • • • • • • • • Reproductive glands seminal vesicles, prostate, bulbourethral glands -produce fluid that combine with sperm to make semen -semen: alkaline, activates sperm cells 1. prostate: surrounds the urethra -secretes a thin, milky fluid that enhances sperm motility and neutralizes vaginal fluid 2. seminal vesicles: connect to urethra via the ejaculatory ducts -secretes an alkaline fluid that contains sugars and prostaglandins (stimulates uterine contractions) 3. bulbourethral glands: 2 glands behind the prostate -secrete a fluid that lubricates the penis Bladder Rectum Prostate Prostatic Urethra Membranous Urethra Spongy/ Penile Urethra Testes Corpus spongiosum Corpus cavernosum Glans Penis External • scrotum = supportive structure for the testes • hangs from the root of the penis • externally- single pouch separated at the midline by a raphe • internally – divided by a scrotal septum into two sacs each containing 1 testis • the scrotum contains two muscles – dartos muscle (smooth muscle) & the cremaster muscle – skeletal muscle that is a continuation of the internal oblique pampiniform plexus Vas deferens testicular artery testicular artery branches Epididymus Seminiferous Tubules Tunica Albuginea Tunica Vaginalis -testis: develop internally near the kidneys and descend during the latter half of the seventh month gestation -covered by two protective membranes: 1. tunica vaginalis –derived from the peritoneum 2. tunica albuginea – internal to the TV -extends inward to divide the testes into lobules (200-300) -each lobule contains 1 to 3 coiled seminiferous tubules for sperm production - lined with spermatogenic cells that produce sperm -contain sperm stem cells = spermatogonium -testis: also contain two additional cell types: -Sertoli cells = sustenacular cells -found in the seminiferous tubule -secretion of growth factors that mediate spermatogenesis -interstitial cells – located between the seminiferous tubules -for testosterone production • • • • • • • • • sperm development – from sperm stem cells called spermatogonium these spermatogonium develop in the embryonic testes the spermatogonium remain dormant in the testes until puberty mature sperm cells = spermatozoa 1. differentiation of the spermatogonium into primary spermatocytes (2n) 2. start of meiosis 3. formation of secondary spermatocytes (n) – 23 chromosomes comprised of two chromatids 4. completion of meiosis and formation of four spermatids (23 chromosomes each made up of one chromatid) 5. spermiogenesis – development of spermatids into a sperm cell (head, acrosome and flagella development) Spermatogenesis Sperm • 300 million made each day • 60 um long • major parts – 1. head: contains the nucleus with 23 highly condensed chromosomes (one chromatid) – 2. acrosome: covers the anterior 2/3 of the head • contains digestive enzymes to dissolve the protective barriers of the egg (hyaluronidase and proteases) – 3. tail or flagellum • neck - constricted region just behind the head • iddle piece – contains mitochondria arranged in a spiral • principal piece – longest portion of the tail • end piece – terminal portion of the tail principal piece end piece made up of a: 1. root 2. body (or shaft) 3. glans -conveys urine and semen -body is found externally, root is found internally (attached to the pubic ramus) -body is comprised of two tissue types: erectile tissue surrounded by connective tissue A. corpus cavernosum – larger spaces B. corpus spongiosum - smaller spaces & surrounds the urethra -corpus spongiosum enlargens at the tip - glans penis (sensory receptors) -glans penis covered with a loose fold of skin = prepuce -release of Gonadotropic releasing hormone (GnRH) from the hypothalamus which stimulates the anterior pituitary gland -anterior pituitary releases two gonadotropins (FSH and LH) 1. Follicle stimulating hormone - stimulates spermatogenesis 2. Leutinizing hormone - stimulates male hormone production -male hormones: androgens (e.g. testosterone) -testosterone: secondary sex characteristics, reproductive organ development and maintenance -rise in testosterone causes a negative feedback: hypothalamus release of GnRH is inhibited -uterus: receives and nourishes the embryo -comprised of a body, a curved portion (fundus) and the cervix -uterine wall outer perimetrium, muscular myometrium and inner endometrium -endometrium: mucosal layer covered with epithelium -rich blood supply, sloughed off during menstruation -comprised of a deeper basal layer and an outer functional layer Fundus Fornix Body Cervix Bladder Rectum Vaginal canal Urethra Labia minora Labia majora External urethral orifice Vaginal orifice -uterine tubes or oviducts (Fallopian tubes): conduction of egg from ovary to uterus -expands at end near the ovary = infundibulum with fimbrae (fingers) for the “catching” of the released egg -fertilization occurs in the uterine tubes -cervix: projects into the vaginal canal -vaginal canal broadens to surround the cervix – fornix -site for the insertion of the penis and deposition of sperm -opens at the exterior as the vulva (female external genitalia) -known as the vulva -mons pubis – mass of adipose tissue that lays on top of the pubic bone -mons pubis divides into the labia majora and minora -labia majora: folds of adipose tissue that enclose and protect the labia minora -labia minora: surrounds the external urethral orifice and the vaginal orifice -clitoris: erectile tissue with a glans, body and a root -ovary: production of oocytes -inner medulla and outer cortex -medulla - connective tissue with blood & lymphatic vessels and nerves -cortex - granular tissue due to the presence of tiny ovarian follicles containing egg stem cells (oogonium) -ovarian follicles mature and contain the developing oocyte = oogenesis 1. growth of primary follicles into secondary follicles containing a primary oocyte 2. secondary follicle matures -> vesicular /tertiary follicle with a large secondary oocyte (for ovulation) 3. ruptured follicle degenerates into a corpus hemorrhagicum and then into a corpus luteum female sex hormone production (estrogen & progesterone) • early fetal development – primordial germ cells in the developing ovaries differentiate to form oogonia (egg stem cells) • at birth: meiosis in the oogonia results in the development of primary follicles containing primary oocytes – stops at prophase I of meiosis • at puberty - release of FSH and LH each month causes the development of a primary oocyte into a secondary oocyte followed by ovulation • coincides with the development of the primary follicle (primary oocyte) into a secondary follicle (primary oocyte) and finally into a tertiary follicle (secondary oocyte) • tertiary follicle – ovulation of secondary oocyte • fertilization is required for the completion of meiosis II • therefore during oogenesis, ONE oocyte merges with the sperm and THREE polar bodies form Oogenesis -GnRH causes release of FSH and LH from anterior pituitary -FSH causes maturation of follicles -LH results in development of corpus luteum -corpus luteum produces and releases estrogen and progesterone -estrogen and progesterone: regulate pregnancy, menstruation, secondary sex characteristics & development of sex organs at puberty -divided into two cycles 1. uterine cycle 2. ovarian cycle -Ovarian cycle: -rise in FSH matures the follicle - day 9 - follicle begins to produce follicular estrogen -day 14 - sudden increase in FSH and LH plus follicular estrogen coincides with ovulation -the increase in follicular estrogen is what causes the spike in LH -day 14 - ovulation = LH spike is the trigger -Ovarian cycle: -drop in LH, FSH and follicular estrogen after ovulation -but FSH will begin to climb at the end of the cycle because of an increase in GnRH release from the hypothalamus Uterine cycle: -menstrual cycle initiated by increased FSH at Day 1 -rise in follicular estrogen starts thickening of uterine lining = known as the proliferative phase -following ovulation and the development of the corpus luteum = increased secretion of luteal estrogens + synthesis of progesterone -increased progesterone results in thickening of the stratum functionalis = known as the secretory phase -Uterine cycle: -estrogen and progesterone begin to drop about day 25 to 28 - disintegration of the stratum functionalis -Menstruation (3 to 7 days) Fertilization -fertilization in the upper third of the oviduct/fallopian tube -fertilization = union of egg and sperm to produce the zygote -sperm must undergo capacitation after ejaculation – increase rate of tail beating -happens in the female reproductive system -plasma membrane of the ovulated secondary oocyte is surrounded by an extracellular matrix (glycoproteins) = zona pellucida and a ring of follicular cells = corona radiata (for nourishment in the follicle) -sperm must penetrate these layers before docking onto the plasma membrane 1. several sperm penetrate corona radiata and enter zona pellucida 2. Sperm bind to the zona pellucida & trigger release of acrosomal contents zonal digestion 3. ONE sperm contacts the plasma membrane of the oocyte 4. changes to the zona pellucida result (hardens) – blocks polyspermy 5. entry of sperm nucleus into egg 6. fusion of the sperm’s pronucleus with the pronucleus of the egg = zygote embryonic stage: 1st week to week 8 -first cell division – within 24 hrs & takes 6 hrs to complete -second day – four cells -end of third day – 16 cells -fourth day – morula stage -fourth to fifth day – blastocyst stage -end of fifth day – hatching of blastocyst from zona pellucida -6th day – implantation of blastocyst into enodmetrium OVIDUCT: -union of sperm and egg nuclei (zygote) -> first cell division within 24 hours to form the embryo - cell division continues -> formation of the morula at day 4 - morula = a mass of tiny, uniformly sized cells with equal amounts of cytoplasm - cells of the embryo = blastomeres embryonic stage: 1st week to week 8 -first cell division – within 24 hrs & takes 6 hrs to complete -second day – four cells -end of third day – 16 cells -fourth day – morula stage -fourth to fifth day – blastocyst stage UTERUS: -day 4 – 5: morula forms a blastocyst (blastula) = assymetrical ball of cells with a cavity called a blastocoel -day 6: -> implantation of blastocyst into the stratum functionalis of the endometrium -blastula = blastocyst - hollow ball of cells/blastomeres -outer layer = trophoblast - forms extraembryonic tissues (e.g. placenta, yolk sac) -inner mass of cells at one end = totipotent embryonic stem cells -second week of development (day 7 – 14) : -amniotic cavity forms between the inner cell mass and the trophoblast -the inner cell mass flattens = embryonic disc Gastrulation • third week of gestation in humans (days 14 – 21) • prior to gastrulation – the embryo is composed of an upper and lower layer that form an embryonic disk Fertilized egg Primitive streak Embryo Yolk – the epiblast and hypoblast – epiblast = embryo – hypoblast (‘roof’ of the yolk sac) = supports embryology & forms part of the yolk sac Primitive streak Epiblast Future ectoderm Blastocoel Migrating cells (mesoderm) Endoderm Hypoblast YOLK Gastrulation • during gastrulation - epiblast cells move toward the midline of the blastoderm – toward a structure called the primitive streak • epiblast cells migrate through the primitive streak toward the yolk – some cells push the hypoblast to the side to become the endoderm – those remaining cells mesoderm – leftover non-migrating epiblast cells ectoderm Fertilized egg Primitive streak Embryo Yolk Primitive streak Epiblast Future ectoderm • animals with three germ layers are known as Triploblastic Blastocoel Migrating cells (mesoderm) Endoderm Hypoblast YOLK -three germ layers: 1. ectoderm integumentary system & nervous system 2. mesoderm mesenchyme which forms the bones, fat, cartilage, blood, muscle of the animal 3. endoderm digestive organs and their linings Endometrial epithelium (uterine lining) 1 Blastocyst reaches uterus. Uterus Inner cell mass Trophoblast Blastocoel 2 Blastocyst implants (7 days after fertilization). Expanding region of trophoblast Maternal blood vessel Epiblast Hypoblast Trophoblast 3 Extraembryonic membranes start to form (10–11 days), and gastrulation begins (13 days). Amniotic cavity Epiblast Hypoblast Yolk sac (from hypoblast) Chorion (from trophoblast) 4 Gastrulation has produced a three-layered embryo with four extraembryonic membranes. Amnion Chorion Ectoderm Mesoderm Endoderm Yolk sac yolk sac chorion amnion placenta -yolk sac: forms blood cells, gives rise to sex cells and the stem cells of the immune system -portion of it becomes part of the umbilical cord -embryo’s first connection is via a connecting stalk -allantois: tube from the yolk sac that projects into the connecting stalk - gives rise to the umbilical artery and vein yolk sac placenta amnion chorion -chorion – forms four weeks after implantation as slender projections that grow out from the trophoblast = chorionic villi (becomes the placenta) -produces human chorionic gondadotropin hormone – hormone of pregnancy -amnion – surrounds the amniotic cavity (amnionic fluid + developing embryo) -amnion enfolds the connecting stalk and remnants of the yolk sac to form the umbilical cord -fifth week (days 28 – 35): formation of lens, beginnings of maxilla and mandible & paddle-shaped forelimb -embryo is 10-12 mm long -35 + 2 days: formation of eye, ear, forebrain, nasal pit, tail -35 + 5 days: formation of midbrain, heart, external ear, primitive fingers -sixth week: formation of primitive toes (22-24 mm) -seventh week: formation of eyelids, webbed fingers -eighth week: separation of toes and fingers (34-40 mm) -fetal stage : end of the eighth week -> birth -third month: body lengthens and head growth slows -ossification of bones -fourth month: reproductive organs appear -rapid body growth -lower limbs lengthen -development of hair, eyebrows, lashes, nipples -fifth month: growth slows -skeletal muscles are active -fetus curls into fetal position -sixth to ninth month: weight gain -skin smoothens as fat is deposited beneath skin -eyelids open -organs elaborate and grow (digestive and respiratory are last) -neuronal networks form