* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 01 FlexArt
Survey
Document related concepts
Transcript
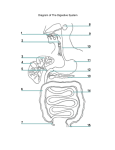
Fig. 16.1 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Pharynx (throat) Oral cavity (mouth) Salivary glands Esophagus Stomach Pancreas Liver Gallbladder Appendix Rectum Anus Small intestine Large intestine Fig. 16.22 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Food Carbohydrates Monosaccharides Lipids Fatty acids Monoglycerides Proteins Amino acids Fig. 16.23 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Carbohydrates Lipids Proteins Mouth (salivary glands) Salivary amylase Polysaccharides, Disaccharides Stomach Pepsin Polypeptides Duodenum (pancreas, liver) Bile salts (liver) Pancreatic amylase Lipase (pancreas) Trypsin, chymotrypsin, carboxypeptidase (pancreas) Disaccharides Peptides Epithelium of small intestine Disaccharidases Peptidases Monosaccharides Fatty acids Monoglycerides Amino acids Fig. 16.1 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Pharynx (throat) Oral cavity (mouth) Salivary glands Esophagus Stomach Pancreas Liver Gallbladder Appendix Rectum Anus Small intestine Large intestine Fig. 16.2 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Blood vessels Enteric plexus Myenteric plexus Lymphatic vessel Submucosal plexus Nerve Gland in submucosa Mesentery Ducts from glands Lymphatic nodule Intestinal gland Mucosa (mucous membrane) Epithelium Lamina propria Muscularis mucosae Submucosa Muscularis Circular muscle layer Longitudinal muscle layer Serosa (serous membrane; visceral peritoneum) Connective tissue layer Simple squamous epithelium Table 7.2 Table 4.10b Fig. 16.9 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Digestive tract Bolus 1 1 A wave of smooth muscle relaxation moves ahead of the bolus, allowing the digestive tract to expand. 2 A wave of contraction of the smooth muscle behind the bolus propels it through the digestive tract. Wave of relaxation Bolus moves. 2 Wave of contraction Fig. 16.15 Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 A secretion introduced into the digestive tract or into food within the tract begins in one location. Secretion or food 1 2 Segments of the digestive tract alternate between contraction and relaxation. 2 3 Material (brown) in the intestine is spread out in both directions from the site of introduction. 3 4 4 The secretion or food is spread out in the digestive tract and becomes more diffuse (lighter color) through time. Contraction waves Contraction waves Fig. 16.2 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Blood vessels Enteric plexus Myenteric plexus Lymphatic vessel Submucosal plexus Nerve Gland in submucosa Mesentery Ducts from glands Lymphatic nodule Intestinal gland Mucosa (mucous membrane) Epithelium Lamina propria Muscularis mucosae Submucosa Muscularis Circular muscle layer Longitudinal muscle layer Serosa (serous membrane; visceral peritoneum) Connective tissue layer Simple squamous epithelium Fig. 16.4 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Upper lip Gingiva covering the maxillary alveolar process Hard palate Soft palate Uvula Cheek Tongue Molars Frenulum of the tongue Premolars Canine Openings of the submandibular ducts Gingiva covering the mandibular alveolar process Incisors Lower lip Fig. 16.7 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Parotid duct Buccinator muscle Mucous membrane (cut) Ducts of the sublingual gland Parotid gland Masseter muscle Sublingual gland Submandibular duct Submandibular gland Fig. 16.8-1 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Tongue Hard palate Soft palate 1 Bolus Oropharynx 1 During the voluntary phase, a bolus of food (yellow) is pushed by the tongue against the hard and soft palates and posteriorly toward the oropharynx (blue arrow indicates tongue movement; black arrow indicates movement of the bolus). Tan: bone; purple: cartilage; red: muscle. Fig. 16.8-2 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Tongue Hard palate Soft palate Nasopharynx 1 2 Bolus Soft palate Superior pharyngeal constrictor Middle pharyngeal constrictor Epiglottis Oropharynx Larynx Inferior pharyngeal constrictor Upper esophageal sphincter Esophagus 1 During the voluntary phase, a bolus of food (yellow) is pushed by the tongue against the hard and soft palates and posteriorly toward the oropharynx (blue arrow indicates tongue movement; black arrow indicates movement of the bolus). Tan: bone; purple: cartilage; red: muscle. 2 During the pharyngeal phase, the soft palate is elevated, closing off the nasopharynx. The pharynx and larynx are elevated (blue arrows indicate muscle movement; green arrow indicates elevation of the larynx). Fig. 16.8-3 Tongue Hard palate Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Soft palate Nasopharynx 1 Soft palate 2 Superior pharyngeal constrictor Middle pharyngeal constrictor Bolus Epiglottis Oropharynx Inferior pharyngeal constrictor Larynx Upper esophageal sphincter Esophagus 1 2 During the voluntary phase, a bolus of food (yellow) is pushed by the tongue against the hard and soft palates and posteriorly toward the oropharynx (blue arrow indicates tongue movement; black arrow indicates movement of the bolus). Tan: bone; purple: cartilage; red: muscle. During the pharyngeal phase, the soft palate is elevated, closing off the nasopharynx. The pharynx and larynx are elevated (blue arrows indicate muscle movement; green arrow indicates elevation of the larynx). 3 3 Epiglottis Superior pharyngeal constrictor Middle pharyngeal constrictor Vestibular fold Vocal fold 3 Successive constriction of the pharyngeal constrictors from superior to inferior (blue arrows) forces the bolus through the pharynx and into the esophagus. As this occurs, the vestibular and vocal folds expand medially to close the passage of the larynx. The epiglottis (green arrow) is bent down over the opening of the larynx largely by the force of the bolus pressing against it. Opening of larynx Fig. 16.8 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Tongue Hard palate Soft palate Nasopharynx 1 2 Soft palate Superior pharyngeal constrictor Middle pharyngeal constrictor Bolus Epiglottis Oropharynx Inferior pharyngeal constrictor Larynx Upper esophageal sphincter Esophagus 1 During the voluntary phase, a bolus of food (yellow) is pushed by the tongue against the hard and soft palates and posteriorly toward the oropharynx (blue arrow indicates tongue movement; black arrow indicates movement of the bolus). Tan: bone; purple: cartilage; red: muscle. 2 During the pharyngeal phase, the soft palate is elevated, closing off the nasopharynx. The pharynx and larynx are elevated (blue arrows indicate muscle movement; green arrow indicates elevation of the larynx). 3 3 Epiglottis Middle pharyngeal constrictor Superior pharyngeal constrictor Opening of larynx Vestibular fold Vocal fold 3 Successive constriction of the pharyngeal constrictors from superior to inferior (blue arrows) forces the bolus through the pharynx and into the esophagus. As this occurs, the vestibular and vocal folds expand medially to close the passage of the larynx. The epiglottis (green arrow) is bent down over the opening of the larynx largely by the force of the bolus pressing against it. Inferior pharyngeal constrictor Upper esophageal sphincter 4 Esophagus 4 As the inferior pharyngeal constrictor contracts, the upper esophageal sphincter relaxes (outwardly directed blue arrows), allowing the bolus to enter the esophagus. 5 Esophagus 5 During the esophageal phase, the bolus is moved by peristaltic contractions of the esophagus toward the stomach (inwardly directed blue arrows). Fig. 16.10 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Esophagus Fundus Location of lower esophageal sphincter Body Gastroesophageal opening Serosa Cardiac part Longitudinal muscle layer Circular muscle layer Muscularis Oblique muscle layer Pyloric part Pyloric sphincter Submucosa Pyloric orifice Mucosa Pyloric canal Pyloric antrum Duodenum Rugae Gastric pit Surface mucous cell Lamina propria Gastric glands Goblet cell Mucous neck cells Parietal cells Mucosa Gastric pit Surface mucous cell Mucous neck cell Chief cells Endocrine cells Submucosa Blood vessels Oblique muscle layer Muscularis Circular muscle layer Longitudinal muscle layer Connective tissue layer Simple squamous epithelium Serosa (visceral peritoneum) ©Victor Eroschenko LM 30x Copyright © McGraw-Hill Education. Permission required for reproduction or display. Fig. 16.11 Cephalic Phase 1 The taste, smell, or thought of food or tactile sensations of food in the mouth stimulate the medulla oblongata (green arrows). Taste, smell, or thought of food (chemoreceptors) 2 Vagus nerves carry parasympathetic action potentials to the stomach (pink arrow), where enteric plexus neurons are activated. 1 Tactile sensation in mouth Hypothalamus 3 Postganglionic neurons stimulate secretion by parietal and chief cells and stimulate gastrin and histamine secretion by endocrine cells. 4 Gastrin is carried through the circulation back to the stomach (purple arrow), where, along with histamine, it stimulates secretion. Medulla oblongata Secretions stimulated 4 Vagus nerves 2 3 (a) Histamine Gastrin Circulation Stomach Gastric Phase 1 Distention of the stomach stimulates mechanoreceptors (stretch receptors) and activates a parasympathetic reflex. Action potentials generated by the mechanoreceptors are carried by the vagus nerves to the medulla oblongata (green arrow). 2 The medulla oblongata increases action potentials in the vagus nerves that stimulate secretions by parietal and chief cells and stimulate gastrin and histamine secretion by endocrine cells (pink arrow). Vagus nerves Medulla oblongata 1 Secretions stimulated Secretions stimulated 3 Distention of the stomach also activates local reflexes that increase stomach secretions (orange arrow). 2 4 Distention 3 4 Gastrin is carried through the circulation back to the stomach (purple arrow), where, along with histamine, it stimulates secretion. Histamine Gastrin Circulation (b) Stomach Intestinal Phase 1 Chyme in the duodenum with a pH less than 2 or containing fat digestion products (lipids) inhibits gastric secretions by three mechanisms (2–4). 2 Chemoreceptors in the duodenum are stimulated by H+ (low pH) or lipids. Action potentials generated by the chemoreceptors are carried by the vagus nerves to the medulla oblongata (green arrow), where they inhibit parasympathetic action potentials (pink arrow), thereby decreasing gastric secretions. 3 Local reflexes activated by H+ or lipids also inhibit gastric secretion (orange arrows). 4 Secretin and cholecystokinin produced by the duodenum (brown arrows) decrease gastric secretions in the stomach. Vagus nerves Medulla oblongata Decreased gastric secretions Vagus nerves Secretions inhibited 4 2 1 pH <2 or lipids Local reflexes 3 Circulation (c) Secretin and cholecystokinin Fig. 16.12 Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 A mixing wave initiated in the body of the stomach progresses toward the pyloric sphincter (pink arrows directed inward). Esophagus Mixing wave 2 The more fluid part of the chyme is pushed toward the pyloric sphincter (blue arrows), whereas the more solid center of the chyme squeezes past the peristaltic constriction back toward the body of the stomach (orange arrow). Pyloric sphincter Chyme 1 Body of stomach Duodenum 2 3 Peristaltic waves (purple arrows) move in the same direction and in the same way as the mixing waves but are stronger. Pyloric region More fluid chyme 4 Again, the more fluid part of the chyme is pushed toward the pyloric region (blue arrows), whereas the more solid center of the chyme squeezes past the peristaltic constriction back toward the body of the stomach (orange arrow). 5 Peristaltic contractions force a few milliliters of the most fluid chyme through the pyloric opening into the duodenum (small red arrows). Most of the chyme, including the more solid portion, is forced back toward the body of the stomach for further mixing (yellow arrow). 3 4 5 More solid chyme Fig. 16.13 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Stomach Duodenum Ascending colon Jejunum Mesentery Ileocecal junction Ileum Cecum Appendix Fig. 16.14 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Villi Blood capillary network Lacteal Epithelium Circular folds Epithelium Intestinal gland Submucosa Circular muscle Longitudinal muscle Serosa (a) (b) Duodenal gland Top of circular fold Microvilli of epithelial cell surface Villus Epithelial cell Capillary (blood) Lacteal (lymph) (d) (c) Fig. 16.15 Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 A secretion introduced into the digestive tract or into food within the tract begins in one location. Secretion or food 1 2 Segments of the digestive tract alternate between contraction and relaxation. 2 3 Material (brown) in the intestine is spread out in both directions from the site of introduction. 3 4 4 The secretion or food is spread out in the digestive tract and becomes more diffuse (lighter color) through time. Contraction waves Contraction waves Fig. 16.9 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Digestive tract Bolus 1 1 A wave of smooth muscle relaxation moves ahead of the bolus, allowing the digestive tract to expand. 2 A wave of contraction of the smooth muscle behind the bolus propels it through the digestive tract. Wave of relaxation Bolus moves. 2 Wave of contraction Fig. 16.21 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Transverse colon Left colic flexure Right colic flexure Ascending colon Descending colon Ileum Teniae coli Ileocecal valve Cecum Sigmoid colon Appendix Rectum (a) Anal canal Internal anal sphincter External anal sphincter (b) ©CNRI/SPL/Science Source Fig. 16.16 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Inferior vena cava Right lobe Left lobe Falciform ligament Round ligament Liver Gallbladder (a) Gallbladder Quadrate lobe Right lobe Hepatic ducts Hepatic portal vein Hepatic artery Caudate lobe Left lobe Portal triad Lesser omentum Inferior vena cava (b) To hepatic vein and inferior vena cava Liver lobule Hepatic cords Central vein Hepatic phagocytic cells Bile canaliculi Hepatic duct Hepatic portal vein Hepatic artery Hepatocyte To common bile duct Hepatic sinusoid From aorta (c) From digestive tract Portal triad Fig. 13.19 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Inferior vena cava Hepatic veins Liver Gallbladder Cystic vein Hepatic portal vein Stomach Gastric veins Gastroomental veins Spleen Splenic vein with pancreatic branches Tail of pancreas Duodenum Head of pancreas Superior mesenteric vein Ascending colon Splenic vein Gastroomental veins Inferior mesenteric vein Descending colon Small intestine Appendix Fig. 16.17 Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 The hepatic ducts from the liver lobes combine to form the common hepatic duct. Liver Gallbladder Hepatic ducts 1 2 The common hepatic duct combines with the cystic duct from the gallbladder to form the common bile duct. Common hepatic duct Spleen Cystic duct Hepatic portalvein 2 Common bile duct 3 The common bile duct joins the pancreatic duct. Accessory pancreatic duct 4 4 The combined duct empties into the duodenum at the duodenal papilla. 5 Pancreatic secretions may also enter the duodenum through an accessory pancreatic duct, which also empties into the duodenum. 5 3 Duodenal papilla Duodenum (cutaway view) Pancreatic duct Pancreas Copyright © McGraw-Hill Education. Permission required for reproduction or display. Fig. 16.18 Brain 1 Vagus nerve stimulation (red arrow) causes the gallbladder to contract, thereby releasing bile into the duodenum. 2 Secretin, produced by the duodenum (purple arrows) and carried through the circulation to the liver, stimulates bile secretion by the liver (green arrows inside the liver). 1 Vagus nerves 3 Cholecystokinin, produced by the duodenum (pink arrows) and carried through the circulation to the gallbladder, stimulates the gallbladder to contract and the sphincters to relax, thereby releasing bile into the duodenum (green arrow outside the liver). 4 Bile salts also stimulate bile secretion. Over 90% of bile salts are reabsorbed in the ileum and returned to the liver (green arrows), where they stimulate additional secretion of bile salts. Bile Bile Liver Bile 2 Secretin Gallbladder Bile Stomach 3 Pancreas Circulation 4 Duodenum Fig. 16.17 Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 The hepatic ducts from the liver lobes combine to form the common hepatic duct. Liver Gallbladder Hepatic ducts 1 2 The common hepatic duct combines with the cystic duct from the gallbladder to form the common bile duct. Common hepatic duct Spleen Cystic duct Hepatic portalvein 2 Common bile duct 3 The common bile duct joins the pancreatic duct. Accessory pancreatic duct 4 4 The combined duct empties into the duodenum at the duodenal papilla. 5 Pancreatic secretions may also enter the duodenum through an accessory pancreatic duct, which also empties into the duodenum. 5 3 Duodenal papilla Duodenum (cutaway view) Pancreatic duct Pancreas Copyright © McGraw-Hill Education. Permission required for reproduction or display. Fig. 16.18 Brain 1 Vagus nerve stimulation (red arrow) causes the gallbladder to contract, thereby releasing bile into the duodenum. 2 Secretin, produced by the duodenum (purple arrows) and carried through the circulation to the liver, stimulates bile secretion by the liver (green arrows inside the liver). 1 Vagus nerves 3 Cholecystokinin, produced by the duodenum (pink arrows) and carried through the circulation to the gallbladder, stimulates the gallbladder to contract and the sphincters to relax, thereby releasing bile into the duodenum (green arrow outside the liver). 4 Bile salts also stimulate bile secretion. Over 90% of bile salts are reabsorbed in the ileum and returned to the liver (green arrows), where they stimulate additional secretion of bile salts. Bile Bile Liver Bile 2 Secretin Gallbladder Bile Stomach 3 Pancreas Circulation 4 Duodenum Fig. 16.19 Duodenum Copyright © McGraw-Hill Education. Permission required for reproduction or display. Jejunum Common bile duct Body of pancreas Accessory pancreatic duct Pancreatic duct Tail of pancreas Duodenal papilla Head of pancreas (a) Pancreatic islet Acini cells (secrete enzymes) Cells producing glucagon Cells producing insulin Vein (b) To pancreatic duct To bloodstream Fig. 16.20 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Brain Stomach Vagus nerves 1 Pancreatic juices 1 Parasympathetic stimulation from the vagus nerve (red arrow) causes the pancreas to release a secretion rich in digestive enzymes. 2 Secretin Cholecystokinin 3 Pancreas 2 Secretin (purple arrows), released from the duodenum, stimulates the pancreas to release a watery secretion, rich in bicarbonate ions. Duodenum Circulation Cholecystokinin Secretin 3 Cholecystokinin (pink arrows), released from the duodenum, causes the pancreas to release a secretion rich in digestive enzymes. Fig. 16.24 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Villus Intestinal epithelial cell Monosaccharide (glucose) transport Lacteal Capillary 1 Glucose is absorbed by symport with Na+ into intestinal epithelial cells. 2 Symport is driven by a sodium gradient established by a Na+–K+ pump. Glucose 3 1 4 3 Glucose moves out of the intestinal epithelial cells by facilitated diffusion. 4 Glucose enters the capillaries of the intestinal villi and is carried through the hepatic portal vein to the liver. Na+ Na+ ATP ADP + Na+ K 2 To liver Fig. 16.27 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Villus Amino acid transport Intestinal epithelial cell 1 Acidic and most neutral amino acids are absorbed by symport into intestinal epithelial cells. 2 Symport is driven by a sodium gradient established by a Na+–K+ pump. Lacteal Amino acid 3 Amino acids move out of intestinal epithelial cells. 4 Amino acids enter the capillaries of the intestinal villi and are carried through the hepatic portal vein to the liver. Capillary 3 1 Na+ Na+ ATP Na+ 4 ADP K+ 2 To liver Fig. 13.19 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Inferior vena cava Hepatic veins Liver Gallbladder Cystic vein Hepatic portal vein Stomach Gastric veins Gastroomental veins Spleen Splenic vein with pancreatic branches Tail of pancreas Duodenum Head of pancreas Superior mesenteric vein Ascending colon Splenic vein Gastroomental veins Inferior mesenteric vein Descending colon Small intestine Appendix Fig. 16.25 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Villus Lipid transport 1 Bile salts surround fatty acids and monoglycerides to form micelles. Capillary 2 Micelles attach to the plasma membranes of intestinal epithelial cells, and the fatty acids and monoglycerides pass by simple diffusion into the intestinal epithelial cells. 3 Within the intestinal epithelial cell, the fatty acids and monoglycerides are converted to triglycerides; proteins coat the triglycerides to form chylomicrons, which move out of the intestinal epithelial cells by exocytosis. Lacteal Intestinal epithelial cell Micelles contact epithelial cell membrane. Triglycerides 1 Protein coat 4 3 4 The chylomicrons enter the lacteals of the intestinal villi and are carried through the lymphatic system to the general circulation. Bile salt 2 Fatty acids and monoglycerides Simple diffusion Exocytosis Micelle Chylomicron Lymphatic system Fig. 14.1-1 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Tonsils Right lymphatic duct Cervical lymph node Thoracic duct Thymus Axillary lymph node Mammary plexus Subclavian veins Thoracic duct Spleen Lymphatic vessel (transports lymph) Bone marrow (a) Lacteals in intestinal wall Inguinal lymph node Fig. 16.28 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Ingestion (2 L) Salivary gland secretions (1 L) Gastric secretions (2 L) Pancreatic secretions (1.2 L) Bile (0.7 L) Small intestine secretions (2 L) 92% absorbed in the small intestine 6%–7% absorbed in the large intestine Ingestion or secretion 1% in feces (Water infeces = Ingested + Secreted – Absorbed) Absorption Fig. 16.21 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Transverse colon Left colic flexure Right colic flexure Ascending colon Descending colon Ileum Teniae coli Ileocecal valve Cecum Sigmoid colon Appendix Rectum (a) Anal canal Internal anal sphincter External anal sphincter (b) ©CNRI/SPL/Science Source Fig. 16.3 Copyright © McGraw-Hill Education. Permission required for reproduction or display. Liver Visceral peritoneum Lesser omentum Stomach Peritoneal cavity containing peritoneal fluid Pancreas (retroperitoneal) Kidney (retroperitoneal) Parietal peritoneum Duodenum (retroperitoneal) Greater omentum Transverse colon Omental bursa Mesentery proper Small intestine Urinary bladder (retroperitoneal) Rectum (retroperitoneal) Medial view