* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
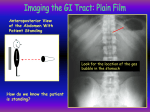
Chapter 24: The Digestive System Copyright 2009, John Wiley & Sons, Inc. 2 groups of organs compose the digestive system Gastrointenstinal (GI) tract or alimentary canal – mouth, most of pharynx, esophagus, stomach, small intestine, and large intestine Accessory digestive organs – teeth, tongue, salivary glands, liver, gallbladder, and pancreas Copyright 2009, John Wiley & Sons, Inc. Parotid gland (salivary gland) Submandibular gland (salivary gland) Mouth (oral cavity) contains teeth and tongue Sublingual gland (salivary gland) Pharynx Esophagus Liver Duodenum Gallbladder Jejunum Ascending colon Ileum Cecum Appendix Stomach Pancreas Transverse colon Descending colon Sigmoid colon Rectum Anal canal Anus (a) Right lateral view of head and neck and anterior view of trunk 6 functions of the digestive system 1. 2. 3. 4. Ingestion Secretion of water, acid, buffers, and enzymes into lumen Mixing and propulsion Digestion 5. 6. Mechanical digestion churns food Chemical digestion – hydrolysis Absorption – passing into blood or lymph Defecation – elimination of feces Copyright 2009, John Wiley & Sons, Inc. Layers of the GI tract Wall of GI tract from lower esophagus to anal canal has same basic 4 layers Mucosa – inner lining 1. Epithelium protection, secretion, absorption Lamina propria – connective tissue with blood and lymphatic vessels and mucosa-associated lymphatic tissue (MALT) Muscularis mucosae – thin layer of smooth muscle making folds to increase surface area Submucosa 2. Connective tissue binding mucosa to muscularis Contains many blood and lymphatic vessels Submucosal plexus Copyright 2009, John Wiley & Sons, Inc. Layers of the GI tract 3. Muscularis Voluntary skeletal muscle found in mouth, pharynx, upper 2/3 of esophagus, and anal sphincter Involuntary smooth muscle elsewhere 4. Arranged in inner circular fibers and outer longitudinal fibers Myenteric plexus between muscle layers Serosa Outermost covering of organs suspended in abdominopelvic cavity Also called visceral peritoneum Esophagus lacks serosa – has adventitia Copyright 2009, John Wiley & Sons, Inc. Duct of gland outside tract (such as pancreas) Submucosal plexus (plexus of Meissner) Gland in mucosa Mucosa-associated lymphatic tissue (MALT) Lumen Mesentery Vein Glands in submucosa Artery Nerve MUCOSA: Epithelium Lamina propria Muscularis mucosae Myenteric plexus (plexus of Auerbach) SUBMUCOSA MUSCULARIS: Circular muscle Longitudinal muscle SEROSA: Areolar connective tissue Epithelium Neural innervation Enteric nervous system (ENS) Intrinsic set of nerves - “brain of gut” Neurons extending from esophagus to anus 2 plexuses Myenteric plexus – GI tract motility Submucosal plexus – controlling secretions Autonomic nervous system Extrinsic set of nerves Parasympathetic stimulation increases secretion and activity by stimulating ENS Sympathetic stimulation decreases secretions and activity by inhibiting ENS Copyright 2009, John Wiley & Sons, Inc. ENTERIC NERVOUS SYSTEM To ANS and CNS neurons Myenteric plexus Interneuron Submucosal plexus Motor neuron Motor neuron Longitudinal and circular smooth muscle layers of the muscularis Sensory neuron Mucosal epithelium Peritoneum Largest serous membrane of the body Divided into Parietal peritoneum – lines wall of cavity Visceral peritoneum – covers some organs Also called serosa Space between is peritoneal cavity 5 major peritoneal folds Greater omentum, falciform ligament, lesser omentum, mesentery, and mesocolon Weave between viscera binding organs together Copyright 2009, John Wiley & Sons, Inc. Peritoneum Cont. Greater omentum – largest “fatty apron” Falciform ligament – attaches liver to anterior abdominal wall Lesser omentum – suspends stomach and duodenum from liver – passage for hepatic portal vein and artery and common bile duct Next two loosely hold the intestines allowing for movement. Mesentery – bind jejunum and ilieum of Small Intestines to posterior abdominal wall Mesocolon - bind transverse and sigmoid colon to posterior abdominal wall Copyright 2009, John Wiley & Sons, Inc. Diaphragm Liver LESSER OMENTUM Pancreas Stomach MESOCOLON Duodenum MESENTERY Transverse colon GREATER OMENTUM Jejunum Ileum PARIETAL PERITONEUM Sigmoid colon Uterus VISCERAL PERITONEUM Urinary bladder PERITONEAL CAVITY Rectum Pubic symphysis POSTERIOR ANTERIOR (a) Midsagittal section showing the peritoneal folds Midsagittal plane FALCIFORM LIGAMENT Liver Stomach Transverse colon GREATER OMENTUM Urinary bladder (b) Anterior view Gallbladder (reflected upward) LESSER OMENTUM Liver (reflected upward) Stomach Duodenum Transverse colon Descending colon Ascending colon Sigmoid colon (c) Lesser omentum, anterior view (liver and gallbladder lifted) GREATER OMENTUM (reflected upward) Transverse colon Jejunum (pulled laterally) MESENTERY Descending colon Ileum (pulled laterally) Sigmoid colon Urinary bladder (d) Anterior view (greater omentum lifted and small intestine reflected to right side) Mouth Oral or buccal cavity Formed by cheeks, hard and soft palates, and tongue Oral cavity proper, is a space that extends from gums and teeth to fauces (opening between oral cavity and oropharynx) Salivary glands release saliva Ordinarily, just enough is secreted to keep mouth and pharynx moist and clean When food enters mouth, secretion increases to lubricate, dissolve and begin chemical digestion 3 pairs of major salivary glands secrete most of the saliva Parotid, submandibular, and sublingual Copyright 2009, John Wiley & Sons, Inc. Superior lip (lifted upward) Superior labial frenulum Gingivae (gums) Palatoglossal arch Hard palate Fauces Soft palate Palatopharyngeal arch Uvula Cheek Palatine tonsil (between the arches) Molars Tongue (lifted upward) Lingual frenulum Opening of duct of submandibular gland Premolars Cuspid (canine) Incisors Oral vestibule Gingivae (gums) Inferior labial frenulum Inferior lip (pulled down) Anterior view Central incisor(8–12 mo.) Lateral incisor(12–24 mo.) Cuspid or canine (16–24 mo.) D E FG H C B I A J First molar (12–16 mo.) Second molar (24–32 mo.) Upper Teeth Lower Teeth Second molar (24–32 mo.) T K S L R M Q P ON First molar (12–16 mo.) Cuspid or canine (16–24 mo.) Lateral incisor(12–15 mo.) Central incisor(6–8 mo.) (a) Deciduous (primary) dentition; teeth are designated by letters (with times of eruption) Central incisor (7–8 yr.) Lateral incisor(8–9 yr.) 7 8 6 5 4 Cuspid or canine (11–12 yr.) 9 1011 12 13 3 First premolar or bicuspid (9–10 yr.) Second premolar or bicuspid (10–12 yr.) 14 2 15 Upper Teeth 1 First molar (6–7 yr.) 16 Second molar (12–13 yr.) Third molar or wisdom tooth (17–21 yr.) Lower Teeth 32 17 31 Third molar or wisdom tooth (17–21 yr.) 18 30 Second molar (11–13 yr.) 29 28 2726 19 First molar (6–7 yr.) 20 21 Second premolar or bicuspid (11–12 yr.) 22 252423 First premolar or bicuspid (9–10 yr.) (b) Permanent (secondary) dentition; teeth are designated by numbers (with times of eruption) Cuspid or canine (9–10 yr.) Lateral incisor(7–8 yr.) Central incisor(7–8 yr.) Parotid duct Zygomatic arch PAROTID GLAND Opening of parotid duct (near second maxillary molar) Second maxillary molar tooth Tongue (raised in mouth) Lingual frenulum Sublingual ducts Lesser sublingual duct Submandibular duct SUBMANDIBULAR GLAND SUBLINGUAL GLAND Mylohyoid muscle (a) Location of salivary glands The three major salivary glandsparotid, sublingual, and submandibular Saliva Saliva Mostly water 99.5% 0.5% solutes – ions, dissolved gases, urea, uric acid, mucus, immunoglobulin A, lysozyme, and salivary amylase (acts on starch) Not all salivary glands produce the same saliva Salivation Controlled by autonomic nervous system Parasympathetic stimulation promotes secretion of moderate amount of saliva Sympathetic stimulation decreases salivation Copyright 2009, John Wiley & Sons, Inc. Tongue and Teeth Tongue Accessory digestive organ Skeletal muscle covered by mucous membrane Maneuvers food for chewing, shapes mass, forces food back for swallowing Lingual glands secrete salivary lipase Teeth or dentes Accessory digestive organ 3 major regions – crown, root, and neck Dentin of crown covered by enamel 2 dentitions – deciduous and permanent teeth Copyright 2009, John Wiley & Sons, Inc. Sagittal plane Enamel Dentin CROWN Gingival sulcus Gingiva (gum) Pulp in pulp cavity NECK Cementum Root canal Alveolar bone ROOT Periodontal ligament Apical foramen Nerve Blood supply Sagittal section of a mandibular (lower) molar Digestion in the mouth Mechanical digestion in the mouth Chewing or mastication Food manipulated by tongue, ground by teeth, and mixed with saliva Forms bolus Chemical digestion in the mouth Salivary amylase secreted by salivary glands acts on starches Only monosaccharides can be absorbed Continues to act until inactivated by stomach acid Lingual lipase secreted by lingual glands of tongue acts on triglycerides Becomes activated in acidic environment of stomach Copyright 2009, John Wiley & Sons, Inc. Pharynx Passes from mouth into pharynx 3 parts Nasopharynx Oropharynx Functions only in respiration Digestive and respiratory functions Laryngopharynx Digestive and respiratory functions Copyright 2009, John Wiley & Sons, Inc. Esophagus Secretes mucous, transports food – no enzymes produced, no absorption Mucosa – protection against wear and tear Submucosa Muscularis divided in thirds Superior 1/3 skeletal muscle Middle 1/3 skeletal and smooth muscle Inferior 1/3 smooth muscle 2 sphincters – upper esophageal sphincter (UES) regulates movement into esophagus, lower esophageal sphincter (LES) regulates movement into stomach Adventitia – no serosa – attaches to surroundings Copyright 2009, John Wiley & Sons, Inc. Histology of the esophagus Copyright 2009, John Wiley & Sons, Inc. Deglutition Act of swallowing Facilitated by secretions of saliva and mucus Involves mouth, pharynx, and esophagus 3 stages Voluntary – bolus passed to oropharynx Pharyngeal – involuntary passage through pharynx into esophagus Esophageal – involuntary passage through esophagus to stomach Peristalsis pushes bolus forward Copyright 2009, John Wiley & Sons, Inc. Nasopharynx Hard palate Soft palate Bolus Uvula Oropharynx Tongue Epiglottis Laryngopharynx Larynx Esophagus (a) Position of structures before swallowing (b) During pharyngeal stage of swallowing Esophagus Relaxed muscularis Circular muscles contract Longitudinal muscles contract Relaxed muscularis Lower esophageal sphincter Bolus Stomach (c) Anterior view of frontal sections of peristalsis in esophagus Stomach Serves as mixing chamber and holding reservoir 4 main regions Cardia, fundus, body, pylorus Same 4 layers Mucosa – gastric glands open into gastric pits 3 types of exocrine gland cells – mucous neck cells (mucus), parietal cells (intrinsic factor; V-B12 and HCl), and chief cells (pepsinogen and gastric lipase) G cell – endocrine cell – secretes H’ gastrin Submucosa Muscularis – additional 3rd inner oblique layer Serosa – part of visceral peritoneum Copyright 2009, John Wiley & Sons, Inc. Esophagus Lower esophageal sphincter FUNDUS Serosa CARDIA Muscularis: Longitudinal layer BODY Circular layer Lesser curvature PYLORUS Oblique layer Greater curvature Duodenum Pyloric sphincter Rugae of mucosa PYLORIC ANTRUM PYLORIC CANAL (a) Anterior view of regions of stomach Esophagus Duodenum PYLORUS Pyloric sphincter PYLORIC CANAL Lesser curvature PYLORIC ANTRUM FUNDUS CARDIA BODY Rugae of mucosa Greater curvature (b) Anterior view of internal anatomy Lumen of stomach Gastric pits Surface mucous cell Lamina propria Lymphatic nodule Mucous neck cell Parietal cell Chief cell Gastric gland G cell Muscularis mucosae MUCOSA SUBMUCOSA Lymphatic vessel MUSCULARIS Venule Arteriole Oblique layer of muscle Circular layer of muscle SEROSA Myenteric plexus Longitudinal layer of muscle (a) Three-dimensional view of layers of stomach Gastric pit Surface mucous cells Gastric pit Lamina SEM 40x propria Stomach mucosa Gastric glands Muscularis mucosae Surface mucous cell (secretes mucus) Mucous neck cell (secretes mucus) Parietal cell (secretes hydrochloric acid and intrinsic factor) Chief cell (secretes pepsinogen and gastric lipase) G cell (secretes the hormone gastrin) Submucosa (b) Sectional view of stomach mucosa showing gastric glands and cell types Mechanical and Chemical Digestion Mechanical digestion Mixing waves – gentle, rippling peristaltic movements – creates chyme Chemical digestion Digestion by salivary amylase continues until inactivated by acidic gastric juice Acidic gastric juice activates lingual lipase Digest triglycerides into fatty acids and diglycerides Parietal cells secrete H+ and Cl- separately but net effect is HCl Kills many microbes, denatures proteins Copyright 2009, John Wiley & Sons, Inc. Chemical Digestion Chemical digestion (cont.) Pepsin secreted by chief cells digest proteins Secreted as pepsinogen Gastric lipase splits triglycerides into fatty acids and monoglycerides Small amount of nutrient absorption Some water, ions, short chain fatty acids, certain drugs (aspirin) and alcohol Copyright 2009, John Wiley & Sons, Inc. Pancreas Lies posterior to greater curvature of stomach Pancreatic juice secreted into pancreatic duct and accessory duct and to small intestine Pancreatic duct joins common bile duct and enters duodenum at hepatopancreatic ampulla Histology 99% of cells are acini Exocrine Secrete pancreatic juice – mixture of fluid and digestive enzymes 1% of cells are pancreatic islets (islets of Langerhans) Endocrine Secrete hormones glucagon, insulin, somatostatin, and pancreatic polypeptide Copyright 2009, John Wiley & Sons, Inc. Falciform ligament Diaphragm Right lobe of liver Right hepatic duct Coronary ligament Left lobe of liver Left hepatic duct Common hepatic duct Gallbladder: Neck Body Round ligament Cystic duct Fundus Common bile duct Pancreas Tail Body Duodenum Pancreatic duct (duct of Wirsung) Accessory duct (duct of Santorini) Head Hepatopancreatic ampulla (ampulla of Vater) Uncinate process Jejunum (a) Anterior view Common bile duct Pancreatic duct (duct of Wirsung) Hepatopancreatic ampulla (ampulla of Vater) Mucosa of duodenum Major duodenal papilla Sphincter of the hepatopancreatic ampulla (sphincter of Oddi) (b) Details of hepatopancreatic ampulla Right hepatic duct Left hepatic duct Common hepatic duct from liver Cystic duct from gallbladder Common bile duct Pancreatic duct from pancreas Key: Liver Sphincter Gallbladder Pancreas Duodenum (c) Ducts carrying bile from liver and gallbladder and pancreatic juice from pancreas to duodenum Pancreatic juice 1200-1500ml daily (1.2-1.5 qt) Mostly water Sodium bicarbonate – buffers acidic stomach chyme Enzymes Pancreatic amylase (starch) Proteolytic enzymes – trypsin (secreted as trypsinogen), chymotrypsin (chymotrypsinogen), carboxypeptidase (procarboxypeptidase), elastase (proelastase) Pancreatic lipase (triglyceride) Ribonuclease and deoxyribonuclease (nucleic acids) Copyright 2009, John Wiley & Sons, Inc. Liver and gallbladder Liver is the heaviest gland of the body Liver is composed of Hepatocytes – major functional cells of liver Wide variety of metabolic, secretory, and endocrine functions – secrete bile (excretory product and digestive secretion) Bile canaliculi – ducts between hepatocytes that collect bile Exits livers as common hepatic duct, joins cystic duct from gallbladder to form common bile duct Hepatic sinusoids – highly permeable blood capillaries receiving oxygenated blood from hepatic artery and deoxygenated nutrientrich blood from hepatic portal vein 3 different ways to organize units Hepatic acinus – preferred method Hepatocytes arranged in 3 zones around short axis with no sharp boundaries Copyright 2009, John Wiley & Sons, Inc. Liver Inferior vena cava Hepatic artery Hepatic portal vein Connective tissue Portal triad: Bile duct Hepatocyte Hepatic laminae Branch of hepatic artery Branch of hepatic portal vein Central vein Hepatic sinusoids (a) Overview of histological components of liver Central vein To hepatic vein Hepatic sinusoids Bile canaliculi Portal triad: Bile duct Branch of hepatic portal vein Branch of hepatic artery Hepatic laminae Hepatocyte Stellate reticuloendothelial (Kupffer) cell Connective tissue Hepatic sinusoid (b) Details of histological components of liver Central vein Portal triad Hepatic lobule Portal lobule Hepatic acinus (d) Comparison of three units of liver structure and function Portal triad Central vein Central vein Zone 3 Zone 2 Zone 1 (e) Details of hepatic acinus Zone 1 Cells – 1st to receive oxygenated blood, nutrients and any toxins, 1st to take up glucose and store as glycogen after a meal. Also 1st to show change if there is a bile duct obstruction and last to die (poor circulation) and 1st to regenerate. Zone 3 Cells – last to show effect of bile duct obstruction or toxin, 1st to show effect from poor circulation and last to regenerate, 1st to show effect of fat accumulation. Zone 2 Cells Copyright 2009, John Wiley & Sons, Inc. Gallbladder Contraction of smooth muscle fibers eject contents of gall bladder into cystic duct Functions to store and concentrate bile produced by the liver until it is needed in the small intestine Absorbs water and ions to concentrate bile up to ten-fold Copyright 2009, John Wiley & Sons, Inc. Hepatic blood flow Liver receives blood from Hepatic artery carrying oxygenated blood Hepatic portal vein carrying deoxygenated blood with newly absorbed nutrients and possibly drugs, microbes or toxins from GI tract Copyright 2009, John Wiley & Sons, Inc. Oxygenated blood from hepatic artery 1 Nutrient-rich, deoxygenated blood from hepatic portal vein 2 Liver sinusoids 3 Central vein 4 Hepatic vein 5 Inferior vena cava 6 Right atrium of heart Hepatic Inferior vena cava Stomach Spleen HEPATIC PORTAL Short gastric Left gastric Liver Pancreas (behind stomach) Cystic Gallbladder Pancreati c Left gastroepiploic Duodenum Right gastric Pancreaticoduoden al Pancreas SPLENIC Transverse colon SUPERIOR MESENTERIC Middle colic Right colic Jejunal and ileal Ascending colon Right gastroepiploic Left colic Inferior mesenteric Descending colon Ileocolic Cecum Sigmoidal Appendix Ileum Drain into superior mesenteric vein Drain into splenic vein Drain into inferior mesenteric vein (a) Anterior view of veins draining into hepatic portal vein Sigmoid colon Superior rectal Rectum Inferior vena cava Heart Hepatic veins Liver Abdominal aorta Proper hepatic artery Splenic vein Tributaries from portions of stomach, pancreas, and portions of large intestine Superior mesenteric vein Tributaries from small intestine and portions of large intestine, stomach, and pancreas Hepatic portal vein (b) Scheme of principal blood vessels of hepatic portal circulation and arterial supply and venous drainage of liver Role and composition of bile Hepatocytes secrete 800-1000mL of bile daily Mostly water, bile salts, cholesterol, lecithin, bile pigments and several ions Bilirubin – principal bile pigment Derived from heme of recycled RBCs Breakdown product stercobilin gives feces brown color Bile salts play role in emulsification Also aid in absorption of lipids following digestion Copyright 2009, John Wiley & Sons, Inc. Functions of the Liver p.995 Carbohydrate metabolism and blood glucose homeostasis. Lipid and protein metabolism and produce plasma proteins Process drugs and proteins Excretion of bilirubin a waste from recycles RBC and excreted in feces Synthesis of bile salts – emulsification and absorption of lipids, Storage – glycogen, A, B12, D, E, K, iron and copper See Table 25.5 and 25.6, Phagocytosis – reticuloendothelial cells, RBC, WBC Copyright 2009, John Wiley & Sons, Inc. Small intestine 3 regions – duodenum (10”), jejunum (3’), and ileum (6’) – Pyloric sphincter to the ileocecal sphincter Same 4 layers 1. Mucosa Absorptive cells (digest and absorb), goblet cells (mucus), intestinal glands (intestinal juice), Paneth cells (lysozyme), and enteroendocrine cells Abundance of MALT Submucosa 2. Duodenal glands secrete alkaline mucus Muscularis Serosa 3. 4. Completely surrounds except for major portion of duodenum Copyright 2009, John Wiley & Sons, Inc. Anatomy of the small intestine Copyright 2009, John Wiley & Sons, Inc. Special structural features increase surface area for digestion and absorption Circular folds Permanent ridges of mucosa and submucosa Cause chyme to spiral Villi Fingerlike projections of mucosa Contains arteriole, venule, blood capillary, and lacteal Microvilli Projects of apical membrane of absorptive cells Brush border with brush border enzymes Copyright 2009, John Wiley & Sons, Inc. Circular folds (plicae circulares) Circular folds Villi Submucosa (a) Relationship of villi to circular folds Circular layer of muscle Longitudinal layer of muscle Serosa Lumen of small intestine Blood capillary Lacteal Villi Opening of intestinal gland Absorptive cell Goblet cell Lacteal Lamina propria MUCOSA Enteroendocrine cell Paneth cell Lymphatic nodule Muscularis mucosae SUBMUCOSA Arteriole Venule Lymphatic vessel MUSCULARIS Circular layer of muscle Myenteric plexus Longitudinal layer of muscle (b) Three-dimensional view of layers of the small intestine showing villi SEROSA Microvilli Absorptive cell (absorbs nutrients) Blood capillary Lacteal Mucosa Goblet cell (secretes mucus) Lamina propria Intestinal gland Enteroendocrine cell (secretes the hormones secretin, cholecystokinin, or GIP) Muscularis mucosae Arteriol Submucosa Venule Paneth cell (secretes lysozyme and is capable of phagocytosis) Lymphatic vessel Muscularis (c) Enlarged villus showing lacteal, capillaries, intestinal glands, and cell type Histology of the duodenum and ileum Copyright 2009, John Wiley & Sons, Inc. Intestinal juice and brush-border enzymes Intestinal juice 1-2L daily Contains water and mucus, slightly alkaline Provide liquid medium aiding absorption Brush border enzymes Inserted into plasma membrane of absorptive cells Some enzymatic digestion occurs at surface rather than just in lumen Carbohydrate = α-dextrinase, maltase, sucrase, lactase, Protein = aminopetidase, dipeptidase, nucleotide = nucleosidases and phosphatases Copyright 2009, John Wiley & Sons, Inc. Mechanical Digestion Governed by myenteric plexus Segmentations Localized, mixing contractions Mix chyme and bring it in contact with mucosa for absorption Migrating motility complexes (MMC) Type of peristalsis Begins in lower portion of stomach and pushes food forward Copyright 2009, John Wiley & Sons, Inc. Chemical digestion Carbohydrates Pancreatic amylase α-dextrinase, sucrase, lactase, maltase in brush border Ends with monosaccharides which can be absorbed Proteins Trypsin, chymotrypsin, carboxypeptidase, and elastase from pancreas – proteins to peptides Aminopeptidase and dipeptidase in brush border Copyright 2009, John Wiley & Sons, Inc. Lipids and Nucleic Acids Lipids Pancreatic lipase most important in triglyceride digestion Emulsification by bile salts increases surface area of lipids. Nucleic acids Ribonuclease and deoxyribonuclease in pancreatic juice Nucleosidases and phosphatases in brush border Copyright 2009, John Wiley & Sons, Inc. Absorption of: Monosaccharides All dietary carbohydrates digested are absorbed Only indigestible cellulose and fibers left in feces Absorbed by facilitated diffusion or active transport into blood Amino acids, dipetides and tripeptides Most absorbed as amino acids via active transport into blood ½ of absorbed amino acids come from proteins in digestive juice and dead mucosal cells Copyright 2009, John Wiley & Sons, Inc. Lipids All dietary lipids absorbed by simple diffusion Short-chain fatty acids go into blood for transport Long-chain fatty acids and monoglycerides Enter lacteals to eventually enter blood Copyright 2009, John Wiley & Sons, Inc. Glucose and galactose Fructose Secondary active transport with Na+ Facilitated diffusion Facilitated diffusion Amino acids Active transport or secondary active transport with Na+ Dipeptides Tripeptides Small short-chain fatty acids To blood capillary of a villus Amino acids Diffusion Secondary active transport with H+ Simple diffusion Large short-chain and long-chain fatty acids Micelle Monosaccharides Diffusion Triglyceride Simple diffusion To lacteal of a villus Monoglycerides Chylomicron Lumen of small intestine Microvilli (brush border) on apical surface Basolateral surface Epithelial cells of villus (a) Mechanisms for movement of nutrients through absorptive epithelial cells of villi Left subclavian vein Villus (greatly enlarged) Chylomicron Heart Liver Hepatic portal vein Thoracic duct Small shortchain fatty acid Blood capillary Amino acid Lacteal Monosaccharide Arteriole Venule Blood Lymphatic vessel Lymph (b) Movement of absorbed nutrients into blood and lymph Absorption of: Electrolytes Vitamins From GI secretions or food Sodium ions (Na+) reclaimed by active transport Other ions also absorbed by active transport Fat-soluble vitamins A, D, E, and K absorbed by simple diffusion and transported with lipids in micelles Most water-soluble vitamins also absorbed by simple diffusion Water 9.3L comes from ingestion (2.3L) and GI secretions (7.0L) Most absorbed in small intestine, some in large intestine Only 100ml excreted in feces All water absorption by osmosis Digestion Video – See Video Chapters 1-2 http://www.pbs.org/wgbh/nova/body/can -i-eat-that.html Copyright 2009, John Wiley & Sons, Inc. INGESTED AND SECRETED ABSORBED Saliva (1 liter) Ingestion of liquids (2.3 liters) Gastric juice (2 liters) Bile (1 liter) Pancreatic juice (2 liters) Intestinal juice (1 liter) Small intestine (8.3 liters) Total ingested and secreted = 9.3 liters Large intestine (0.9 liters) Total absorbed = 9.2 liters Excreted in feces (0.1 liter) Fluid balance in GI tract Large intestine Overall function to complete absorption, produce certain vitamins, and form and expel feces 4 major regions – cecum, colon, rectum, and anal canal Ileocecal sphincter between small and large intestine Colon divided into ascending, transverse, descending and sigmoid Opening of anal canal (anus) guarded by internal anal sphincter of smooth muscle and external anal sphincter of skeletal muscle Copyright 2009, John Wiley & Sons, Inc. TRANSVERSE COLON Left colic (splenic) flexure Right colic (hepatic) flexure Teniae coli ASCENDING COLON Teniae coli DESCENDING COLON Ileum Omental appendices Mesoappendix Haustra Ileocecal sphincter (valve) CECUM RECTUM VERMIFORM APPENDIX SIGMOID COLON ANAL CANAL ANUS (a) Anterior view of large intestine showing major regions Rectum Anal canal Internal anal sphincter (involuntary) External anal sphincter (voluntary) Anus Anal column (b) Frontal section of anal canal Large Intestine Same 4 layers Mucosa – mostly absorptive and goblet cells Submucosa Muscularis No circular folds or villi Does have microvilli Longitudinal muscle modified to form teniae coli Forms haustra – pouches Serosa Copyright 2009, John Wiley & Sons, Inc. Digestion of the Large Intestine Mechanical digestion Haustral churning Peristalsis Mass peristalsis – drives contents of colon toward rectum Chemical digestion Final stage of digestion through bacterial action Ferment carbohydrates, produce some B vitamins and vitamin K Mucus but no enzymes secreted Remaining water absorbed along with ions and some vitamins Copyright 2009, John Wiley & Sons, Inc. Lumen of large intestine Openings of intestinal glands Absorptive cell Goblet cell MUCOSA Intestinal gland Lamina propria Lymphatic nodule Muscularis mucosae Lymphatic vessel Arteriole SUBMUCOSA MUSCULARIS Venule Circular layer of muscle SEROSA Myenteric plexus Longitudinal layer of muscle (a) Three-dimensional view of layers of large intestine Openings of intestinal glands Lamina propria Microvilli Intestinal gland Absorptive cell (absorbs water) Goblet cell (secretes mucus) Muscularis mucosae Lymphatic nodule Submucosa (b) Sectional view of intestinal glands and cell types Histology of the large intestine Copyright 2009, John Wiley & Sons, Inc. Phases of digestion Cephalic phase Gastric phase Smell, sight, thought or initial taste of food activates neural centers – prepares mouth and stomach for food to be eaten Neural and hormonal mechanisms promote gastric secretion and motility Intestinal phase Begins when food enter small intestine Slows exit of chyme from stomach Stimulates flow of bile and pancreatic juice Copyright 2009, John Wiley & Sons, Inc. Food entering stomach disrupts homeostasis by Increasing pH of gastric juice Distention (stretching) of stomach walls Receptors Chemorecepto rs and stretch receptors in stomach detect pH increase and distention Input Control center Nerve impulses Submucosal plexus Output Return to homeostasis when response brings pH of gastric juice and distention of stomach walls back to normal (pre-eating status) Nerve impulses (parasympathetic) Effectors Parietal cells secrete HCI and smooth muscle in stomach wall contracts more vigorously Increase in acidity of stomach chyme; mixing of stomach contents; emptying of stomach HCI Defecation reflex Mass peristaltic movement from sigmoid colon to rectum, distension triggers reflex. Diarrhea Constipation Exercise, stress, fluid intake, dietary fiber Copyright 2009, John Wiley & Sons, Inc.