* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Delusional Disorder
History of psychosurgery in the United Kingdom wikipedia , lookup
Dementia praecox wikipedia , lookup
Schizophrenia wikipedia , lookup
Bipolar disorder wikipedia , lookup
Panic disorder wikipedia , lookup
Excoriation disorder wikipedia , lookup
Mental disorder wikipedia , lookup
Rumination syndrome wikipedia , lookup
Sluggish schizophrenia wikipedia , lookup
Child psychopathology wikipedia , lookup
Factitious disorder imposed on another wikipedia , lookup
Antipsychotic wikipedia , lookup
Antisocial personality disorder wikipedia , lookup
Depersonalization disorder wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Asperger syndrome wikipedia , lookup
Moral treatment wikipedia , lookup
Spectrum disorder wikipedia , lookup
Conduct disorder wikipedia , lookup
Schizoaffective disorder wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Emergency psychiatry wikipedia , lookup
History of mental disorders wikipedia , lookup
Conversion disorder wikipedia , lookup
History of psychiatry wikipedia , lookup
Abnormal psychology wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
Mental status examination wikipedia , lookup
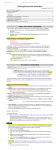
Delusional Disorder Dr.Arfat H. Al Dujaily 2009 Introduction Delusional disorder is an illness characterized by the presence of nonbizarre delusions in the absence of other mood or psychotic symptoms. Diagnostic Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) (APA, 2000) defines delusions as false beliefs based on incorrect inference about external reality that persist despite the evidence to the contrary and these beliefs are not ordinarily accepted by other members of the person's culture or subculture. Nonbizarre refers to the fact that this type of delusion is about situations that can occur in real life such as being followed, being loved, having an infection, and being deceived by one's spouse. In contrast, bizarre delusions, which represent the manifestations of more severe types of psychotic illnesses (eg, schizophrenia) "are clearly implausible, not understandable, and not derived from ordinary life experiences" (APA, 2000). On the other end of the spectrum, making a distinction between a delusion and an overvalued idea is important, the latter representing an unreasonable belief that is not firmly held (APA, 2000). Additionally, personal beliefs should be evaluated with great respect to complexity of cultural and religious differences: some cultures have widely accepted beliefs that may be considered delusional in other cultures. Because of poor insight into their pathological experiences, patients with delusional disorder may rarely seek psychiatric help and often may present to internists, surgeons, dermatologists, policemen, and lawyers rather than psychiatrists. History The concept of the delusional disorder has both a very long and a very short history: while the term of delusional disorder was only coined in 1977, the concept of paranoia has been used for centuries. Originally, the word paranoia comes from Greek para, meaning along side, and noos or nous, meaning mind, intelligence (Munro, 1999). The Greeks used this term to describe any mental abnormalities similar to how we use the word insanity. In the modern world, the term reappeared in the 17th century, and it was largely used as a generic name for mental illness. In 1863, Karl Kahlbaum introduced the concept of paranoia as a separate mental illness: "a form of partial insanity, which throughout the course of the disease principally affected the sphere of the intellect" (Manschreck, 2000). He used this term to describe an illness with persistent delusions and stable course. He noted that delusions may occur in other medical and psychiatric conditions (Manschreck, 2000). Later Emil Kraepelin, who observed 19 cases, continued to work on defining the concept of paranoia, which is reflected in several editions of his famous textbook and most closely resembles the modern definition of delusional disorder. Kraepelin viewed paranoia as uncommon, chronic condition different from dementia praecox by the presence of fixed, nonbizarre delusions, lack of deterioration over time, preserved thought process, and relatively slight involvement of affect and volition (Manschreck, 2000). He described that delusions of paranoia, contrary to the delusions of dementia praecox, are well systemized, relatively consistent, and often related to real-life events. He identified persecutory, grandiose, jealous, erotomanic, and possibly hypochondriacal types of that disorder. He believed that the illness derived from the deficit in the patients' judgments caused by constitutional factors and environmental stress (Manschreck, 2000; Munro, 1999). Later, Eugen Bleuler continued to recognize paranoia as a separate disorder and included hallucinations in its description (Fennig, 2005; Munro, 1999). After Kraepelin's death, Kurt Kolle (1931) reported a detailed follow-up of 66 cases seen in Kraepelin's former clinic in Munch (Munro, 1999). He noted a pattern of deterioration and concluded that paranoia represents a form of schizophrenia. This view continued to be popular in the psychiatric community for several decades and was reflected in DSM-I and DSM-II. Winokur (1977) had redescribed paranoia under the name of delusional disorder basing his findings on Kraepelin's definition and the observation of case types (Munro, 1999). Additionally, Kendler (1980) and Munro (1982) substantially contributed to our current understanding of nosology of this illness (Munro, 1999; Kelly, 2005). In 1987, delusional disorder was introduced in DSM-III-R and continued to be present in subsequent editions. Current Diagnosis DSM-IV-TR (APA, 2000) defines delusional disorder with the following criteria: Criterion A: Nonbizarre delusions (ie, involving situations that occur in real life, such as being followed, poisoned, infected, loved at distance, or deceived by spouse or lover, or having a disease) of at least 1 month's duration. Criterion B: Criterion A for schizophrenia has never been met (ie, patients do not have simultaneous hallucinations, disorganized speech, negative symptoms such as affective flattening, or grossly disorganized behavior). Note: Tactile and olfactory hallucinations may be present in delusional disorder if they are related to the delusional theme. Criterion C: Apart from the impact of the delusion(s) or its ramifications, functioning is not markedly impaired, and behavior is not obviously odd or bizarre. Criterion D: If mood episodes have occurred concurrently with delusions, their total duration has been brief relative to the duration of the delusional periods. Criterion E: The disturbance is not due to the direct physiological effects of a substance (eg, a drug of abuse, a medication) or a general medical condition. Subtypes are defined, including erotomanic, grandiose, jealous, persecutory, somatic, mixed, and unspecified. Epidemiology The prevalence of delusional disorder in the United States is estimated in the DSM-IV-TR to be around 0.03% (APA, 2000), which is considerably lower than the prevalence of schizophrenia (1%) and mood disorders (5%) (Sadock, 2003). According to the DSM-IV-TR, delusional disorder accounts for 1-2% of admissions to inpatient mental health facilities (APA, 2000). The incidence of first admissions for delusion disorder is considerably lower, between 0.001 and 0.003% (Kendler, 1982). A British study reported that of 227 patients presented to mental health centers during the 3-year study period with a first episode of psychosis, 7% were diagnosed with persistent delusional disorder, as compared to 11% with schizophrenia and 19% with psychotic depression (Proctor, 2003). The incidence of first admission for delusional disorder in this study was 0.007%, which is 2-7 times as high as in the Kendler data. The mean age of onset is 40 years and ranges from 18-90 years (Sadock, 2003). The female-to-male ratio has been reported to vary between 1.18. (Kendler, 1982) and 3:1 (Yamada et al 1998 as cited in Kelly, 2005). Men are more likely than woman to develop paranoid delusions; women are more likely than men to develop delusions of erotomania (Sadock, 2003). Associated factors include being married, being employed, recent immigration, low socioeconomic status, celibacy among men, and widowhood among women (Kendler, 1982; Manschreck, 2000). Etiology General considerations The etiology of delusional disorder is unknown, and several difficulties exist in conducting research in this area: The definition of this condition has changed over time and continues to be a work in progress. Patients currently diagnosed with delusional disorder may represent a heterogeneous group of patients with delusions as the predominant symptom. Patients often do not present for treatment, and thus they do not commonly make themselves available for research studies. However, strong indications exist that delusional disorder is a distinct condition, different from schizophrenia or mood disorder. Naturalistic studies indicated that delusional disorder has a relatively stable course Genetics Kendler (1981) noted significantly lower prevalence of schizophrenia in families of patients with delusional disorder (0.6%) compared with families with schizophrenia (3.8%). Later Kendler and his colleagues (1985) showed that a history of paranoid personality disorder was more common in first-degree relatives of patients with delusional disorder (4.8%) compared with medical controls (0%) and patients with schizophrenia (0.8%). In their study they found no increased incidence of schizophrenia, schizoid-schizotypal personality disorder, and affective illness in the first-degree relatives of delusional disorder patients. Biochemical factors Delusions are associated with a wide range of nonpsychiatric medical conditions, which suggest that biological factors may play some role in the development of delusional disorder. Among patients with neurologic disorders (primarily dementia, head injury, and seizures) conditions involving the basal ganglia and temporal lobe are most commonly associated with delusions (Sadock, 2003; Gorman and Cummings, 1990). Hyperdopaminergic states have been implemented in the development of delusions. Recently, Morimoto et al (2002) reported that 13 patients with delusional disorder were reported to have increased levels of plasma homovanillic acid (HVA) (a dopamine metabolite) compared with control subjects, and that the level of HVA is correlated with severity of psychotic symptoms. His patients responded well to treatment with low-dose haloperidol (average 2.7 mg/d) and showed decreased posttreatment plasma level of HVA, which correlated with the improvement of their symptoms. The same authors reported an increased prevalence of a polymorphism at the D2 receptor gene at amino acid 311 (cysteine-for-serine substitution) among individuals with delusional disorder in their sample who have persecutory delusions; they also reported that individuals in their sample with more TCAT repeats within the first intron of the tyrosine hydroxylase gene have higher levels of HVA (Morimoto, 2002), although it is unclear if they corrected for multiple statistical comparisons. Psychological factors Cognitive and experimental psychology suggest that persons with delusions selectively attend to available information, make conclusions on the basis on insufficient information, attribute negative events to external personal causes, and have difficulty in envisaging other's intentions and motivations (Fennig, 2005). Conway et al (2002) reported that patients with delusional disorder required less data to make probability decisions compared with normal controls. Despite using less data, they were as certain as controls regarding the accuracy of their decisions. Psychodynamic theories suggest that paranoia is a protective response to stress or conflict that represents a threat to self-esteem or to the self (eg, unacceptable homosexual impulses, fear of the unknown, immigration) (Fennig, 2005). Clinical Features General approach Theo Manschreck (1996) outlined 3 steps in the initial evaluation of patients presented with delusions. The first step in the clinical evaluation is establishing whether pathology is present. This represents a clinical judgment that sometimes is difficult to make. Some comments that appear delusional may, in fact, be true. In contrast, some reports that initially seem believable may be later identified as delusions as the symptoms worsen, the delusions become less encapsulated (ie, begin to extend to more people or situations), and more information comes to light. The clinical judgment that delusions are present should be made after taking into account the degree of plausibility, systemization, and the possible presence of culturally sanctioned beliefs that are different from one's own beliefs. Making the distinction between a true observation, a firm belief, an overvalued idea, and a delusion is sometimes a challenging task. Often, the extremeness and inappropriateness of the patient's behaviors, rather than the simple truth or falsity of the belief, indicate its delusional nature(Manschreck,1996;Fennig,2005). The second step is determining the presence or absence of important characteristics often associated with delusions, such as confusion, agitation, perceptual disturbances, physical symptoms, and prominent mood abnormalities (which would point away from a diagnosis of delusional disorder and toward other diagnoses) (Manschreck, 1996). The third step is to present a systematic differential diagnosis. A thorough history, mental status examination, and laboratory/radiologic evaluation should be performed to rule out other medical and psychiatric conditions that are commonly present with delusions. Delusional disorder should be seen as a diagnosis of exclusion (Manschreck, 1996). Clinical presentation (Manschreck, 1999; Manschreck, 2000; Fennig, 2005) The mental examination is usually normal with exception of the presence of abnormal delusional beliefs. In general, patients are well groomed and well dressed without evidence of gross impairment. Speech, psychomotor activity, and eye contact may be affected by the emotional state associated with delusions. Mood and affect are consistent with delusional content; for example, patients with persecutory delusions may be suspicious and anxious. Mild dysphoria may be present without regard of type of delusions. Tactile and olfactory hallucinations may be present and may be prominent if they are related to the delusional theme (eg, the sensation of being infested by insects, the perception of body odor). Medical causes of tactile and olfactory hallucinations, such as substance intoxication and withdrawal, temporal lobe epilepsy, and others, should be ruled out. Auditory or visual hallucinations are uncommon but, if present, they are not prominent. The thought content is notable for systematized, well-organized, nonbizarre delusions that are possible to occur, such as delusions of being persecuted, being loved by a person of higher status, being infected, having an unfaithful spouse, and others. Delusional concepts may be complex or simple, but bizarre beliefs such as delusions of thought insertion, and thought control are more common in schizophrenia. Contrary to schizophrenia, the thought process is usually not impaired; however, some circumstantiality and idiosyncrasy may be observed. Memory and cognition are intact. Level of consciousness is unimpaired. Patients usually have little insight and impaired judgment regarding their pathology. Police, family members, coworkers, and physicians other than psychiatrists are usually the first to suspect the problem and seek psychiatric consultation. Seeking corroborative information, when permitted by the patient, is often crucial. Assessment of homicidal or suicidal ideation is extremely important in evaluating patients with delusional disorder. The presence of homicidal or suicidal thoughts related to delusions should be actively screened for and the risk of carrying out violent plans should be carefully assessed. Reid (2005) pointed out that some types of this illness— erotomanic, jealous, and persecutory—are associated with higher risk for violence than others (Reid, 2005). History of previous violent acts as well history of how aggressive feelings were managed in the past may help to assess the risk. Presentation of the subtypes Erotomanic type o Related terms include erotomania, psychose passionelle, Clerambault syndrome, and old maid's insanity (Manschreck, 2000; Fennig, 2005; Kelly, 2005). o The central theme of delusions is that another person, usually of higher status, is in love with the patient. The object of delusion is generally perceived to belong to a higher social class, being married, or otherwise unattainable (Munro, 1999; Kelly, 2005). o Patients with this type of delusion are generally female, although males predominate in forensic samples (APA, 2000; Kelly, 2005). o Delusional love is usually intense in nature. Signs of denial of love by the object of the delusion are frequently falsely interpreted as affirmation of love (Manschreck, 2000; Kelly, 2005). o Patients may attempt to contact the object of the delusion by making phone calls, sending letters and gifts, making visits, and even stalking. Some cases lead to assaultive behaviors as a result of attempts to pursue the object of delusional love or attempting to "rescue" her/him from some imagined danger (APA, 2000). Grandiose type o Patients believe that they possess some great and unrecognized talent, have made some important discovery, have a special relationship with a prominent person, or have special religious insight (APA, 2000). o Grandiose delusions in the absence of mania are relatively uncommon, and the distinction of this subtype of disorder is debatable. Many patients with paranoid type show some degree of grandiosity in their delusions (Fennig, 2005). Jealous type o Related terms include conjugal paranoia, Othello syndrome, and pathological or morbid jealousy (Manschreck, 1999; Sadock, 2003). o The main theme of the delusions is that her or his spouse or lover is unfaithful. Some degree of infidelity may occur; however, patients with delusional jealousy support their accusation with delusional interpretation of "evidence" (eg, disarrayed clothing, spots on the sheets) (APA, 2000; Fennig, 2005). o Patients may attempt to confront their spouses and intervene in imagined infidelity. Jealousy may evoke anger and empower the jealous individual with a sense of righteousness to justify their acts of aggression. This disorder can sometimes lead to acts of violence, including suicide and homicide (Fennig, 2005). Persecutory type o Patients believe that they are being persecuted and harmed (Fennig, 2005). o In contrast to persecutory delusions of schizophrenia, the delusions are systematized, coherent, and defended with clear logic. No deterioration in social functioning and personality is observed (Manschreck, 2000). o Patients are often involved in formal litigation against their perceived persecutors. Munro (1999) refers to an article by Freckelton who identifies the following characteristics of deluded litigants: determination to succeed against all odds, tendency to identify the barriers as conspiracies, endless drive to right a wrong, quarrelsome behaviors, and "saturating the field" with multiple complaints and suspiciousness (Munro, 1999). o Patients often experience some degree of emotional distress such as irritability, anger, and resentment (Fennig, 2005). In extreme situations, they may resort to violence against those who they believe are hurting them (APA, 2000) o The distinction between normality, overvalued ideas, and delusions is difficult to make in some of the cases (Fennig, 2005). Somatic type o Related terms include monosymptomatic hypochondriasis (Fennig, 2005). o The core belief of this type of disorder is delusions around bodily functions and sensations. The most common are the belief that one is infested with insects or parasites, the belief of emitting a foul odor, the belief that parts of the body are not functioning, and the belief that their body or parts of the body are misshapen or ugly (APA, 2000). o Patients are totally convinced in physical nature of this disorder, which is contrary to patients with hypochondriasis who may admit that their fear of having a medical illness is groundless (Manschreck, 2000). o Patients are usually first seen by dermatologists, cosmetic surgeons, urologists, gastroenterologists, and other medical specialists (Fennig, 2005). o Sensory experiences associated with this illness (eg, sensation of parasites crawling under the skin) are viewed as components of systemized delusions (Fennig, 2005). Mixed type o Patients exhibit more than one of the delusions simultaneously (Fennig, 2005), and no one delusional theme predominates (APA, 2000). Unspecified type o Delusional themes fall outside the specific categories or cannot be clearly determined (APA, 2000). o Misidentification syndromes such as Capgras syndrome (characterized by a belief that a familiar person has been replaced by an identical impostor) or Fregoli syndrome (a belief that a familiar person is disguised as someone else) fall into this category. Misidentification syndromes are rare and frequently are associated with other psychiatric conditions (eg, schizophrenia) or organic illnesses (eg, dementia, epilepsy) (Fennig, 2005). o Another unusual syndrome is Cotard syndrome, in which patients believe that they have lost all their possessions, status, and strength as well as their entire being, including their organs (Fennig, 2005). Described first in the 19th century, it is a rare condition, which is usually considered a precursor to a schizophrenic or depressive episode (Manschreck, 2000). Differential Diagnosis Table 1. Medical Conditions Associated With Development of Delusions (Fenning et al, 2005) Medical Conditions Examples Neurodegenerative disorders Alzheimer disease, Pick disease, Huntington disease, basal ganglia calcification, multiple sclerosis, metachromatic leukodystrophy Other CNS disorders Brain tumors, especially temporal lobe and deep hemispheric tumors; epilepsy, especially complex partial seizure disorder; head trauma (subdural hematoma); anoxic brain injury; fat embolism Vascular disease Atherosclerotic vascular disease, especially when associated with diffuse, temporoparietal, or subcortical lesions; hypertensive encephalopathy; subarachnoid hemorrhage, temporal arteritis Infectious disease Human immunodeficiency virus/acquired immune deficiency syndrome, encephalitis lethargica, Creutzfeldt-Jakob disease, syphilis, malaria, acute viral encephalitis Metabolic disorder Hypercalcemia, hyponatremia, hypoglycemia, uremia, hepatic encephalopathy, porphyria Endocrinopathies Addison disease, Cushing syndrome, hyperthyroidism or hypothyroidism, panhypopituitarism Vitamin deficiencies Vitamin B-12 deficiency, folate deficiency, thiamine deficiency, niacin deficiency Medications Adrenocorticotropic hormones, anabolic steroids, corticosteroids, cimetidine, antibiotics (cephalosporins, penicillin), disulfiram, anticholinergic agents Substances Amphetamines, cocaine, alcohol, cannabis, hallucinogens Toxins Mercury, arsenic, manganese, thallium Delusional symptoms are preferentially associated with disorders involving the limbic system and basal ganglia (Fennig, 2005). Fifty percent of patients with Huntington disease and individuals with idiopathic basal ganglia calcifications developed delusions at some point of their illness (Fennig, 2005). Head trauma has been associated with development of delusions. Koponen et al (2002) found patients with traumatic brain injury were diagnosed with delusional disorder in 5% of the cases during a 30-year follow-up (3 out of 60 assessed patients). Table 2. Disorders and Differentiating Features Disorder Differentiating Features Delirium Fluctuating level of consciousness and impaired cognition are features of delirium that are absent in delusional disorder. Dementia Delusions (usually persecutory) are common in Alzheimer and other types of dementia (the prevalence ranges from 15-50%) and may present first, before cognitive deficits become apparent. Neuropsychological testing may be warranted to detect cognitive impairments. Additionally, elderly patients with delusional disorder were found to have an incidence of dementia that was twice as high as the general population's in a 10-year follow-up period (Leinonen, 2004). Substance-related disorders (intoxication, withdrawal, substance-induced psychotic disorder with delusion) Amphetamines and cocaine are the most commonly described substances to be associated with delusions, typically of persecutory type. Other illicit drugs (especially hallucinogens, anabolic steroids) and alcohol have been related to the development of delusions. (For example, alcohol withdrawal is a common condition, which may present with tactile or somatic delusions). Prescribed substances (especially steroids, dopamine agonists), OTC medications (especially sympathomimetics), and herbal products may also be associated with delusions. Careful substance and medication use history with specific attention to temporal relationship between substance use and onset/persistence of delusional symptoms may aid in differential diagnosis. Mood disorders with delusional symptoms (manic or depressive type) Mood symptoms are common in persons with delusional disorder and often represent an appropriate emotional response to perceived delusional experiences. However, given that mood disorders are common in the general population, they may present as comorbid conditions, often predating delusional disorder. Mood symptoms of mood disorders contrary to mood symptoms of delusional disorder are prominent and meet criteria for a full mood episode (depressive, manic, or mixed). Delusions associated with mood disorders usually develop after the onset of mood symptoms and progress secondary to mood abnormalities. Mood symptoms of delusional disorder are generally mild and delusions usually exist in the absence of mood abnormalities. Schizophrenia Delusions of schizophrenia are bizarre in nature, and hallucinations are common. Additionally, disorganized thought process, speech, or behaviors is present. Negative symptoms and deterioration in function are prominent. Cognitive deficits are common. Hypochondriasis Patients with hypochondriasis are usually able to doubt (at least for a short while) their convictions of having illness when presented with reassuring data. Most of them have a long history of preoccupation, and their fears are usually not limited to a single symptom or organ system. Body dysmorphic disorder (BDD) Many patients with BDD hold their beliefs with conviction that reaches level of delusions, leading to a significant overlap between these conditions. Obsessive-compulsive disorder (OCD) Patients with OCD show a varying degree of insight into their obsessions and compulsions. If reality testing is lost and conviction in their beliefs reaches the level of delusions, both disorders may be present. Paranoid personality disorder Differentiation between extreme suspiciousness and frank delusions may be difficult. History of pervasive distrust beginning by early adulthood is suggestive of personality disorder, while the delusional disorder most commonly presents as an acute illness of middle life. Additionally, patients with paranoid personality disorder frequently appear to be unemotional and lack warmth in their relationships. Shared psychotic disorder Symptoms emerge in the context of a close relationship with another person with delusional beliefs and diminish with separation from that other person. Treatment General considerations Delusional disorder is challenging to treat for various reasons, including patients' frequent denial that they have any problem, especially of a psychological nature, difficulties in developing a therapeutic alliance, and social/interpersonal conflicts. Careful assessment and diagnosis are crucial because delusions commonly represent an underlying organic illness that warrants specific treatment. Additionally, coexisting psychiatric disorders should be recognized and treated accordingly. Treatment of delusional disorder often involves both psychopharmacology and psychotherapy. Given the chronic nature of this condition, treatment strategies should be tailored to the individual needs of the patients and focus on maintaining social function and improving quality of life. Establishing a therapeutic alliance, establishing acceptable symptomatic treatment goals, and educating the patient's family are of paramount importance. Avoiding direct confrontation of the delusional symptoms enhances the possibility of treatment compliance and response. Hospitalization should be considered if a potential for harm or violence exists. Otherwise, outpatient treatment is preferred. Psychopharmacological treatment Limited data exist on the psychopharmacological treatment of delusional disorder. Most of the available information is based on case reports or small collection studies. No controlled studies have been published up to date. As such, evidence for the psychopharmacological treatment of delusional disorder would commonly be considered "grade C" (case series) or "grade D" (single case studies) evidence in many evidence-based medicine hierarchies, as opposed to randomized, blinded studies (grade A) or nonrandomized or nonblinded, but still systematically conducted, studies (grade B). (For example, see the Center for Evidence-Based Medicine guidelines). Antipsychotics have been used since the seventies when the first report was published on the use of pimozide for the treatment of monosymptomatic hypochondriacal psychosis (now classified as the delusional disorder, somatic type by DSM-IV-TR). Several case reports that followed supported its use. This medication continues to be cited as a preferential treatment for this disorder in literature. In 1995, Munro and Mok published a review of the treatment data published between 1965 and 1985 of approximately 1000 cases. They analyzed 257 cases and found that the body of evidence is limited and confusing. Nevertheless, they concluded that delusional disorder has a relatively good prognosis when adequately treated: 52.6% of the patients recovered, 28.2% achieved partial recovery, and 19.2% did not improve. Additionally, they reported that treatment response was positive regardless of the specific delusional content. They found that pimozide showed the strongest evidence of response compared with other typical antipsychotics: 68.5% recovery rate and 22.4% partial recovery rate were found in pimozide-treated cases and 22.6% recovery and 45.3% partial recovery were found in cases treated by other typical antipsychotics. Since then, new data have been accumulated, but the data still consist only of case reports. The most recent review of treatment for delusional disorder Manschreck and Khan (2006) analyzed 224 additional case reports published since 1995, and they summarized 134 case reports that provided sufficiently detailed information about treatment. The following is the summary of their findings: In general, delusional disorders were reported to be fairly responsive to treatment (50% of the published patients reported symptom-free recovery and 90% of patients showed at least some improvement). Polypharmacy was common, most often including a combination of antipsychotic and antidepressant medication. In addition, patients commonly received more than one antipsychotic over the course of their illness, and medication treatments were also complemented by other interventions, such as cognitivebehavioral therapy or even (in a single case) ECT. In contrast to previous findings, no significant difference was observed between treatment with pimozide and with other antipsychotics. In addition, no difference was observed between typical and atypical antipsychotic agents. The authors did identify that somatic delusions appeared potentially more responsive to antipsychotic therapy than other types of delusions (regardless of whether this treatment was pimozide or other antipsychotics). However, this difference may result from the generally poor response rates (50% improvement rates, with no reports of complete recovery) observed for the few case reports of treatment of delusional disorder with persecutory delusions. Four reports (5 cases) of individuals with delusions presumably refractory to previous antipsychotic treatment reported that clozapine was associated with an improved quality of life and a decrease in symptoms associated with the delusion, although the central delusional theme often persisted. Antidepressants have been successfully used for the treatment of delusional disorder, although primarily of the somatic type. The data consist of case reports showing improvement with SSRI (Hayashi, 2004) and clomipramine treatments (Sondheimer, 1988; Wada, 1999). Several case reports documented successful treatment with SSRI for culture-bound syndromes (conditions that would be diagnosed as somatic type of delusional disorder in Western cultures) (Nagata, 2006). A single case report of successful ECT use for somatic delusions exists (Ota, 2003). Review of treatment of delusional disorder have not systematically addressed the question of what dose of antipsychotic is not typically sufficient to achieve remission of symptoms; however, one study (Morimoto, 2002) did note that their 11 patients with delusional disorder appeared to be adequately treated on fairly low doses of antipsychotic (4.7 mg of haloperidol). In contrast, as indicated above (Manschreck and Khan, 2006), some cases of delusional disorder appear refractory even to clozapine treatment. In summary, a reasonable pharmacological treatment approach for the patient with delusional disorder is a standard trial of an antipsychotic or, for somatic delusions, SSRI at starting doses commonly used to treat psychotic or mood disorders. Psychotherapy For most patients with delusional disorder, some form of supportive therapy is helpful. The goals of supportive therapy include facilitating treatment adherence and providing education about the illness and its treatment. Educational and social interventions can include social skills training (eg, not discussing delusional beliefs in social settings) and minimizing risk factors, including sensory impairment, isolation, stress, and precipitants of violence. Providing realistic guidance and assistance in dealing with problems stemming from the delusional system may be very helpful (Fochtmann, 2005). Cognitive therapeutic approaches may be useful for some patients. The therapist helps the patient to identify maladaptive thoughts by means of Socratic questioning and behavioral experiments, and then to replace them with alternative, more adaptive beliefs and attributions. Discussion of the unrealistic nature of delusional beliefs should be done gently and only after rapport with the patient has been established (Silva, 2003; Fochtmann, 2005; Turkington, 2006). Some authors believe that insight-oriented therapy is rarely indicated (Forchtmann, 2005) or even contraindicated (Manschreck, 2000). However, reports exist of successful treatment (Silva, 2003). Goals in insight-oriented therapy include development of the therapeutic alliance; containing projected feelings of hatred, badness, and impotence; measured interpretation; and, ultimately, developing a sense of creative doubt in the internal perception of the world through empathy with the patient's defensive position (Silva, 2003). Principal sources for this review include American Psychiatric Association, 2000, DSM-IV-TR; the chapters by Manschrek and Fenning in Kaplan and Sadock's Comprehensive Textbook of Psychiatry (7th and 8th eds, respectively); the chapter by B.J. Sadock in Kaplan and Sadock's Synopsis of Psychiatry (9th ed); and Delusional disorder: paranoia and related illness by Munro, 1999; as well as the seminal treatment reviews by Munro and Mok, 1995, and Manschrek and Khan, 2006. Citations to original literature included when these citations could be confirmed, or occasionally by referencing a secondary, more recent source citing the original literature when the original report was not available. Specific references cited are provided below. Patient and family education Often the treatment approach covers patient education, but educating the family about the symptoms and course of the disorder is also useful. This is especially true since the family frequently feels the impact of the disorder the most.