* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download When Would You Remove a Central Venous Catheter
Neglected tropical diseases wikipedia , lookup
Tuberculosis wikipedia , lookup
Leptospirosis wikipedia , lookup
Hookworm infection wikipedia , lookup
Onchocerciasis wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Herpes simplex wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
West Nile fever wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hepatitis C wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Marburg virus disease wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Sarcocystis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Trichinosis wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Schistosomiasis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Candidiasis wikipedia , lookup
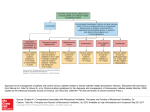
Provided by When Would You Remove a Central Venous Catheter from a Child with Cancer? Lead contributor: Hugo Paganini, MD Hospital JP Garrahan Buenos Aires, Argentina. Translation by: Nicolas Fernandez, MD Hospital JP Garrahan Buenos Aires, Argentina. A. Important Issues Each year, more than 150 million intravascular devices are used in the United States. These devices are implanted for the management of intravenous fluids, medications, or blood products. These devices are usually well tolerated by patients, but complications associated with their use may develop under certain conditions. Thrombosis and infections are the infections commonly associated with intravascular devices. The incidence of endovascular catheterrelated infections in the United States is 80,000 every year, and these infections are the most frequently occurring infection in pediatric hospitals. The risk of acquiring a catheter-related infection depends on several factors: the inclusion site, the age of the patient, the underlying disease, the experience of the surgeon implanting the device, and the strategies used to prevent infection. The indications and the right time for the removal of an infected catheter are under discussion. B. Epidemiology and Etiology Two types of long-term central venous catheters are used for children with cancer; totally implantable catheters such as the Port-A-Cath and tunneled catheters such as Hickman and Broviac catheters. The catheter-related infection rate in patients with cancer is estimated to be 0.83 for every 1000 days of use of the implantable catheter. The incidence rate increases to 2.85 for every 1000 days of use of tunneled catheters. In Hospital Garrahan in Buenos Aires, Argentina, the rate of infection is 1.56 catheter-related infection to every 1000 days of use. Gram-positive cocci are the microorganisms that often cause infections associated with intravascular devices in 50–60% cases. Coagulase-negative staphylococci are the prevalent causative organisms, followed by Staphylococcus aureus. The incidence of infections caused by gram-negative bacilli depends on epidemiology. Pseudomonas aeruginosa, Klebsiella pneumoniae, and Escherichia coli are the most common causative agents in such cases. Finally, between 5 and 10% of catheter-related infections are caused by Candida spp., and of these, approximately 50% by Candida albicans. C. Treatment Generally, treatment with antibiotics is indicated in most cases of catheter-related infections. Initial antibiotic selection should be based on epidemiological data from local centers. Data from studies of children indicate that 76% of catheter-related infections in children with implanted tunneled Page 2 of 8 catheters can be treated without removal of the catheter. Very few studies have been conducted on the access ports of catheters. A review of 5 studies of children with tunneled catheters revealed that 71–89% of these children were cured without removal of the device. In contrast, in a review of 9 studies that included 121 children with implantable catheters, it was observed that 95 of these children were cured without removal of the catheter. Currently, the indications for removing a long-term catheters are being debated. The decision to remove a permanent catheter depends on the age of the child, the underlying disease, clinical status, and the presence of cellulitis or embolic infections. The type of pathogen causing the infection is the main factor influencing the decision for catheter removal. C.1 Coagulase-negative Staphylococci Catheter-related infections are most frequently caused by coagulasenegative staphylococci. The course of the infection is usually mild and rarely associated with severe complications. No randomized studies have been performed to evaluate these infections in children. Recently, Raad et al reported the results of a cohort of 188 patients (children and adults) who developed bacteremia due to catheter-related infections caused by coagulase-negative staphylococci. In 175 of these patients, the catheter was not removed, and these patients were treated with antibiotics only. Recurrent infections were noted in 10% of these patients. In a multivariate analysis among patients needing removal of the catheter versus those treated with antibiotics only, the results revealed that the recurrence rate was significantly higher in patients whose implantable catheters had been retained. These authors concluded that leaving the catheter does not increase mortality, although patients whose device was not removed had a higher rate of recurrent infections. Page 3 of 8 According to the guidelines recently published by the Infectious Diseases Society of America (IDSA), catheters infected with coagulase negativestaphylococci should be withdrawn only after antibiotic treatment has been tried and has failed. C.2 Staphylococcus aureus No consensus has been reached on the indications for catheter removal in the pediatric population when the cause of the infections is S. aureus. Infections caused by S. aureus are more severe than those caused by other pathogens and have a high rate of associated complications and a mortality rate of 20%. According to the IDSA standards (2009), all patients with catheter-related infections caused by S. aureus should be treated with by both catheter removal and antibiotic therapy unless (1) there is no other alternative venous access available and (2) the patient has significant bleeding that is difficult to treat or (3) the child has a severe clinical condition that may be seriously complicated by catheter removal. It should be emphasized that the IDSA guidelines are based on the results of studies of adults, and the available data for studies in children are very scarce. In 4 pediatric studies, 70% of children were cured without catheter removal. A similar outcome with a success rate of 62% was observed in a small series study conducted at Garrahan Hospital, Argentina, on 13 children with catheter-related infections caused by S. aureus. C.3 Gram-negative bacilli Not much information is available on the treatment of children with implanted catheters infected by gram-negative bacilli. The available data are related to infections by specific pathogen.. The IDSA guidelines recommend catheter removal as the primary approach for patients who have catheterPage 4 of 8 related infections caused by gram-negative bacilli, whose health status is compromised, or who have persistent bacteremia. Infections caused by Acinetobacter baumannii, Pseudomonas spp., and Stenotrophomonas maltophilia, deserve special attention because these pathogens produce substances that promote the adhesion of organisms to the light source in the catheter. C.4 Fungi The importance of catheter extraction in children with candidal infections has long been debated. In the last few years, there has been a shift in the epidemiology of catheter-related infections caused by Candida species. An increasing number of candidal infections are caused by non-albicans species, especially Candida parapsilosis. Patients infected with such species usually develop persistent fungemia and embolic infections, and have a higher mortality rate if the catheter is not removed. Clinical trials (most of which have been conducted with adult participants only) revealed that removal of the infected device improves the patient’s status and prevents emergence complications. Currently, catheter removal is recommended for children with candidal infections. C.5 Other indications The other indications for catheter removal (C.Table 1) depend on the clinical condition of the patient and the type of organism causing the infection. C. Table 1. Indications for removal of long-term catheters: Cellulitis at the catheter exit site (depending on the severity of infection) Severe sepsis without a focus Page 5 of 8 Thrombophlebitis Endocarditis Persistent bacteremia for 72 hours despite appropriate treatment Infection with species of Corynebacterium, Bacillus, Micrococcus, Enterococcus, and Mycobacterium Fungal infections D. Summary All variables must be evaluated when deciding whether to remove a longterm catheter in a child with cancer. The most important factors to be considered are the age of the patient, the type of infection, the pathogen involved, and the clinical condition of the patient. The indications for the removal of a permanent catheter can be divided into 2 categories on the basis of the factors mentioned above. Where there is no controversy about the indication the indication has to be adapted according to the clinical situation at hand) (D.Table 1). D. Table 1. Summary of the indications for removal of implantable catheters in children. Absolute Indications 1. Severe sepsis 2. Cellulitis 3. Candidal infection 4.Endocarditis 5.Thrombophlebitis 6. Failure of medical treatment 7. Mycobacterial infection 8. Fungal infection Relative Indications Page 6 of 8 9. Infection with Staphylococcus aureus 10. Infection with gram-negative bacilli 11. Infection with species of Enterococcus, Bacillus, Corynebacterium, Propionibacterium, and Micrococcus E. Bibliography 1 Mermel LA, Allon M, Bouza E et al. Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 2009;49:1–45 2 Maki DG, Mermel LA. Infections due to infusion therapy. In: Bennett JV, Brachman PS, eds. Hospital infections. Philidelphia, PA: Lippincott-Raven, 1998:689–724 3 O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep 2002; 51:1–29 4 Safdar N, Mermel LA, Maki DG. The epidemiology of catheter-related infection in the critically ill. In: O’Grady N, Pittet D, eds. Catheter-related infections in the critically ill. New York, NY: Kluwer, 2004:1–23. 5 Ekkelenkamp MB, van der Bruggen T, van de Vijver DA, Wolfs TF, Bonten MJ. Bacteremic complications of intravascular catheters colonized with Staphylococcus aureus. Clin Infect Dis 2008; 46:114–8 6 Piedra PA, Dryja DM, LaScolea LJ Jr. Incidence of catheter-associated gram-negative bacteremia in children with short bowel syndrome. J Clin Microbiol 1989; 27:1317–9 7 Flynn PM, Shenep JL, Stokes DC, Barrett FF. In situ management of confirmed central venous catheter-related bacteremia. Pediatr Infect Dis J 1987; 6:729–34. 8 Dato VM, Dajani AS. Candidemia in children with central venous catheters: role of catheter removal and amphotericin B therapy. Pediatr Infect Dis J 1990; 9:309–14 9 Castagnola E, Marazzi MG, Tacchella A, Giacchino R. Broviac catheter-related candidemia. Pediatr Infect Dis J 2005; 24:747 10 Stovroff M, Teague WG. Intravenous access in infants and children. Pediatr Clin North Am 1998; 45:1373–93, viii 11 Fowler VG Jr, Justice A, Moore C, et al. Risk factors for hematogenous complications of intrava scular catheterassociated Staphylococcus aureus bacteremia. Clin Infect Dis 2005; 40:695–703. Page 7 of 8 12 Sandoe JA, Witherden IR, Au-Yeung HK, Kite P, Kerr KG, Wilcox MH. Enterococcal intravascular catheterrelated bloodstream infection: management and outcome of 61 consecutive cases. J Antimicrob Chemother 2002; 50:577–82 13 Seifert H, Strate A, Pulverer G. Nosocomial bacteremia due to Acinetobacter baumannii. Clinical features, epidemiology, and predictors of mortality. Medicine (Baltimore) 1995; 74:340–9. 14 Elting LS, Bodey GP. Septicemia due to Xanthomonas species and non-aeruginosa Pseudomonas species: increasing incidence of catheter-related infections. Medicine (Baltimore) 1990; 69:296–306. 15 Karlowicz MG, Hashimoto LN, Kelly RE Jr, Buescher ES. Should central venous catheters be removed as soon as candidemia is detected in neonates? Pediatrics 2000; 106:E63 16 Oudiz RJ, Widlitz A, Beckmann XJ, et al. Micrococcus-associated central venous catheter infection in patients with pulmonary arterial hypertension. Chest 2004; 126:90–4. 17 Khan EA, Correa AG, Baker CJ. Suppurative thrombophlebitis in children: a ten-year experience. Pediatr Infect Dis J 1997; 16:63–7 18 Centers for Disease Control and Prevention. Update: delayed onset Pseudomonas fluorescens bloodstream infections after exposure to contaminated heparin flush—Michigan and South Dakota, 2005–2006. MMWR Morb Mortal Wkly Rep 2006; 55:961–3. 19 Almuneef MA, Memish ZA, Balkhy HH, Hijazi O, Cunningham G, Francis C. Rate, risk factors and outcomes of catheter-related bloodstream infection in a paediatric intensive care unit in Saudi Arabia. J Hosp Infect 2006; 62:207–13 20 Wiener ES, McGuire P, Stolar CJ, et al. The CCSG prospective study of venous access devices: an analysis of insertions and causes for removal. J Pediatr Surg 1992; 27:155–63; discussion 63–4 Page 8 of 8