* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download High dose intravenous immunoglobulin treatment: Mechanisms of
Survey
Document related concepts
Transcript
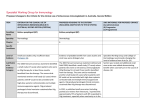
REVIEW High Dose Intravenous Immunoglobulin Treatment: Mechanisms of Action Peter Boros,1 Gabriel Gondolesi,1 and Jonathan S. Bromberg1,2 Intravenous immunoglobulin (IVIg) treatment was introduced as replacement therapy for patients with antibody deficiencies, but evidence suggests that a wide range of immune-mediated conditions could benefit from IVIg. The immunoglobulins are precipitated from human plasma by fractionation methods. In conclusion, the differences in basic fractionation methods and the addition of various modifications for purification, stabilization, and virus inactivation result in products significantly different from each other. (Liver Transpl 2005;11:1469-1480.) patient and are believed to correct immune dysregulation. Immunomodulatory and anti-inflammatory properties associated with IVIg administration are based on multiple connected and synergistic mechanisms. Here, we review the potential immunologic mechanisms of action, with particular emphasis on the use of IVIg in organ transplantation. The mode of action of IVIg depends largely on antigen binding and modification of effector functions. Antigen binding is mediated via immune antibodies and a wide spectrum of autoantibodies. The effector functions include modulation of expression and function of Fc receptors, complement activation, complement binding, anti-inflammatory effects ensuing from interference with the cytokine network, provision of anti-idiotypic antibodies, and modulation of T- and B-cell activation. Organ transplantation is an important field for IVIg treatment, primarily for patients with high titers of anti-HLA antibodies. Intravenous immunoglobulin (IVIg) treatment was introduced in the 1950s as replacement therapy for patients with congenital antibody deficiencies. Clinical and experimental evidence accumulated since then suggests that a wide range of immune-mediated conditions could benefit from IVIg, including acute and chronic/ relapsing diseases, autoimmune diseases mediated by pathogenic autoantibodies, or by autoaggressive T cells, as well as inflammatory disorders. IVIg treatment of immunodeficiency delivers missing immune antibodies against pathogens. This form of treatment is aimed at substitution or passive immunization against multiple bacteria and viruses. The use of IVIg in hyperactive conditions of the immune system is not as widely accepted, although the efficacy of IVIg treatment has been demonstrated in several autoimmune diseases.1-4 IVIg preparations are fractionated from a plasma pool of healthy donors and contain both immune antibodies and physiologic autoantibodies. As immune antibodies reflect the immunologic experience of the donor population, this component is utilized for replacement therapy and passive immunization. Natural autoantibodies react with the immune system of the Production and Properties of IVIg Preparations Several different IVIg formulations are licensed in the USA and Europe. The production process might affect composition and properties, alter tolerability, and ultimately modify therapeutic effects. IVIg is prepared from pools of plasma from up to 100,000 (a minimum of 3,000) healthy blood donors, and it is assumed that IVIg contains the entire array of variable regions of antibodies that would be present in normal serum. The large number of donors in the pool adds more individual activities to the IVIg preparation; however, it carries the risk of diluting out any useful activity that is rare. Preparation of IVIg The immunoglobulins are precipitated from human plasma by fractionation methods using ethanol. While Abbreviations: IVIg, Intravenous immunoglobulin; HIV, human immunodeficiency virus; HTLV, human T cell lymphotropic retrovirus; GPI glycosylphosphatidylinositol; Th1, T helper 1; IL-1ra, interleukin-1 receptor antagonist; IL-1, interleukin-1; HBV, Hepatitis B virus; CMV, Cytomegalovirus; CIg, Cytomegalovirus immunoglobulin. From the 1Recanati/Miller Transplantation Institute, The Mount Sinai School of Medicine, New York, NY; and 2Department of Gene and Cell Medicine, The Mount Sinai School of Medicine, New York, NY. Received March 15, 2005; accepted August 17, 2005. Address reprint requests to Peter Boros, Recanati/Miller Transplantation Institute, The Mount Sinai School of Medicine, POB 1504, New York, NY, 100229-6574. Telephone: (212) 241-5589; FAX: (212) 426-2233; E-mail: [email protected] Copyright © 2005 by the American Association for the Study of Liver Diseases Published online in Wiley InterScience (www.interscience.wiley.com). DOI 10.1002/lt.20594 Liver Transplantation, Vol 11, No 12 (December), 2005: pp 1469-1480 1469 1470 Boros et al. the early products could not be administered intravenously as they contained aggregates and other impurities capable of activating complement and causing severe reactions, processing modifications developed over the years ensure the stability and purity of preparations.5 Today’s IVIgs, suitable for intravenous administration, contain high levels of intact IgG, display normal distribution of IgG subclasses, and have only small concentrations of dimers. Further modifications involving specific virus inactivation or removal (solvent/detergent treatment, low pH incubation, ultrafiltration, and pasteurization) made these products even safer. The differences in basic fractionation methods and the addition of various modifications for purification, stabilization, and virus inactivation resulted in products significantly different from each other with respect to chemical structure, antibody content, subclass distribution, and electrophoretic profile. When commercial products are compared for antibody activity to various bacteria such as Staphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli, and group B Streptococcus, they were found to have differences and inconsistencies among batches and formulations, with some of the products showing reduced opsonization activity.6-8 Different production procedures have also been shown to affect Fc receptor activity9 or complement fixation,10 which can influence the protective effects of IVIg in patients with antibody deficiency. These factors may significantly affect clinical outcome in treated patients. There is an important distinction between standard pooled IVIg (derived from the plasma of unselected normal donors) and hyperimmune immunoglobulins. To prepare hyperimmune immunoglobulins, donors are selected for high levels of reactivity to specific pathogens. Those samples are specially selected, pooled, and immunoglobulin derived from them is used to manufacture specific products to treat or prevent diseases such as cytomegalovirus, respiratory syncytial virus, hepatitis B, tetanus, and varicella. Properties of IVIg Preparations General Characteristics The Food and Drug Administration currently approves eight IVIg preparations for use in the United States. Preparation methods as mentioned vary somewhat, but the final product is purified IgG, with traces of IgM. Half-lives, may range from 21 to 33 days, and pH may also vary, which may be relevant for acid-base balance in certain patients. Products can also differ with respect to the composition of stabilizers (e.g., maltose, sucrose, and mannitol), which may significantly affect their osmolality. Some IVIg preparations are shipped in liquid form, while others are shipped in lyophilized form and reconstituted at the time of infusion. The risk of transmission of infectious disease is a concern whenever blood derivatives are prepared from large numbers of donors. Safety standards for viral pathogens include plasma testing of both individual donations and pools, all products are tested for human immunodeficiency virus (HIV), hepatitis B, hepatitis C, and human T cell lymphotropic retrovirus (HTLV). Solvent/detergent treatment inactivates enveloped viruses, such as HIV, while several other aggressive processing steps including treatment with trypsin, pasteurization, nano-filtration, and low pH are used to remove or inactivate additional pathogens. These steps are complementary and increase overall safety by providing the widest possible safety margin against known and unknown viruses. Wide variations have been reported regarding the risk of transmission of hepatitis C. Some preparations, including Gammagard and Polygam, both prepared by fractionation and chromatographic purification, were implicated in over 100 cases worldwide.11 Today, validated industrial-scale viral inactivation and removal methods mentioned above are being used in the manufacturing processes of the available IVIg preparations. Combined with vigorous donor screening, plasma testing, and quality control procedures, these steps have greatly minimized the risk of hepatitis C transmission.12 Components Sugar Content To prevent aggregate formation, sugars such as sorbitol, glucose, and sucrose are added to IVIg preparations. The major, albeit rare, complication associated with sugar content is acute renal failure or insufficiency as more than 90% of the IVIg-associated adverse renal events in the United States occurred with sucrose-containing IVIg preparations.13 Nephrotoxicity can be a serious complication of IVIG therapy. Preexisting renal disease, volume depletion, and old age are risk factors for such toxicity. A recent analysis reported that a high percentage of these patients required hemodialysis, and mortality occurred in 10-15%.14 Sodium Content The sodium content, ranging from trace amounts to 0.9%, determines the osmolality of the infused solution 1471 IVIg Treatment Table 1. IVIg Products Sugar content Product Manufacturer Viral inactivation IgG IgA IgM pH Venoglobulin-S solvent/detergent ⬎99% 15–20 g/ml 10–40 g/ml 5.2–5.8 Panglobulin Alpha Therapeutic ARC ⱖ96% ⬎970 g/ml ⬎20 g/ml 6.4–6.8 Polygam ARC pH 4, pepsin, filtration solvent/detergent 5% Dsorbitol 5% sucrose ⱖ90% ⬍3.7 g/ml trace 6.4–7.2 2% glucose Gammagard Baxter Healthcare Bayer solvent/detergent ⱖ90% ⬍3.7 g/ml trace 6.4–7.2 2% glucose pH 4.2, solvent/ detergent Pasteurization ⱖ98% trace trace 4–4.5 None ⱖ98% 25–50 g/ml 20–50 g/ml 6.4–7.2 5% sucrose trypsin, PEG 100% ⬍2 g/ml trace 6.4–6.8 5% glucose pH 4, pepsin, filtration ⱖ96% ⬍970 g/ml ⬍20 g/ml 7 5% sucrose Gamimmune Gammar-P Iveegam Carimmune Aventis Behring Baxter Healthcare ZLB Bioplasma and thus can affect tolerability and occurrence of adverse events. Osmolality Osmolality in different IVIg solutions may range from physiologic values (280-296 mOsm/l) to greater than 1,000 mOsm. Hyperosmolar solutions may cause fluid shifts and the occurrence of infusion-related adverse events. pH The optimal pH to prevent aggregation is 4.0 to 4.5. Low-pH preparations are instantaneously neutralized by the buffering capacity of blood on infusion. Many IVIg products have a final pH that is close to neutral (a pH of 7.0-7.5) or in the range of 6 to 7, requiring the addition of different agents to maintain stability and prevent aggregation. IgA Content A principal clinically significant difference among IVIg products is the presence or absence of IgA. Some patients are IgA-deficient, so it is extremely important that their IgA levels be measured before receiving the first IVIg treatment. IgA-deficient patients may develop immunity to IgA and are at increased risk of anaphylaxis if they receive a blood product that contains IgA. Several methods have been developed to prevent anaphylaxis; both ex vivo pretreatment of the IVIg preparation with autologous plasma or subcutaneous injection of the IVIg allow safe management of patients even with high anti-IgA titers.15,16 Osmolarity 300–330 mOsm/l 192–768 mOsm/l 663–1,326 mOsm/l 636–1,250 mOsm/l 274 mOsm/l 330–600 mOsm/l 375 mOsm/l 192–768 mOsm/l Isohemagglutinin Antibodies Preparations of IVIg contain low titers of anti-A, anti-B, anti-C, and anti-E blood group antibodies. Mild, self-limiting hemolysis due to residual anti-A and anti-B antibodies may regularly occur. Serious hemolysis has been reported only with hyperimmune preparations.17 Table 1 summarizes some of the main characteristics of primary IVIg products. Mechanisms of Action of IVIg The extensive range of effects associated with IVIg treatment reflects the functions of circulating immunoglobulins in the maintenance of tolerance to self and immune homeostasis in healthy individuals. The mode of action of IVIg is complex, but efficacy depends on two general types of mechanism: antigen binding and modification of various effector functions. Antigen binding is mediated by the Fab part. The effector functions include binding to the various Fc receptors resulting in modulation of expression and function of Fc receptors, complement activation, complement binding, anti-inflammatory effects resulting from interference with the cytokine network, provision of anti-idiotypic antibodies, and modulation of T and B-cell activation.1-4,18-23 It should be emphasized that these mechanisms overlap, and the outcome of IVIg treatment manifests as a combination of many different effects. Antigen Binding Natural Antibodies These antibodies are mostly IgM, but can also be of the IgG or IgA classes, and are not the result of an 1472 Boros et al. immune response because they are also present in embryos as well as in animals raised under sterile conditions.24,25 Natural antibodies have been shown to prevent the spreading of pathogens into the brain and the kidneys, and can therefore be considered as “first-line defense” antibodies, and elements of the innate immune system.26 Natural autoantibodies can be autoreactive and be part of the “first-line defense” at the same time. The peripheral control of natural autoantibody production occurs through their Fab portions or idiotypes. In turn, these Fab parts are recognized by other natural anti-idiotypic autoantibodies. Natural autoantibodies bind to both pathogens and complement factors, and promote the uptake of pathogens by antigen-presenting cells. Consecutively, this may facilitate an effective adaptive immune response against pathogen-specific epitopes, while the development of autoimmunity is prevented.27 CD4-positive T cells by human immunodeficiency virus.33 Natural anti-MHC class I antibodies block the function of CD8 T cells in vitro.34 Natural “First-Line Defense” Antibodies Sera of healthy individuals, and therefore all IVIg preparations, contain physiologic autoantibodies directed against an wide range of cytokines (IL-6, IL-1, TNF-␣, IL-8, and GM-CSF).41-43 These antibodies are partially responsible for the anti-inflammatory activities of IVIg by neutralizing pro-inflammatory cytokines. Superantigens may trigger the activation of autoreactive cells in an MHC unrestricted manner. IVIg contains antibodies to superantigens such as TSST-1 and Staphylococcal enterotoxins. Autoimmune diseases have often been associated with bacterial or viral superantigens, which may accelerate such conditions. Thus, anti-superantigen antibodies can be considered as immunomodulatory resulting in the elimination of pathogens.28 Physiologic Autoantibodies Against AntigenBinding Structures IVIg may contain natural autoantibodies directed against the idiotype, the hinge region, the constant heavy chain 1, and the constant light chain domains of antibodies. The anti-idiotype antibodies bind pathogenic autoantibodies in vitro, suggesting that they might also be able to prevent binding to autoantigens under in vivo conditions.29,30 Anti-idiotype autoantibodies may also bind to variable regions of antigen receptors, rendering B and T cell activation by autoantigens impossible. Physiologic autoantibodies against the variable region of the T-cell receptor block autoantigen-mediated T-cell activation resulting in long-term T-cell down-regulation.31,32 CD4 and MHC Class I-Specific Autoantibodies Natural autoantibodies against both CD4 and MHC class I have been detected in IVIg preparations. In vitro, natural anti-CD4 antibodies block T-cell proliferation in mixed lymphocyte cultures and the infection of Autoantibodies Against the Fas Receptor IVIg preparations contain natural anti-Fas receptor autoantibodies that block Fas ligand/Fas receptor interactions and prevent keratinocyte apoptosis.35,36 This explains the beneficial effects of IVIg treatment in patients with toxic epidermal necrolysis, a condition where keratinocytes are highly sensitized toward Fas ligand-mediated apoptosis.37 The titers of Fas inhibitory antibodies vary from batch to batch similar to the anti-microbial antibodies. Agonistic anti-Fas receptor autoantibodies have also been detected in IVIg preparations.38 These antibodies might support anti-inflammatory effects by promoting apoptosis of activated T cells or neutrophils.39,40 Cytokine-Specific Natural Autoantibodies Effector Functions IVIg preparations have been shown to exhibit antiinflammatory properties in patients with diseases associated with a hypersensitive immune system. Many in vitro and also in vivo data suggest a number of potential mechanisms of action. Activation/Blockade of Fc Receptors IgG Fc receptors (Fc␥Rs) are immunoglobulin superfamily members and are of 3 main types: Fc␥RI (CD64), Fc␥RII (CD32), and Fc␥RIII (CD16). All of these are integral transmembrane glycoproteins, with the exception of Fc␥RIIIB, which is expressed as a glycosylphosphatidylinositol (GPI)-linked molecule on neutrophils. Most of the Fc␥Rs are of the activating type, and receptor engagement leads to a variety of functions depending on the type of effector cell, including phagocytosis, degranulation, antibody-dependent cell-mediated cytotoxicity, cytokine release, and regulation of antibody production. Importantly, both mice and human beings also express the inhibitory Fc␥R, Fc␥RIIB, which contains inhibitory motifs in the cytoplasmic domain, and whose ligation down regulates these cellular functions. Humans express other forms of Fc␥RII, namely, Fc␥RIIA and Fc␥RIIC, that deliver IVIg Treatment activating signals, while mice express only the inhibitory form, Fc␥RIIB.44-47 IgG molecules bind via their Fc region to Fc receptors on macrophages, neutrophils, eosinophils, platelets, mast cells, natural killer cells, and B cells. The Fc region of the antibody interacts with hematopoietic cells to disable or up-regulate cellular activities depending on the Fc receptor types. It is widely accepted that treatment of idiopathic thrombocytopenic purpura and other autoantibody-induced cytopenias by IVIg is mechanistically mediated by the blockade of the Fc receptor on macrophages, which prevents the removal of sensitized platelets by the reticuloendothelial system.48 Attenuation of Complement-Mediated Damage IVIg binds the activated components C3b and C4b in a C1q-independent and C1q-dependent fashion. By scavenging these active complement components and diverting complement attack from cellular targets, IVIg prevents the generation of the C5b-9 membrane attack complex, the deposition of the complex on target surfaces, and subsequent complement-mediated tissue damage.49 In addition, natural anti-C3b autoantibodies have been identified that inhibit C3 convertase activity in vitro.50 This mode of action of IVIg is of significance in the treatment of patients with severe dermatomyositis, Guillain-Barre syndrome, and myasthenia gravis. Neutralization of Pathogenic Autoantibodies and the Regulation of Autoreactive B-Cell Clones Inhibition of autoantibody activity by IVIg has been observed in the case of autoantibodies to factor VIII, thyroglobulin, DNA, intrinsic factor, peripheral nerve, cytoplasmic antigens of neutrophils, platelet gpIIb/IIIa, the acetylcholine receptor, endothelial cells, phospholipids, nephritic factor, and retinal autoantigens.51. Presence of anti-idiotypes to disease-associated autoantibodies may be relevant in explaining the efficacy of IVIg in myasthenia gravis, Lambert-Eaton myasthenia syndrome, and antibody-mediated neuropathies.52 Induction of Anti-Inflammatory Cytokines Modulation of the production of cytokines and cytokine antagonists is a major mechanism by which IVIg exerts its anti-inflammatory effects in vivo in various neuromuscular disorders such as inflammatory myopathies, demyelinating neuropathies, and myasthenia gravis.3,4. The anti-inflammatory effects of IVIg involving modulation of cytokine production are not restricted to monocytic cytokines but are also reliant on the ability of 1473 IVIg to increase T helper 1 (Th1) and Th2 cytokine gene expression and production.53 IVIg selectively triggers the production of interleukin-1 receptor antagonist (IL-1ra), the natural antagonist of interleukin-1 (IL-1), in cultures of purified monocytes, without affecting the production of the proinflammatory cytokines IL-1␣, IL-1, IL-6, and TNF-␣.54 IVIg and Dendritic Cells Alteration in the phenotype and function of dendritic cells (DC) may explain, at least partially, the systemic autoimmune responses that characterize systemic lupus erhythematosus (SLE). HLA-DR⫹, CD4⫹ B7⫹ and CD40⫹ DC are less frequent in SLE patients than in control individuals. Functional analysis of DC from SLE patients discovered diminished allogeneic and antigen-specific T cell-stimulatory capacity compared with healthy controls.55 IVIg interferes with the differentiation of DC from SLE patients and from healthy donors cultured in the presence of SLE sera in vitro, and reduces the capacity of mature DC to secrete IL-12 upon activation, while enhancing IL-10 production. IVIg-treatment of DC also inhibits the ingestion of nucleosomes by immature DC. IVIg induced downregulation of co-stimulatory molecules CD80/CD86 and modulation of cytokine secretion from DC, which in turn resulted in the inhibition of auto-and allo-reactive T cell activation and proliferation.56,57 The inhibition of expression of co-stimulatory molecules on DC by IVIg offers a possible explanation for the efficacy of IVIg in other immuno-inflammatory conditions, such as autoimmune diseases and transplantation. Recent Advances in Understanding the Mechanism of IVIg Fc␥R-s with intracellular immune receptor tyrosinebased activation motifs (ITAM or activating receptors) mediate inflammatory effector functions. Cytokines are known to regulate Fc␥R expression on monocytes and neutrophils. Th1 cytokines (TNF-␣ and IFN-␥) upregulate and activate various FcRs, while Th2 (IL-4 and IL-13) cytokines up regulate the inhibitory FcR (FcRIIB). IVIg induces both IL-4 and lL-13, and induces FcRIIB leading to anti-inflammatory effects.58,59 Thus, IVIg mediates in part its anti-inflammatory effect by up regulating the FcRIIB, which has a negative effect on the inflammatory cascade (in contrast to FcRI, III, IIA, and C). The importance of FcRIIb for the therapeutic effect of IVIg has been directly suggested based on data from a mouse model of idiopathic 1474 Boros et al. thrombocytopenia. Fc␥RIIB was required for IVIg to exert its protection, because disruption either by genetic deletion or with a blocking monoclonal antibody reversed the therapeutic effect of IVIg.60 IVIg may also influence the differentiation of new monocytes/macrophages by IgG-IgG dimers, which usually do not exist in the circulation, by shifting the balance between inhibitory and activating receptors on monocytes/macrophages. In hypogammaglobulinemic patients with reduced occupation of Fc␥ receptors, infusion of IVIg can result in the release of pro-inflammatory and subsequently anti-inflammatory cytokines.61,62 IgG-IgG dimers present in IVIg are responsible for this phenomenon and the absence of polymers in IVIg preparations may prevent cytokine release.63 Dimers may be responsible for many adverse effects associated with IVIg treatment.64-66 IVIg have also been reported to accelerate autoantibody catabolism by binding to an Fc receptor called “FcRn” on endothelial cells. If IgG is pinocytosed and binds in a low pH milieu to FcRn, the immunoglobulin is protected from lysosomal degradation. IVIg treatment may result in the saturation of FcRn receptors, and through competition prevents pathogenic autoantibodies from binding, with the consequence of their accelerated degradation. This hypothesis was supported by a recent animal model, where, in FcRn knockout mice, IVIg did not increase the clearance of a monoclonal anti-platelet anti-body, while in the wild-type animals it did.67,68 IVIg is capable of reversing the steroid resistant state. Steroid resistance has been observed in asthma, SLE, inflammatory bowel diseases, and transplant rejection. In these patients, lymphocyte activation (thymidine uptake in the presence of PHA) is not suppressed in the presence of steroids. Five percent of the cases of steroid resistance are genetic and 95% are acquired. In patients unresponsive to glucocorticoids, a resistant isoform (GR-) of the steroid receptor can be detected. IVIg reverses steroid resistance state by reducing the binding affinity of GR- to glucocorticoids.69,70 New promising products have been designed and introduced. Recently, anti-dsDNA idiotypes were affinity purified from sera of SLE patients and were used to isolate natural polyclonal anti-dsDNA anti-idiotypic antibodies from IVIg preparations. These antibodies improved the clinical manifestations of SLE in (NZBxW)F1 mice in very low concentrations. The lupus specific IVIg was introduced to a peptide phage display library (C-7mer-C). The identified synthetic peptides (idiotype mimetics) were synthesized and used to replace the original human anti-dsDNA idiotype column. Molecules affinity purified on the synthetic peptide column from IVIg were determined as psIVIg (peptide specific IVIg). These peptide-specific IVIgs decreased the titer of circulating anti-dsDNA antibodies, and improved leucopenia, proteinuria, and immunoglobulin depositions in the kidneys, when injected into mice with experimental SLE significantly greater than conventional IVIg.71 It is possible that many of the discussed mechanisms are not mutually exclusive and may contribute to the success of IVIg therapy in different diseases. It has been also suggested that some immunoregulatory effects of IVIg are not due to the immunoglobulin fraction itself but may be due to “contaminating” products present in the product such, as growth factors.72It is very likely that neither B cells, T cells, nor their cytokines are required for the immediate/short-term protective effect of IVIg. Our understanding of the mechanisms of IVIg is expected to grow primarily regarding the medium and long-term effects on the immune system. As we discussed, IVIg affects both cytokines and cytokine receptor levels. IL-2 is a key cytokine in the immune response whose function is inhibited by IVIg. This inhibition appears to be upstream of IL-2 secretion, at a posttranscriptional level.73 There are additional possible mechanisms for IVIg-induced changes in cellular immunity. There is increasing understanding of the immunological role of human regulatory T cells (Treg), but the direct effect of IVIg on this cell population is not known. While IVIg evidently inhibits T-cell proliferation and T cell cytokine production, it is not completely clear to what extent these effects are dependent on the direct effects of IVIg on T cells or if they occur mostly through the inhibition of antigen-presenting cell activity including altered DC function. The study of the IVIg mediated inhibitory signaling pathways on specific cells, including T and B cells and monocytes, is also an area where further explorations are needed. IVIg Treatment in Organ Transplantation Highly Sensitized Patients The presence of antibodies of the IgG isotype, directed against the HLA class I molecules presented by the graft, correlates with episodes of severe acute rejections and ultimate graft loss. These antibodies are demonstrated by “crossmatch”, when the serum of the recipient is incubated with lymphocytes from the donor, and the potential binding exposed either through cytotoxicity with complement or through flow cytometry. The positivity of a classical cytotoxic T cell IgG crossmatch IVIg Treatment was considered an absolute contra-indication for transplantation. A crossmatch positive by only flow cytometry does not rule out transplantation, but these patients experience a significantly higher frequency of acute rejections, with more severe lesions representing vasculitis. Reactivity of the actual serum sample obtained from a patient on the waiting list is determined on a panel of human cells representing the major HLA determinants. Highly sensitized patients, making up close to 30% of waiting lists, often have to wait prolonged periods for suitable organs and are at risk for early rejection and/or graft failure. Different IVIg preparations are used to treat prospective recipients who display high titers of donor specific anti-HLA antibodies. IVIg alone or in combination with plasmapheresis, anti-lymphocyte antibody, or immunoadsorption techniques coupled with immunosuppressive agents effectively desensitizes these patients, shortens waiting time, and facilitates transplantation74-77 as demonstrated by multiple studies in kidney and heart transplantation. The mechanism may involve a direct effect on circulating IgG anti-HLA immunoglobulins, as naturally occurring anti-idiotypic antibodies to HLA, which are also present in pooled human IVIg, improve graft survival.30,78 IVIg has also been demonstrated to stimulate the production of anti-idiotypic IgM blocking antibodies. Soluble HLA class I molecules may transiently reduce anti-HLA activity by binding to circulating anti-HLA antibodies in the recipient.79,80 IVIg may also induce B cell apoptosis.81 The beneficial effect of pre-transplant IVIg treatment is further strengthened by a recent doubleblinded placebo-controlled multi-center study in kidney patients. The treatment consisted of IVIg 2 g/kg monthly for 4 months or an equivalent volume of placebo. At baseline, the levels of panel reactive antibodies (PRA) were similar. IVIg significantly reduced PRA levels compared with placebo. The decrease in antiHLA antibody levels was sustained, and a significantly higher percentage of patients could be transplanted in the IVIg group (35 % vs. 17%). With a median follow-up of 2 years, the viable transplants functioned normally, and the frequency adverse events rates was similar.82 In addition to kidney and heart recipients, an ongoing study at our institution examines the use of IVIg in highly sensitized patients awaiting small bowel transplantation. Isolated intestinal transplant (IIT) is preferable over multi-organ procedures for its typically better outcome. A positive crossmatch in highly sensitized patients on the intestinal waiting list is also considered contraindication for IIT, as extensive graft damage or 1475 graft loss may develop due to humoral rejection.83 Several our patients have undergone desensitization using various doses of IVIg (depending on the level of PRA). A sustained reduction of PRA and, in some cases, negative crossmatch was achieved, and the patients were successfully transplanted.84 This approach may facilitate earlier IIT in highly sensitized individuals who would otherwise be offered multi-organ transplant after they develop liver failure. IVIg may also be administered at the time of transplantation for prevention of acute rejection. IVIgs have been used for prophylaxis of acute rejection in hyperimmunized patients, including multi-organ procedures performed in children as well as second transplants. In hyperimmunized patients, post-transplant administration of IVIg (0.4 g/kg for the first 5 days after transplantation in addition to an immunosuppressive regimen resulted in graft survival superior (95% at 2 years) to typical results for this group of patients (approximately 80%).85 In a randomized study using IVIgs as prophylaxis for acute rejection, patients receiving 0.4 g/kg per day from day 0 to day 5 with a quadruple immunosuppressive regimen had a significantly higher 5-year graft survival rate (68%, vs. 50% in the control group).86 In addition to these studies in kidney transplantation, a similar study in heart transplant patients demonstrated that the graft survival in immunized patients treated with IVIgs and plasmapheresis was identical to the survival of non-immunized patients.87 IVIg preparations may also be useful in the treatment of established rejection, particularly when antilymphocyte antibody therapy is considered too risky. In a study of 30 steroid-resistant rejections, IVIg treatment rescued over 70% of the grafts, without the wellknown side effects of OKT3.88 In addition to other mechanisms described above, the beneficial effect of IVIg in rejection may arise from neutralization of circulating anti-endothelial antibodies or by blocking endothelial cell activation of the vascular lesions.89,90 IVIg is increasingly used to facilitate the transplantation of ABO incompatible organs such as kidney, lung, and heart. Generally, IVIg is administered in combination with immunosuppression, immunoadsoption, and plasmapheresis, and it is infused during the immediate pretransplant period.91,92 Successful treatment with IVIg of antibody-mediated rejection following ABO-incompatible liver transplantation has also been reported.93 In liver transplantation, IVIg is an important therapeutic option in prevention of Hepatitis Bvirus (HBV) recurrence. The introduction of high-dose HBIg for long-term prophylaxis of HBV recurrence in patients receiving transplants for HBV-related cirrhosis resulted 1476 Boros et al. in survival rates comparable with those of liver transplants for other indications.94 While lamivudine is a potential alternative to HBIg, lamivudine monotherapy has not proved satisfactory. As a combination therapy, high doses of HBIg (5,000 IU) can be given during the first 6 months post-transplant, followed by lamivudine monotherapy. Recently, the use of low-dose HBIg (2,000 IU) in association with lamivudine for long-term maintenance has been recommended.95,96 Considering the high cost of HBIg treatment, other groups suggests serial anti-HBs antibody titer determinations, which allows the identification of the optimal timing for HBIg administration. This individualized “on demand” approach appeared to be successful in preventing recurrence over a 2-year period, and proved to be cost-effective.97 IVIg and CMV infections in liver transplant patients. Cytomegalovirus (CMV) infection emerged as a serious problem for patients immunocompromised by organ transplantation. Cytomegalovirus immunoglobulin (CIg) was licensed in 1991 and has regularly been utilized to reduce CMV morbidity and mortality. Treatment is expensive and does not always prevent serious CMV disease. Several studies demonstrate that CIg infusion reduces serious CMV infections associated with liver transplants and improves survival of infected patients.98,99 Reducing transplantation of organs from CMV-positive donors to CMV-negative recipients would be ideal but is usually not attainable. Recent results demonstrate that adding prophylactic ganciclovir further reduces infection rates and improves survival and clinical outcomes.100-103 Additional areas for IVIg treatment in liver transplant patients include idiopathic thromocytopenic purpura (ITP), which was reported following both cadaveric and living-related transplants.104,105 Successful post-transplant treatment of chronic inflammatory demyelinating polyradiculoneuropathy observed in patients undergoing liver transplantation has also been described.106 A recent addition to the indications for IVIg therapy is post-transplant hypoglammaglubulinemia. This condition is being increasingly reported in liver, lung, and heart transplant patients.107-109 The exact mechanism is not clear, although heavy immunosuppression is likely to play a role. Serious hypoglammaglubulinemia (IgG ⬍ 350-400 mg/dL) is associated with increased incidence of viral, fungal, and bacterial infections, in certain cases an increased risk of rejection, and ultimately poorer outcomes. Pre-emptive treatment appears to be beneficial, and the use of IVIg in post- transplant hypogammaglobulinemia is viewed as an accepted indication at several centers.110 Perspective It is possible that many of the discussed mechanisms are not mutually exclusive and may contribute to the success of IVIg therapy in different diseases. It has been also suggested that some immunoregulatory effects of IVIg are not due to the immunoglobulin fraction itself but may be due to “contaminating” products present in the product such, as growth factors. It is very likely that neither B cells, T cells, nor their cytokines are required for the immediate/short term protective effect of IVIg. Our understanding of the mechanisms of IVIg is expected to grow primarily regarding the medium and long-term effects on the immune system. As we discussed, IVIg affects both cytokines and cytokine receptor levels. IL-2 is a key cytokine in the immune response whose function is inhibited by IVIg. This inhibition appears to be upstream of IL-2 secretion, at a posttranscriptional level. There are additional possible mechanisms for IVIg-induced changes in cellular immunity. There is increasing understanding of the immunological role of human regulatory T cells (Treg), but the direct effect of IVIg on this cell population is not known. While IVIg evidently inhibits T cell proliferation and T cell cytokine production, it is not completely clear to what extent these effects are dependent on the direct effects of IVIg on T cells or if they occur mostly through the inhibition of antigen-presenting cell activity including altered DC function. The study of the IVIg mediated inhibitory signaling pathways on specific cells, including T and B cells and monocytes, is also an area where further explorations are needed. Although the exact mechanisms of action are not fully understood, high-dose IVIg is an extremely valuable treatment option for a number of autoimmune diseases as well as in patients with autoimmunity, allergy, or special transplant-related problems who do not respond to conventional therapies. References 1. Kazatchkine MD, Kaveri SV. Immunomodulation of autoimmune and inflammatory diseases with intravenous immune globulin. N Engl J Med 2001;345:747-755. 2. Dwyer JM. Manipulating the immune system with immune globulin. N Engl J Med 1992;326:107-116. 3. Dalakas MC. Intravenous immune globulin therapy for neurologic diseases. Ann Intern Med 1997;126:721-730. 4. Yu Z, Lennon V. Mechanism of intravenous immune globulin IVIg Treatment 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. therapy in antibody-mediated autoimmune diseases. N Engl J Med 1999;340:227-228. Nielsen H. Immunoglobulin preparations for intravenous administration. Allergy 1994;49:69-73. van Furth R, Leijh PC, Klein F. Correlation between opsonic activity for various microorganisms and composition of gammaglobulin preparations for intravenous use. J Infect Dis 1984; 149:511-517. Givner LB. Human immunoglobulins for intravenous use: comparison of available preparations for group B streptococcal antibody levels, opsonic activity and efficacy in animal models. Pediatrics 1990;86:955-962. Skvaril F, Roth-Wicky B, Barandum S. IgG subclasses in human gamma-globulin preparations for intravenous use and their reactivity with staphylococcus protein A. Vox Sang 1980; 38:147-155. Romer J, Spath PJ, Skvaril F, Nydegger UE. Characterization of various immunoglobulin preparations for intravenous application. II. Complement activation and binding for staphylococcus protein A. Vox Sang 1982;42:74-80. Steele RW, Augustine RA, Tannenbaum AS, Charlton RK. A comparison of native and modified intravenous immunoglobulin for the management of hypogammaglobulinemia. Am J Med Sci 1987;293:69-74. Outbreak of hepatitis C associated with intravenous immunoglobulin administration: United States, October 1993-June 1994. MMWR 1994;43:505-509. Ballow M. Intravenous immunoglobulins: clinical experience and viral safety. J Am Pharm Assoc 2002;42:449-458. Renal insufficiency and failure associated with immune globulin intravenous therapy. MMWR 1999;48:1985-1998. Orbach H, Tishler M, Shoenfeld Y. Intravenous immunoglobulin and the kidney-a two-edged sword. Semin Arthritis Rheum 2004;34:593-601. Eijkhout HW, van den Broek PJ, van der Meer JW. Substitution therapy in immunodeficient patients with anti-IgA antibodies or severe adverse reactions to previous immunoglobulin therapy. Neth J Med 2003;61:213-217. Salama A, Temmesfeld B, Hippenstiel S, Kalus U, Suttorp N, Kiesewetter H. A new strategy for the prevention of IgA anaphylactic transfusion reactions. Transfusion 2004;44:509-511. Savasman C.M. Sandler S.G., Serologic Aspects of Treating Immune Thrombocytopenic Purpura Using Intravenous Rh Immune Globulin. Immunohematology 2001;17:106-110. Gelfand EW, Landwehr LP, Esterl B, Mazer B. Intravenous immuneglobulin: an alternative therapy in steroid-dependent allergic diseases. Clin Exp Immunol 1996;104:61-66. Dalakas MC. Mechanism of action of intravenous immunoglobulin and therapeutic considerations in the treatment of autoimmune neurologic diseases. Neurology 1998;51:2-8. Van Schaik IN, Lundkvist I, Vermeulen M, Brand A. Polyvalent immunoglobulin for intravenous use interferes with cell proliferation in vitro. J Clin Immunol 1992;12:325. Modiano JF, Amran D, Lack G, Bradley K, Ball C, Domenico J, et al. Posttranscriptional regulation of T cell IL-2 production by human pooled immunoglobin. Clin Immunol Immunopathol 1997:83:77-85. Andersson U, Bjork L, Skansen SU, Andersson J. Pooled human IgG modulates cytokine production in lymphocytes and monocytes. Immunol Rev 1994:139:21-42. Vuist W, Van Schaik I, Van Lint M, Brand A. The growth arresting effect of human immunoglobulin for intravenous use 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 1477 is mediated by antibodies recognizing membrane glycolipids. J Clin Immunol 1997;17:301-310. Cukrowska B, Sinkora J, Mandel L, Splichal I, Bianchi AT, Kovaru F, et al. Thymic B cells of pig fetuses and germ-free pigs spontaneously produce IgM, IgG and IgA: detection by ELISPOT method. Immunology 1996;87:487-492. Cukrowska B, Sinkora J, Rehakova Z, Sinkora M, Splichal I, Tuckova L, et al. Isotype and antibody specificity of spontaneously formed immunoglobulins in pig fetuses and germ-free piglets: Production by CD B cells. Immunology 1996;88:611617. Ochsenbein AF, Fehr T, Lutz C, Suter M, Brombacher F, Hengartner H, et al. Control of early viral and bacterial distribution and disease by natural antibodies. Science 1999;286: 2156-2159. Fagarasan S, Honjo T. T-independent immune response: new aspects of B cell biology. Science 2000;290:89-91. Horwitz MS, Sarvetnick N. Viruses, host responses, and autoimmunity. Immunol Rev 1999;169:253-253. Terness P, Opelz G. Natural anti-immunoglobulin autoantibodies: Irrelevant by-products or immunoregulatory molecules? Int Arch Allergy Immunol 1998;115:270-277. Rossi F, Kazatchkine MD. Antiidiotypes against autoantibodies in pooled normal human polyspecific Ig. J Immunol 1989; 143:4104-4109. Marchalonis JJ, Kaymaz H, Dedeoglu F, Schluter SF, Yocum DE, Edmundson AB. Human autoantibodies reactive with synthetic autoantigens from T cell receptor beta-chain. PNAS 1992;89:3325-3329. Marchalonis JJ, Kaymaz H, Dedeoglu F, Schluter SF, Yocum DE, Edmundson AB. Immune modulatory effects of immunoglobulins on cell-mediated immune responses in vitro. Scand J Immunol 1993;38:477-484. Hurez V, Kaveri SV, Mouhoub A, Dietrich G, Mani JC, Klatzmann D, et al. Anti-CD4 activity of normal human immunoglobulin G for therapeutic use. (Intravenous immunoglobulin, IVIg). Ther Immunol 1994;1:269-277. Kaveri S, Vassilev T, Hurez V, Lengagne R, Lefranc C, Cot S, et al. Antibodies to a conserved region of HLA class I molecules, capable of modulating CD8 T cell-mediated function, are present in pooled normal immunoglobulin for therapeutic use. J Clin Invest 1996;97:865-869. Viard I, Wehrli P, Bullani R, Schneider P, Holler N, Salomon D, et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobulin. Science 1998;282:490-493. Trautmann A, Akdis M, Schmid-Grendelmeier P, et al. Targeting keratinocyte apoptosis in the treatment of atopic dermatitis and allergic contact dermatitis. J Allergy Clin Immunol 2001; 108:839-846. Prins C, Kerdel FA, Padilla RS, Hunziker T, Chimenti S, Viard I, et al. Treatment of toxic epidermal necrolysis with high-dose intravenous immunoglobulins: multicenter retrospective analysis of 48 consecutive cases. Arch Dermatol 2003;139:26-32. Prasad NK, Papoff G, Zeuner A, Bonnin E, Kazatchkine MD, Ruberti G et al. Therapeutic preparations of normal polyspecific IgG (IVIg) induce apoptosis in human lymphocytes and monocytes: a novel mechanism of action of IVIg involving the Fas apoptotic pathway. J Immunol 1998;161:3781-3790. Simon HU, Yousefi S, Dommann-Scherrer CC, Zimmermann DR, Bauer S, Barandun J, et al. Expansion of cytokine-produc- 1478 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. Boros et al. ing CD4-CD8- T cells associated with abnormal Fas expression and hypereosinophilia. J Exp Med 1996;183:1071-1082. Daigle I, Yousefi S, Colonna M, Green DR, Simon HU. Death receptors bind SHP-1 and block cytokine-induced anti-apoptotic signaling in neutrophils. Nat Med 2002;8:61-67. Bendtzen K, Svenson M, Hansen M. Autoantibodies to cytokines in IVIg. J Rheumatol 1993;20:2176-2177. Abe Y, Horiuchi A, Miyake M, Kimura S. Anti-cytokine nature of natural human immunoglobulin: one possible mechanism of the clinical effect of intravenous immunoglobulin therapy. Immunol Rev 1994;139:5-19. Ross C, Svenson M, Hansen MB, Veijlsgaard GL, Bendtzen K. Specific autoantibodies directed against interferon- in pharmaceutically prepared human immunoglobulin preparations. J Interferon Res 1994;14:159-160. Van der Pol,W-L, van de Winkel JGJ. IgG receptor polymorphisms: risk factors for disease. Immunogenetics 1998;48:222232. Ravetch JV, Bolland S. IgG Fc receptors. Annu Rev Immunol 2001;19:275-290. Unkeless JC, Jin J. Inhibitory receptors, ITIM sequences and phosphatases. Curr Opin Immunol 1997;9:338-343. Takai T. Roles of Fc receptors in autoimmunity. Nat Rev Immunol 2002;2:580-592. Bussel JB. Modulation of Fc receptor clearance and antiplatelet antibodies as a consequence of intravenous immune globulin infusion in patients with immune thrombocytopenic purpura. J Allergy Clin Immunol 1989;84:566-577. Basta M, Fries LF, Frank MM. High-dose intravenous immunoglobulin inhibits in vitro uptake of C4 fragments onto sensitized erythrocytes. Blood 1991;77:376-380. Lutz HU, Stammler P, Jelezarova E, Nater M, Späth PJ. Lutz HU, et al. High doses of immunoglobulin G attenuate immune aggregate-mediated complement activation by enhancing physiologic cleavage of C3b in C3bn -IgG complexes. Blood 1996; 88:184-193. Kazatchkine MD, Dietrich G, Hurez V, Ronda N, Bellon B, Rossi F, et al. V Region-mediated selection of autoreactive repertoires by intravenous immunoglobulin (IVIg). Immunol Rev 1994;139:79-107. Dalakas MC, Quarles RH, Farrer RG, Dambrosia J, Soueidan S, Stein DP, et al. A controlled study of intravenous immunoglobulin in demyelinating neuropathy with IgM gammopathy. Ann Neurol 1996;40:792-795. Andersson UG, Bjork L, Skansen-Saphir U, Andersson JP. Down-regulation of cytokine production and IL-2 receptor expression by pooled human IgG. Immunology 1993;79:211216. Ruiz de Souza V, Carreno MP, Kaveri SV, Ledur A, Sadeghi H, Cavaillon JM, et al. Selective induction of interleukin-1 receptor antagonist and interleukin-8 in human monocytes by normal polyspecific IgG (intravenous immunoglobulin). Eur J Immunol 1995;25:1267-1273. Scheinecker C, Zwolfer B, Koller M, Manner G, Smolen JS. Alterations of dendritic cells in systemic lupus erythematosus: phenotypic and functional deficiencies. Arthritis Rheum 2001; 44:856-865. Bayry J, Lacroix-Desmazes S, Carbonneil C, Misra N, Donkova V, Pashov A et al. Inhibition of maturation and function of dendritic cells by intravenous immunoglobulin. Blood 2003;101:758-765. Bayry J, Lacroix-Desmazes S, Delignat S, Mouthon L, Weill B, 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. 71. 72. Kazatchkine MD, et al. Intravenous immunoglobulin abrogates dendritic cell differentiation induced by interferon-alpha present in serum from patients with systemic lupus erythematosus. Arthritis Rheum 2003;48:3497-3502. Pricop L, Redecha P, Teillaud JL, Frey J, Fridman WH, SautesFridman C, et al. Differential modulation of stimulatory and inhibitory Fcgamma receptors on human monocytes by Th1 and Th2 cytokines. J Immunol 2001;166:531-537. Sharief MK, Ingram DA, Swash M, Thompson EJ. I.v.immunoglobulin reduces circulating proinflammatory cytokines in Guillain-Barré syndrome. Neurology 1999;52:1833-1838. Samuelsson A, Towers TL, Ravetch JV. Anti-inflammatory activity of IVIg mediated through the inhibitory Fc receptor. Science 2001;291:484-486. Farber CM, Crusiaux A, Schandene L, van Vooren JP, Goldman M, Dupont E, et al. Tumor necrosis factor and intravenous gammaglobulins in common variable immunodeficiency. Clin Immunol Immunopathol 1994;72:233-236. Aukrust P, Froland SS, Liabakk NB, Muller F, Nordoy I, Haug C, et al. Release of cytokines, soluble cytokine receptors, and interleukin-1 receptor antagonist after intravenous immunoglobulin administration in vivo. Blood 1994;84:2136-2143. Wolf HH, Davies SV, Borte M, Caulier MT, Williams PE, Bernuth HV, et al. Efficacy, tolerability, safety and pharmacokinetics of a nanofiltered intravenous immunoglobulin: studies in patients with immune thrombocytopenic purpura and primary immunodeficiencies. Vox Sang 2003;84:45-53. Roux KH, Tankersley DL. A view of the human idiotypic repertoire: electron microscopic and immunologic analyses of spontaneous idiotype-anti-idiotype dimers in pooled human IgG. J Immunol 1990;144:1387-1395. Tankersley DL. Dimer formation in immunoglobulin preparations and speculations on the mechanism of action of intravenous immune globulin in autoimmune diseases. Immunol Rev 1994;139:159-172. Teeling JL, Jansen-Hendriks T, Kuijpers TW, de Haas M, van de Winkel JG, Hack CE, et al. Therapeutic efficacy of intravenous immunoglobulin preparations depends on the immunoglobulin G dimers: studies in experimental immune thrombocytopenia. Blood 2001;98:1095-1099. Yu Z, Lennon VA. Mechanism of intravenous immune globulin therapy in antibody-mediated autoimmune diseases. N Engl J Med 1999;340:227-228. Hansen RJ, Balthasar JP. Intravenous immunoglobulin mediates an increase in anti-platelet antibody clearance via the FcRn receptor. Thromb Haemost 2002;88:898-899. Levy Y, Sherer Y, George J, Rovensky J, Lukac J, Rauova L, et al. Intravenous immunoglobulin treatment of lupus nephritis. Semin Arthritis Rheum 2000;29:321-327. Luke PP, Scantlebury VP, Jordan ML, Vivas CA, Hakala TR, Jain A, et al. Reversal of steroid- and anti-lymphocyte antibodyresistant rejection using intravenous immunoglobulin (IVIg) in renal transplant recipients. Transplantation 2001;72:419422. Shoenfeld Y, Rauova L, Gilburd B, Kvapil F, Goldberg I, Kopolovic J, et al. Efficacy of IVIg affinity-purified anti-doublestranded DNA anti-idiotypic antibodies in the treatment of an experimental murine model of systemic lupus erythematosus. Int Immunol 2002;14:1303-1311. Amemiya K, Semino-Mora C, Granger RP, Dalakas MC. Downregulation of TGF-beta1 mRNA and protein in the muscles of patients with inflammatory myopathies after treatment IVIg Treatment 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. with high-dose intravenous immunoglobulin. Clin Immunol 2000;94:99-104. Modiano JF, Amran D, Lack G, Bradley K, Ball C, Domenico J, et al. Posttranscriptional regulation of T-cell IL-2 production by human pooled immunoglobin.Clin Immunol Immunopathol 1997;83:77-85. Glotz D, Antoine C, Julia P, Suberbielle-Boissel C, Boudjeltia S, Fraoui R, et al. Desensitization and subsequent kidney transplantation of patients using intravenous immunoglobulins (IVIg). Am J Transplant 2002;2:758-760. Jordan S, Cunningham-Rundles C, McEwan R. Utility of intravenous immune globulin in kidney transplantation: efficacy, safety, and cost implications. Am J Transplant 2003;3: 653-664. John R, Lietz K, Burke E, Ankersmit J, Mancini D, Suciu-Foca N, et al. Intravenous immunoglobulin reduces anti-HLA alloreactivity and shortens waiting time to cardiac transplantation in highly sensitized left ventricular assist device recipients. Circulation 1999;100:II229-235. Akalin E, Ames S, Sehgal V, Fotino M, Daly L, Murphy B, et al. Intravenous immunoglobulin and thymoglobulin facilitate kidney transplantation in complement-dependent cytotoxicity B-cell and flow cytometry T- or B-cell crossmatch-positive patients. Transplantation 2003;76:1444-1447. Reed E, Hardy M, Benvenisty A, Lattes C, Brensilver J, McCabe R, et al. Effect of antiidiotypic antibodies to HLA on graft survival in renal-allograft recipients. N Engl J Med 1987; 316:1450-1455. Tyan DB, Li VA, Czer L, Trento A, Jordan SC. Intravenous immunoglobulin suppression of HLA alloantibody in highly sensitized transplant candidates and transplantation with a histoincompatible organ. Transplantation 1994;57:553-562. Lam L, Whitsett CF, McNicholl JM, Hodge TW, Hooper J. Immunologically active proteins in intravenous immunoglobulin. Lancet 1993;342:678. Toyoda M, Petrosyan A, Pao A, Jordan SC. Immunomodulatory effects of combination of pooled human gammaglobulin and rapamycin on cell proliferation and apoptosis in the mixed lymphocyte reaction. Transplantation 2004;78:1134-1138. Jordan SC, Tyan D, Stablein D, McIntosh M, Rose S, Vo A, et al. Evaluation of intravenous immunoglobulin as an agent to lower allosensitization and improve transplantation in highly sensitized adult patients with end-stage renal disease: report of the NIH IG02 trial. J Am Soc Nephrol 2004;15:3256-3262. Wu T, Abu-Elmagd K, Bond G, Demetris AJ. A clinicopathologic study of isolated intestinal allografts with preformed IgG lymphocytotoxic antibodies. Hum Pathol 2004;35:13321339. Blondeau B, Sauter B, Akalin E, Hoppenhauer L, RodriguesLais D, et al. Pre-stransplant immunomodulation of highly sensitized small bowel transplant candidates with IVIg. Am Transplant Congress 2005, Abstract 289. Bunchman TE, Parekh RS, Kershaw DB, Smoyer WE, Flynn JT, Valentini RP, et al. Beneficial effect of Sandoglobulin upon allograft survival in the pediatric renal transplant recipient. Clin Transplant 1997;11:604-607. Peraldi MN, Akposso K, Haymann JP, Flahaut A, Marlin C, Rondeau E, et al. Long-term benefit of intravenous immunoglobulins in cadaveric kidney retransplantation. Transplantation 1996;62:1670-1673. Pisani BA, Mullen GM, Malinowska K, Lawless CE, Mendez J, Silver MA, et al. Plasmapheresis with intravenous immuno- 88. 89. 90. 91. 92. 93. 94. 95. 96. 97. 98. 99. 100. 101. 1479 globulin G is effective in patients with elevated panel reactive antibody prior to cardiac transplantation. J Heart Lung Transplant 1999;18;701-706. Casadei DH, del C Rial M, Opelz G, Golberg JC, Argento JA, Greco G, et al. A randomized and prospective study comparing treatment with high-dose intravenous immunoglobulin with monoclonal antibodies for rescue of kidney grafts with steroidresistant rejection. Transplantation 2001;71:53-58. Schussler O, Genevaz D, Latremouille C, Goussev N, Kaveri S, Glotz D. Intravenous immunoglobulins for therapeutic use contain anti-idiotypes against xenophile antibodies and prolong discordant graft survival. Clin Immunol Immunopathol 1998;86:183-191. Schussler O, Lantoine F, Devynck MA, Glotz D, David-Dufilho M. Human immunoglobulins inhibit thrombin-induced Ca2⫹ movements and nitric oxide production in endothelial cells. J Biol Chem 1996;271:264-273. Tyden G, Kumlien G, Genberg H, Sandberg J, Lundgren T, Fehrman I. ABO incompatible kidney transplantations without splenectomy, using antigen-specific immunoadsorption and rituximab. Am J Transplant. 2005;5:145-148. Nydegger U, Mohacsi P, Koestner S, Kappeler A, Schaffner T, Carrel T. ABO histo-blood group system-incompatible allografting. Int Immunopharmacol. 2005;5:147-153. Morioka D, Sekido H, Kubota K, Sugita M, Tanaka K, Togo S, et al. Antibody-mediated rejection after adult ABO-incompatible liver transplantation remedied by gamma-globulin bolus infusion combined with plasmapheresis. Transplantation 2004;27:1225-1228. Terrault NA, Wright TL. Hepatitis B virus infection and liver transplantation. Gut 1997;40:568-571. Yoshida EM, Erb SR, Partovi N, Scudamore CH, Chung SW, Frighetto L, et al. Liver transplantation for chronic hepatitis B infection with the use of combination lamivudine and low-dose hepatitis B immune globulin. Liver Transpl Surg 1999;5:520525. Angus PW, McCaughan GW, Gane EJ, Crawford DH, Harley H. Combination low-dose hepatitis B immune globulin and lamivudine therapy provides effective prophylaxis against posttransplantation hepatitis B. Liver Transpl 2000;6:429-433. Di Paolo D, Tisone G, Piccolo P, Lenci I, Zazza S, Angelico M. Low-dose hepatitis B immunoglobulin given “on demand” in combination with lamivudine: a highly cost-effective approach to prevent recurrent hepatitis B virus infection in the long-term follow-up after liver transplantation. Transplantation 2004;77: 1203-1208. Turgeon N, Fishman JA, Doran M, Basgoz N, Tolkoff-Rubin NE, Cosimi AB, et al. Prevention of recurrent cytomegalovirus disease in renal and liver transplant recipients: effect of oral ganciclovir. Transpl Infect Dis 2000;2:2-10. Arbo MD, Snydman DR, Wong JB, Goldberg HS, Schmid CH, Pauker SG. Cytomegalovirus immune globulin after liver transplantation: a cost-effectiveness analysis. Clin Transplant 2000;14:19-27. King SM, Superina R, Andrews W, Winston DJ, Dunn S, Busuttil RW, et al. Randomized comparison of ganciclovir plus intravenous immune globulin (IVIG) with IVIG alone for prevention of primary cytomegalovirus disease in children receiving liver transplants. Clin Infect Dis 1997;25:1173-1179. Gane E, Saliba F, Valdecasas GJ, O’Grady J, Pescovitz MD, Lyman S, et al. Randomised trial of efficacy and safety of oral 1480 102. 103. 104. 105. Boros et al. ganciclovir in the prevention of cytomegalovirus disease in liver-transplant recipients. Lancet 1997;350:1729-1733. Singh N, Paterson DL, Gayowski T, Wagener MM, Marino IR. Cytomegalovirus antigenemia directed pre-emptive prophylaxis with oral versus I.V. ganciclovir for the prevention of cytomegalovirus disease in liver transplant recipients: a randomized, controlled trial. Transplantation 2000;70:717-722. Singh N, Wannstedt C, Keyes L, Gayowski T, Wagener MM, Cacciarelli T. Efficacy of valganciclovir administered as preemptive therapy for cytomegalovirus disease in liver transplant recipients: impact on viral load and late-onset cytomegalovirus disease. Transplantation 2005;79:85-90. Takatsuki M, Uemoto S, Kurokawa T, Koshiba T, Inomata Y, Tanaka K. Idiopathic thrombocytopenic purpura after a livingrelated liver transplantation. Transplantation 1999;67:479481. Rosoff PM, Tuttle-Newhall E, Treem WR. Successful treatment of immune thrombocytopenic purpura with anti-D antibody following a cadaveric liver transplant for hepatoblastoma. Med Pediatr Oncol 2003;40:402-404. 106. Echaniz-Laguna A, Battaglia F, Ellero B, Mohr M, Jaeck D. Chronic inflammatory demyelinating polyradiculoneuropathy in patients with liver transplantation. Muscle Nerve 2004;30: 501-514. 107. Ganschow R, Englert C, Grabhorn E, Richter A, Hinrichs B, Broering DC, et al. Hypogammaglobulinemia in pediatric liver transplant recipients. Pediatr Transplant 2005;9:215-219. 108. Yamani MH, Avery RK, Mawhorter SD, Young JB, Ratliff NB, Hobbs RE, et al. Hypogammaglobulinemia following cardiac transplantation: a link between rejection and infection. J Heart Lung Transplant 2001;20:425-430. 109. Corales R, Chua J, Mawhorter S, Young JB, Starling R, Tomford JW, et al. Significant post-transplant hypogammaglobulinemia in six heart transplant recipients: an emerging clinical phenomenon? Transpl Infect Dis 2000;2:133-139. 110. Yamani MH, Avery R, Mawhorter S, Young JB, McNeill A, Cook DJ, et al. Hypogammaglobulinemia after heart transplantation: impact of pre-emptive use of immunoglobulin replacement (CytoGam) on infection and rejection outcomes. Transpl Infect Dis 2001;3:40-43.














![2014 Jun 13. pii: ciu449. [Epub ahead of print] Clinical efficacy](http://s1.studyres.com/store/data/004659563_1-cbbffe8299af8775d28fa21caafaf24f-150x150.png)