* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cell Pathology Lecture 4
Survey
Document related concepts
Transcript
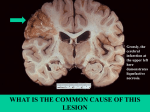
Cellular Pathology (VPM 152) Lecture 4 (web) Paul Hanna Jan 2016 IRREVERSIBLE CELL INJURY 1) Necrosis • describes the range of morphologic changes that follow cell death in living tissue • the morphologic appearance is due to 2 concurrent processes: denaturation of proteins (nonproteolytic alteration 2o or 3o structure) Raw egg white (albumin protein) is a transparent (clear) viscous liquid Adding heat, acid or alkali will denature (misfold) the proteins which results in a change of the color to white (opaque) & the texture becomes solid. enzymatic digestion autolysis* (self digestion) = endogenous enzymes derived from the lysosomes of the dead cells themselves. heterolysis = lysosomes of immigrant leukocytes. *autolysis also used for changes that occur in all cells after death, ie postmortem autolysis 1) Necrosis • distinctive morphologic patterns depending on whether enzyme catabolism or protein denaturation predominates • morphologic patterns of necrosis include: Coagulation Necrosis Liquefactive Necrosis Caseous Necrosis *Gangrenous Necrosis *Fat Necrosis a) Coagulation Necrosis • most common manifestation of cell death • characteristic of hypoxic / ischemic death of cells in all tissues (except brain) • on LM, basic outline of the coagulated cell persists at least a few days (protein denaturation predominates over enzymatic digestion) • necrotic cells eventually removed by leukocyte proteolysis & phagocytosis a) Coagulation Necrosis Gross Appearance • architecture resembles normal tissue, but color and texture are different • lighter in color – denatured cytoplasmic proteins & decreased blood flow • usually firm • tissue may be swollen or shrunken • may see a local vascular / inflammatory reaction to necrotic tissue Figure 01-18A (McGavin & Zachary). Coagulation necrosis, infarcts, kidney, cow. A, Note the pale regions of acute coagulation necrosis surrounded by a red rim of active hyperemia and inflammation (far left). Bovine, kidney, renal infarct, cut surface. Note pyramidal (wedge) shaped area of necrosis with hyperemic border. Bovine, fetus, liver, IBR (infectious bovine rhinotracheitis) - multifocal hepatic necrosis (necrotizing hepatitis) Bovine, liver: Multifocal hepatic necrosis (coagulative) due to infection with the bacterium Fusobacterium necrophorum. The majority of bacterial infections cause liquefactive necrosis due to the marked infiltration of neutrophils with associated heterolysis; however in this particular bacterial infection there are toxins which result in coagulative necrosis (at least initially). Bovine, heart, myocardial necrosis (coagulative); note irregular area of pallor within myocardium. a) Coagulation Necrosis Microscopic Appearance • original cell shape & tissue architecture is preserved (ie eosinophilic "shadow“) • cytoplasm: increased eosinophilia (H&E stain) usually hyalinized (homogeneous / glassy) may be mineralized • nucleus: karyolysis pyknosis karyorrhexis Figure 01-17B (McGavin & Zachary). Pyknosis and karyolysis, renal cortex, chloroform toxicosis, mouse. Some epithelial cells exhibit hydropic degeneration, whereas others are necrotic. Some necrotic cells exhibit pyknosis (arrow), whereas others have lost the nucleus or have a very pale nucleus (karyolysis) (arrowheads) Figure 01-17C (McGavin & Zachary) Karyorrhexis, lymphocytes, spleen, dog. Spleen of a dog with parvovirus infection. Lymphocyte nuclei have fragmented because of the infection (arrow). H&E stain. Skeletal muscle, white muscle disease; note coagulation necrosis of myofibers characterized by fragmentation and hyalinization; also note extensive mineralization (blue-purple staining) b) Liquefactive Necrosis • when enzymatic digestion of necrotic cells predominates • many bacterial infections; neutrophils contain potent hydrolases • in hypoxic damage of the CNS Gross appearance • affected tissue is liquefied, ie soft to viscous to fluid mass • in inflammation, the liquid is often mostly dead WBC’s (pus) Microscopic appearance • may see degenerate neutrophils and/or amorphous necrotic material Porcine, abscess in ventral neck / shoulder area; note escape of purulent exudate (pus) when the abscess is lanced. (ie purulent exudate is an example of liquefactive necrosis). Porcine, kidney, pyelonephritis, note purulent exudate (again an example of liquefactive necrosis). Ovine, pituitary gland abscess, irregular shaped aggregates of amorphous acidophilic material (liquefied cells) with basophilic granular material (degenerate neutrophils) at margins Figure 01-20A (McGavin & Zachary). Liquefactive necrosis. Acute polioencephalomalacia, brain, goat. A thiamine deficiency has resulted in polioencephalomalacia (ie polio = grey, encephalo = brain and malacia = necrosis). This is liquefaction necrosis with varying degrees of tissue separation (arrows). Scale bar = 2 cm. Note: can see this same lesion resulting from either ischemia, lead poisoning or “salt” poisoning. Also note: c) Caseous Necrosis • typical seen with specific bacterial diseases, eg TB, caseous lymphadenitis • infections in birds, since heterophils lack myeloperoxidase Gross appearance • grey-white, dry, friable to pasty (caseous = cheese like) Microscopic appearance • dead cells persist as amorphous, coarsely granular, eosinophilic debris • retain cellular outline (coagulative) caseous complete dissolution (liquefactive) Ovine, submandibular lymph node, with a disease called “caseous lymphadenitis” caused by infection with the bacteria Corynebacterium pseudotuberculosis; note the type of necrosis in this exudate is caseous (not quite liquefactive, but more broken down than coagulation necrosis, ie it would be a thick pasty texture, if you could cut / feel it) Equine, lung tissue, pyogranulomatous pneumonia due to Rhodococcus equi; note caseous exudate (arrows). Figure 01-19. Tuberculosis, lymph node, transverse section, ox. A, The lymph has been replaced by a caseating granuloma. Note the caseous necrosis characterized by a pale yellow, crumbly exudate. B, Granulomatous inflammation in caseous necrosis. Cell walls are disrupted and tissue architecture is lost. Mineralization (not seen here) is common in this type of necrosis. H&E stain. d) Gangrenous Necrosis • definition = necrosis (usually ischemic) of extremities, eg digits, ear tips • dry gangrene = coagulation necrosis of an extremity • wet gangrene = when the coagulative necrosis of dry gangrene is modified by liquefactive action of saprophytic / putrefactive bacteria Cat, note, sloughing of ear tips and paws following dry gangrene due to frostbite. Bovine, calf, gangrenous necrosis / dry gangrene with sloughing of distal limbs, ergot poisoning Calf, gangrenous necrosis of distal limbs due to ischemia; this ischemia could result from frostbite or sepsis or a mycotoxin such as ergot. Fig 1-21A (McGavin & Zachary), Moist gangrene, udder, sheep. The surrounding tissue is well vascularized, which contributes to the wet and bloody nature of the lesion. Often saprophytic bacteria and clostridia contaminate areas of necrosis. Bovine, mammary gland, wet gangrene; tissue starting to slough. Bovine, lung, “gangrenous” pneumonia following aspiration of rumen content. [Although historically called “gangrenous” pneumonia, it is probably better called necrotizing pneumonia as a morphologic Dx or aspiration pneumonia as an etiologic Dx] e) Fat Necrosis • distinguished by its location within body fat stores • etiology: inflammation (eg pancreatitis), Vit E deficiency, trauma, idiopathic Canine, pancreatitis (“recurrent pancreatic necrosis”) with mesenteric fat necrosis Canine, pancreatitis (“recurrent pancreatic necrosis”) with omental fat necrosis. Canine, pancreatitis (“recurrent pancreatic necrosis”) with fat necrosis; note necrosis of fat (larger arrow) and pancreatic tissues (smaller arrow)– some areas of coagulative type and other areas with significant enzyme degradation (liquefaction) of necrotic tissue. 2) Apoptosis • Greek = “falling off” • death of single cells through activation of genetically programmed “suicide” pathways • apoptosis indicates selective elimination of cells (either physiologic or pathologic), while necrosis points to widespread tissue injury (severe pathologic stimuli) • apoptosis → death of single cells / intact membranes / phagocytosed with no inflam. necrosis → area of dead cells / damaged membranes / enzyme digest. & 2o inflam. Figure 17-35 (Molecular Biolology of the Cell, 4th ed) Sculpting the digits in the developing mouse paw by apoptosis (A) The paw in this mouse embryo has been stained with a dye that specifically labels cells that have undergone apoptosis. The apoptotic cells appear as bright green dots between the developing digits (arrows). (B) This interdigital cell death eliminates the tissue between the developing digits, as seen one day later, when few, if any, apoptotic cells can be seen. Incomplete tissue sculpting (ie incomplete apoptosis) of the digits results in syndactyly (from Greek syn = "together" + dactyly = “digits”) It can be partial, as in the web toes (above left) or complete as seen in the childs hand (above right) and calves hooves (below left) 2) Apoptosis • seen in many physiologic, adaptive and pathologic events: Physiologic causes: Cells undergoing programmed cell death during embryogenesis Cells undergoing normal turnover - hormone-dependent involution - cell deletion in proliferating population Immune System - deletion of autoreactive T cell in thymus - immune regulation 2) Apoptosis Pathologic causes: DNA damaged beyond repair – eg radiation, toxins Misfolded proteins – ER stress Specific infectious agents – esp viruses Specific immune responses – via cytotoxic T cells Pathologic atrophy of organs after duct obstruction c) Biochemical Mechanisms Signaling pathways that initiate apoptosis (“Death Signals”) • stimulate targets on cell surface or within the cell c) Biochemical Mechanisms Control and integration • balance of +ve / -ve regulatory molecules determines outcome of the affected cell c) Biochemical Mechanisms Common execution phase • actual death program accomplished by endonucleases & proteases (esp caspases) c) Biochemical Mechanisms Removal of dead cells • apoptotic bodies have ligands for phagocytic cells (efficient / no inflammation) 2) Apoptosis d) Morphology • considerable apoptosis may occur in tissues before it is evident on histology Cell shrinkage - cytoplasm has packed organelles Chromatin condensation - dense aggregates of chromatin ± fragmentation Formation of cytoplasmic blebs / apoptotic bodies - with intact membranes (± nuclear fragments) Phagocytosis of apoptotic cells / bodies - usually by macrophages with no inflammation Figure 1-8 (Robbins) Schematic illustration of morphologic changes in cell injury culminating in necrosis or apoptosis. Note: with necrosis cells swell, lose membrane integrity and incite an inflammatory response VS apoptosis where cells shrink (condense), membranes remain intact in forming apoptotic bodies and are removed with minimal inflammation. SEM showing showing cytoplasmic blebbing / apoptotic body formation. Figure 3–23 (Junqueira’s Basic Histology) Late apoptosis-formation of apoptotic bodies. TEM of a cell in late apoptosis shows that during this process the cell’s shape changes radically and large cytoplasmic vesicles (blebs) are formed. These detach from the cell and often separate one from another, but remain contained within plasma membrane so that no cytoplasmic contents are released into the extracellular space. Figure 01-33 (McGavin & Zachary). Apoptosis, cytoarchitecture of cells, pancreas, rat. Individual acinar cells are shrunken and their chromatin condensed and fragmented (arrows). Cytoplasmic blebs are found in adjacent cells. Inflammation is absent. H&E. (note: blockage of glandular ducts typically results in apoptosis within the gland) www.skin-science.com Note, arrows indicate apoptotic epidermal keratinocytes (“sunburn cells”) due to UVB radiation. These can be induced within 30 minutes of sun exposure. e) Consequences of “too much” or “too little” apoptosis Disorders associated with defective apoptosis (increased cell survival) • increased survival of abnormal cells with neoplasia • increased survival of autoreactive lymphocytes causing autoimmune disorder Disorders associated with increased apoptosis (excessive cell death) • increased loss of cells in: neurodegenerative diseases ischemic injured cells viral infected cells