* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cellulitis protocol
Neglected tropical diseases wikipedia , lookup
Antibiotics wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Gastroenteritis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
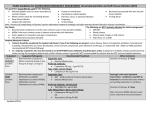
Trichinosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Schistosomiasis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Anaerobic infection wikipedia , lookup
Candidiasis wikipedia , lookup
Cellulitis Cellulitis – Cellulitis is an infection of the skin with some extension into the subcutaneous tissues.13 While a lower extremity is the most common location.14 Cellulitis can involve any area of the body. Erysipelas represents a distinct form of superficial cellulitis that is associated with marked swelling of the skin and does not involve subcutaneous tissues. The margins of involved and normal tissues are sharply demarcated, particularly at bony prominences, in contrast to cellulitis in which the margins are generally not distinct. Cellulitis falls into a continuum of skin infections including impetigo, folliculitis, carbuncles, and abscesses. Necrotizing cellulitis is more akin to other necrotizing infections. With the diminished infectious organism recognition and organism attacking subsets of the immune system, entrance of an organism into the skin begins an invasion that trespasses from the dermal layers into the subcutaneous tissues. The organism populates the area and begins to reach out into the surrounding tissues through both tissue and hematological routes of extension. Cellulitis.doc Page 1 of 13 Created on 7/11/2012 1:20:00 PM Cellulitis SCOPE OF PRACTICE PRACTITIONER SCOPE OUTOMES • Nurse Practitioner – Aged Care Medical Practitioner ± Nurse Practitioner Cellulitis.doc The NP will refer all Hall & Prior residents outside their scope of practice, to a medical practitioner. Page 2 of 13 The expected outcome of use of this clinical guideline is rapid and effective relief from symptoms and eradication of bacteria, from wounds skin infections and prevention of reoccurrence, reduction in hospitalisation rates, improved morbidity and reduce the risk and rate of mortality. • Upon failure of treatment, complications of infection or recurrence of infection, referral to an urologist is required. Referral to occupational therapist and/or physiotherapist should be considered if lack of mobility or function are contributing factors. Created on 7/11/2012 1:20:00 PM Cellulitis RESIDENT’S ASSESSMENT RESIDENT’S HISTORY SCOPE OUTCOMES Presenting symptoms Signs and symptoms of cellulitis in the elderly: Cellulitis is a recognizable clinical syndrome with both systemic and local features. Systemic findings, Increased age increases skin frailty and increases the risk of infection. Pressure ulcers increase the risk of mortality /morbidity. Some become infected, cellulitis causes inflammation tender, painful, erythematous and oedematous presentations. Usually caused by Staph.aureus/streptococcus pyogenes. Severe myalgias and fatigue can occasionally mimic influenza, particularly if there is a delay in onset or in the recognition of local findings. Disorientation or mental status changes can occur in the absence of shock, particularly in the elderly. Cellulitis.doc Page 3 of 13 • Gaining comprehensive and holistic data in order to prescribe appropriate diagnostics and interventions related to indicators identified in assessment. • Constructing and ruling out related differential diagnoses to specific pathophysiology identified. • Prevent interactions and further complications with interventions • If known allergy to recommended formulary, NP & MP to instigate alternative treatment option to ensure optimal and safe response to treatment. Created on 7/11/2012 1:20:00 PM Cellulitis RESIDENT’S HISTORY INFORMATION OUTCOMES A number of findings are typical of cellulitis: Macular erythema that is largely confluent generalized swelling of the involved area, warmth to the touch of the involved skin, tenderness in the affected area,tender regional lymphadenopathy is common lymphangitis may be present. Abscess formation also may be present, significance of accompanying tinea pedis or other dermatologic abnormalities such as psoriasis or dyshidrosis in resident’s with lower extremity involvement. The absence of erythema, warmth, swelling, and local tenderness argue strongly against the diagnosis of cellulitis; lymphangitis is supportive of the diagnosis of cellulitis, if present, but its absence does not establish the diagnosis. The pattern of skin involvement can vary, but the sharply demarcated margins seen in erysipelas are uncommon in other forms of cellulitis. Discrete lesions may or may not be present; bullous cellulitis is occasionally seen, usually due to group A streptococcus. Cellulitis.doc Page 4 of 13 Created on 7/11/2012 1:20:00 PM Cellulitis RESIDENT’S HISTORY INFORMATION OUTCOMES Known risk factors for the presenting symptoms Risk factors fall into several categories: disruption of the cutaneous barrier (eg, leg ulcer, traumatic wound, dermatoses) venous or lymphatic compromise (eg, venous insufficiency, overweight. Previous history of cellulitis. Staphylococcus aureus & beta-hemolytic streptococci in the toe webs are significantly associated with acute cellulitis of the lower limb. Relevant medical, surgical and obstetric history Prompt diagnosis and treatment will be initiated Previous medical history Medications Current Medications Other relevant information Allergies, previous cellulitis history, nutrition & hydration, skin integrity, mobility, cognition, behaviour PHYSICAL Ax SCOPE Usual physical examination Record findings: vital signs, skin assessment, wound assessment, pain assessment Assess systems that may reveal fever with/without tachycardia, lymphadenopathy, vascular streaking, mental status changes, hypotension, decreased pulses & signs of DVT. Specific focus on lifestyle risks, previous surgery, comorbid conditions: diabetes, PVD, peripheral arterial disease, heart failure, use of immunosuppressive agents & potential sources of skin disruption: ulcerations, fungal infection in the toe webs, punctures & animal bites. Indications for specific examinations Cellulitis.doc OUTCOMES Page 5 of 13 • Correct diagnosis, provision of effective disease and symptomatic eradication/relief Created on 7/11/2012 1:20:00 PM Cellulitis INVESTIGATIONS INDICATIONS INVESTIGATIONS Routine investigations Laboratory/diagnostics used for diagnosis and identification of organism: skin swab only if ulceration or exudate present. Pathology To determine underlying organism, severity and sensitivity of organism. Wound/skin MCS OUTCOMES • Results from all investigations will be used when determining future management of the resident’s cellulitis and appropriate treatment. • Accurate diagnosis will be made. • Correct pharmacotherapy will be prescribed based on sensitivity of organism. • Appropriate dressings will be initiated Imaging nil Haematology / Biochemistry If suspected pyelonephritis only. FBC, U&E Other Investigations nil Cellulitis.doc Page 6 of 13 Created on 7/11/2012 1:20:00 PM Cellulitis FOLLOW UP AND EDUCATION INTERVENTION INFORMATION Pharmacotherapeutics The treatment chosen will be dependent on the organism believed to have caused the infection, with consideration of the residents allergy history, general medical condition, and renal and hepatic status, as well as the degree and quality of infection, all may effect outcomes of resident’s hospitalization versus resident’s treatment. In the feet, topical antifungals should be used in those with fissures,until healed. Analgesics should be used as appropriate. Immobilization of the area with elevation (if in a limb) is important to decrease pain and diminish oedema. Blood glucose levels in known diabetics should be regularly monitored and managed. Consultation with a GP is recommended if necrotizing fascitis or an abscess is suspected, if cellulitis occurs in the orbit of the eye, if there is high fever or extreme pain, if the condition does not respond to treatment, or if surgical debridement is required. Hospitalization may be required in any of these instances. Non-pharmacological Cellulitis.doc Page 7 of 13 OUTCOMES • • • • Eradication of infection Prevention of recurrence of infection Symptomatic relief Management of oedema. Created on 7/11/2012 1:20:00 PM Cellulitis FOLLOW UP AND EDUCATION INTERVENTION INFORMATION Follow up appointments Resident needs to be reviewed daily post commencing antibiotic therapy to reassess symptoms & monitor for any complications or adverse reactions to therapy.1,3 Follow up consultation is required to validate eradication of inf. & determine whether further antimicrobial treatment is required. An evidence based care plan should be developed.1,3 NPs are required to follow up on all referrals to allied health/specialists & reinforce education & management strategies. Resident & their caregivers need to understand the importance of completion of diagnostic & treatment plans. Completion of antibiotic regimens is important to eradicate the infecting organisms & to decrease the possibility of treatment failures, including organisms’ tolerance to antibiotics. Education re: possible medication side effects & anaphylaxis; signs & symptoms of superinfection of the site, DVT, systemic infection; & the importance of follow-up care is needed. Control of oedema, elevation of the affected limb, & minimization of trauma to the area should be taught. The resident’s or caregiver should be able to demonstrate specific wound care. Signs & symptoms that require immediate follow-up should be emphasized. Letter to residents GP Resident’s/staff education Letters Cellulitis.doc Page 8 of 13 OUTCOMES • • • • • • • Underlying disease will be detected at follow up. Upon failure of treatment, complications of infection or recurrence of infection, referral to a medical practitioner is required.1 Referral to occupational therapist and/or physiotherapist should be considered if lack of mobility is a contributing factor. Optimise independence, awareness and education Optimise compliance with treatment Optimise eradication of infection and prevent recurrence of infection Review of resident notes Letters/progress reports are provided at the discretion of the NP Created on 7/11/2012 1:20:00 PM Cellulitis – PHARMACOTHERAPY The management of cellulitis can be divided into two distinct phases: Treatment directed at the acute cellulitis, including the decision about hospitalization Preventive therapy to diminish the likelihood of subsequent bouts of cellulitis, particularly in resident’s who have had previous episodes in the same anatomic location. Decision to hospitalize - Most resident’s with cellulitis present with recognizable skin findings (erythema, skin induration, edema, lymphangitis) and low-grade fever. For the occasional resident’s with high fevers, rigors and other signs of systemic toxicity including mental status changes or even shock, the decision to admit the resident’s to the hospital is obvious. 1st line treatment for cellulitis flucloxacillin/cephalexin Diabetics – Cellulitis in the diabetic resident with a nonhealing plantar foot ulcer usually requires broader spectrum coverage to include treatment of S. aureus, beta-hemolytic streptococci, aerobic gram-negative bacilli, and anaerobes pending results of cultures and susceptibility testing : antibiotic therapy is a treatment option in these resident’s but should not be used first for cellulitis in the absence of an ulcer. One study of 90 diabetic resident’s with limb-threatening foot infections concluded that an antibiotic such as ampicillin-sulbactam was less costly and just as effective.19 Diagnostic testing for accompanying osteomyelitis or abscess formation should be included in the evaluation of diabetic resident’s with cellulitis of the foot. Treatment Augmentin duo 1 tab bd Cellulitis.doc Page 9 of 13 Created on 7/11/2012 1:20:00 PM Cellulitis PHARMACOTHERAPY FORMULARY cephalexin Drug (generic name): cephalexin 1st line Poisons schedule: schedule 4 Therapeutic class: 8(b) cephalosporins Dosage range: 250mg – 500mg Route: oral Frequency of administration: 6 hourly Duration of order: variable Actions: intervenes in bacteria cell wall peptidoglycan synthesis Indications for use: staphylococcal & streptococcal infections (when mild-moderate allergy to penicillins), susceptible gram negative bacterial UTIs, epididymo-orchitis Contraindications for use: allergy to penicillins, cephalosporins or carbapenems Adverse drug reactions: nausea, diarrhoea, electrolyte imbalance, rash, rare: cholestatic hepatitis Cellulitis.doc Page 10 of 13 Created on 7/11/2012 1:20:00 PM Cellulitis PHARMACOTHERAPY flucloxacillin 1st line amoxycillin with clavulanic acid (diabetic) Drug (generic name): amoxycillin with clavulanic acid Poisons schedule: schedule 4 Drug (generic name): flucloxacillin Therapeutic class: 8(a) penicillins – infections & infestations Poisons schedule: schedule 4 Dosage range: 875mg/125mg Therapeutic class: 8(a) penicillins – infections & infestations Route: oral Dosage range: 250-500mg Frequency of administration: 12 hourly Route: oral Duration of order: 5-10days Frequency of administration: 6 hourly Actions: bactericidal, intervenes in bacteria cell wall Duration of order: variable peptidoglycan synthesis Actions: bactericidal, intervenes in bacteria cell wall Indications for use: hospital acquired pneumonia, UTI, peptidoglycan synthesis epididymo-orchitis, bites & clenched fist injuries, otitis media, Indications for use: staphylococcal skin infections incl:folliculitis, acute bacterial sinusitis, acute cholecystitis, melioidosis boils, carbuncles, bullous impetigo, mastitis, crush injuries, stab Contraindications for use: allergy to penicillins, cephalosporins wounds, infected scabies or carbapenems. Cholestatic jaundice or hepatic dysfunction Contraindications for use: allergy to penicillins, cephalosporins associated with amoxycillin with Clavulanic acid, or ticarcillin with or carbapenems. Cholestatic hepatic associated with dicloxicillin Clavulanic acid or flucloxicillin Adverse drug reactions: transient increases in liver enzymes & Adverse drug reactions: transient increase in liver enzymes & bilirubin, cholestatic hepatitis bilirubin, cholestatic hepatitis, rare: acute generalised exanthematous pustulosis Cellulitis.doc Page 11 of 13 Created on 7/11/2012 1:20:00 PM Cellulitis PHARMACOTHERAPY dicloxacillin Drug (generic name): dicloxacillin Poisons schedule: schedule 4 Therapeutic class: 8(a) penicillins – infections & infestations Dosage range: 250-500mg Route: oral Frequency of administration: 6 hourly Duration of order: variable Actions: bactericidal, intervenes in bacteria cell wall peptidoglycan synthesis Indications for use: staphylococcal skin infections incl: folliculitis, boils, carbuncles, bullous impetigo, mastitis, crush injuries, stab wounds, infected scabies, pneumonia, osteomyelitis, septic arthritis, septicaemia, empirical treatment for endocarditis, surgical prophylaxis Contraindications for use: allergy to penicillins, cephalosporins or carbapenems. Cholestatic hepatitis with dicloxacillin or flucloxacillin Adverse drug reactions: transient increase in liver enzymes & bilirubin Cellulitis.doc Page 12 of 13 Created on 7/11/2012 1:20:00 PM REFERENCES 1. Clinical Practice Guidelines for Nurses in Primary Care [monograph online]. 2000 [cited 2006 Apr 12]. Available from: http://www.hc-sc.gc.ca/msb/fnihp. 2. Tal S, Guller V, Levi S, Bardenstein R, Berger D, Gurevich I, Gurevich A. Profile and prognosis of febrile elderly resident’s with bacteremic urinary tract infection. Journal of Infection [serial online]. 2005 [cited 2006 Oct 20]; 50:296-305. Available from: ScienceDirect. 3. The Royal Australian College of General Practitioners. Medical Care of Older Persons in Residential Aged Care Facilities. 4th ed. South Melbourne: The Royal Australian College of General Practitioners; 2005. 4. Wagenlehner FM, Naber KG. Treatment of bacterial urinary tract infections: presence and future. European Urology [serial online]. 2006 [cited 2006 Oct 20]; 49:235-244. Available from: ScienceDirect. 5. Dartnell JG, editor. Therapeutic guidelines: antibiotic. 12th ed. Victoria: Therapeutic Guidelines Limited; 2003. 6. Rossi S, editor. Australian medicines handbook. Adelaide SA: Australian Medicines Handbook Pty Ltd; 2011. 7. eMIMS MIMS. MIMS medicine information [standard online]. c2005 [cited 2006 Oct 20]. Available from: eMIMS MIMS Online. 8. Hughes J. Urinary tract infections. Proceedings from The Infectious Diseases Module Lectures; 2006 Oct 9-16; Bentley, Perth: Curtin University of Technology; n.d. 9. McMurdo M, Bissett L, Price R, Phillips G, Crombie I. Does ingestion of cranberry juice reduce symptomatic urinary tract infections in older people in hospital? A double-blind, placebo-controlled trial. Age and Ageing. 2005; 34: 256-261. 10. etg complete( internet ). Melbourne : Therapeutic Guidelines Limited; 2011 Nov Accessed 2001at http://etg.com.au/ref/ref 11. Grayson ML, McDonald M, Gibson K, Athan E, Munckhof WJ, Paull P, et al. Once-daily intravenous cefazolin plus oral probenecid is equivalent to once-daily intravenous ceftriaxone plus oral placebo for the treatment of moderate-to-severe cellulitis in adults. Clinical Infectious Diseases. 2002; 34(11): 1440-1448. 12. Ginsberg MB. Cellulitis: analysis of 101 cases and review of the literature. Southern Medical Journal. 1981; 74(5): 530-533. 13. Fleisher G, Ludwig S. Cellulitis: a prospective study. Annals of Emergency Medicine. 1980; 9(5): 246-249. 14. Kennedy M L, Fletcher KR, Plank LM. Management guidelines for nurse practitioners working with older adults. 2nd ed. Philadelphia: F. A. Davis; 2004. 15. Reuben DB, Herr KA, Pacala JT. Geriatrics at your fingertips. 6th ed. Malden, MA: Blackwell; 2004. 16. McKinnon PS, Paladino JA, Grayson ML, Gibbons GW, Karchmer AW. Cost-effectiveness of ampicillin/su;bactam versus imipenum/cilastatin in the treatment of limb-threatening foot infections in diabetic resident’s. Clinical Infection Diseases. 1997; 24(1): 57-63. 17. Friedlaender MH. A review of the causes and treatment of bacterial and allergic conjunctivitis. Clinical Therapeutics. 1995; 17(5): 800-810. 18. Wan W L, Farkas GC, May WN, Robin JB. The clinical characteristics and course of adult gonococcal conjunctivitis. American Journal of Ophthalmology. 1986; 102(5): 575-583. Cellulitis.doc Page 13 of 13 Created on 7/11/2012 1:20:00 PM