* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PAROXETINE Paxil NEFAZODONE Serzone
Survey
Document related concepts
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Compounding wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Drug interaction wikipedia , lookup
Prescription costs wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
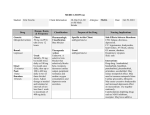
A NTIDEPRESSANTS NEFAZODONE 453 Serzone Pharmacology. Nefazodone is a postsynaptic serotonin 5-HT2A antagonist and presynaptic serotonin reuptake inhibitor. These two serotonergic effects make it different from SSRIs and TCAs.153–156 (See Antidepressants Comparison Chart.) Administration and Adult Dosage. PO for depression 100 mg bid initially (50 mg bid in the elderly), increasing q 4–7 days to the effective dosage range of 150– 300 mg bid. After initial dosage titration, once-daily bedtime administration is preferred to minimize daytime sedation.157 Dosage Forms. Tab 50, 100, 150, 200, 250 mg. Pharmacokinetics. Nefazodone has an oral bioavailability of about 20%. Singledose studies in the elderly have shown a 100% larger AUC; with multiple doses, the AUC differences decreased to 10–20% above those in younger populations. It is >99% protein bound and extensively metabolized, with a dose-dependent elimination half-life of about 1–2.3 hr in young patients, modestly prolonged in the elderly, and 2–3 times longer in hepatic disease. The major active metabolite, hydroxynefazodone, has a half-life of 1.2–1.6 hr in young and elderly patients, increasing to 2–4 hr with hepatic disease. Renal impairment does not markedly affect nefazodone pharmacokinetics. Adverse Reactions. Although chemically similar to trazodone, it causes less sedation and orthostatic hypotension, and its lower -adrenergic blockade makes priapism much less likely (no cases reported). Frequent adverse effects include sedation, dry mouth, nausea, and dizziness. Unlike SSRIs, nefazodone’s effects on sexual function, agitation, tremor, insomnia, and weight are no different from placebo. Drug Interactions. Nefazodone is a potent inhibitor of the CYP3A4 isoenzyme and a weak inhibitor of the CYP2D6 isoenzyme. Drug interactions of particular concern include the triazolobenzodiazepines (ie, alprazolam, triazolam, midazolam). A 1- to 2-week washout period is recommended when converting a patient to or from a MAOI and nefazodone. PAROXETINE Paxil Pharmacology. Paroxetine is a highly selective and potent inhibitor of serotonin reuptake (an SSRI) similar to fluoxetine.126,158–164 (See Antidepressants Comparison Chart.) Administration and Adult Dosage. PO for depression 20 mg/day; a few patients require 30–50 mg/day for full efficacy. PO for social anxiety disorder and panic disorder 10 mg/day initially; usual maintenance dosage is 20–60 mg/day. PO for OCD 20 mg/day initially; maintenance dosage is 40 mg/day to a maximum of 60 mg/day, preferably as a single dose in the morning or evening. The starting dosage for all uses in elderly patients and those with marked renal or hepatic impairment is 10 mg/day. For the elderly or those with severe renal or hepatic impairment, the maximum dosage is 40 mg/day. Dosage Forms. Tab 10, 20, 30, 40 mg; SR Tab 12.5, 25 mg; Susp 2 mg/mL. 454 C ENTRAL N ERVOUS S YSTEM D RUGS Pharmacokinetics. Paroxetine is completely orally bioavailable; protein binding is 93–95%. Unlike fluoxetine, paroxetine is metabolized to inactive metabolites and has an elimination half-life of 24 hr. Adverse Reactions. Paroxetine causes the typical SSRI adverse effects of nausea, sexual dysfunction, and headache but is more likely to cause sedation than insomnia and can cause more delay of orgasm or ejaculation and more impotence than other SSRIs.165 Like the other SSRIs, it is much safer in overdose than TCAs. Drug Interactions. Paroxetine is a potent inhibitor of CYP2D6, so most other antidepressants, antipsychotics, -blockers, and type Ic antiarrhythmics can have increased serum levels and adverse effects when paroxetine is combined with these drugs. Do not use paroxetine within 14 days of using an MAOI. REBOXETINE (Investigational—Pharmacia) Vestra Pharmacology. Reboxetine is the first in a new class of selective norepinephrine reuptake inhibitors with no affinity for serotonin or dopamine reuptake sites. It has negligible affinity for muscarinic, histaminic, or adrenergic receptors. This noradrenergic mechanism for antidepressant efficacy is similar to TCAs such as desipramine without the potential for appreciable adverse anticholinergic, cardiovascular, and sedative effects. It has efficacy for major depression equal to fluoxetine and desipramine.166,167 (See Antidepressants Comparison Chart.) Administration and Adult Dosage. PO for depression 8–10 mg/day given bid, 4–6 mg/day given bid in the elderly. Dosage Forms. Tab 4 mg (investigational). Pharmacokinetics. Reboxetine is rapidly absorbed. Metabolism occurs through three oxidative pathways: hydroxylation, dealkylation, and oxidation. The CYP450 isoenzymes responsible for metabolism have not been identified, and the degree of activity of the metabolites is unknown. Reboxetine has no inhibitory effect on CYP450 isoenzymes. Elimination half-life is 13 hr.166 Adverse Reactions. The most common adverse effects include dry mouth, constipation, increased sweating, insomnia, and urinary hesitancy, which are greater than placebo, but less frequent than imipramine. These “anticholinergic-like” effects are believed to result from increased norepinephrine levels. Side effects commonly associated with serotonin reuptake inhibitors such as nausea, anxiety or agitation, and daytime somnolence were no more common with reboxetine than with placebo.167 No information is available regarding reboxetine overdose in humans. SERTRALINE Zoloft Pharmacology. Sertraline is an SSRI similar to fluoxetine, which indirectly results in a downregulation of -adrenergic receptors. It has no clinically important effect on noradrenergic or histamine receptors and no effect on MAO. It lacks stimulant, cardiovascular, anticholinergic, and convulsant effects. Sertraline has antidepressant effects equal to TCAs and fluoxetine and might have anorectic effects and efficacy in OCD.130,168–170 (See Antidepressants Comparison Chart.) Administration and Adult Dosage. PO for depression, panic disorder, OCD, and posttraumatic stress disorder 50 mg/day initially, increasing if necessary at weekly intervals to a maximum of 200 mg/day in a single dose in the morning or evening. A NTIDEPRESSANTS 455 Dosage Forms. Tab 25, 50, 100 mg; Soln 20 mg/mL. Pharmacokinetics. Sertraline has an oral bioavailability of 36%, and, when it is taken with food, peak serum concentrations and bioavailability increase by 30–40%. Peak serum concentrations are reached in 6–8 hr. Sertraline concentrations in breast milk are the lowest of the SSRIs and produce minimal serum levels in the breast-fed infant.171 Its primary metabolite is N-desmethylsertraline, which has 5–10 times less activity than sertraline as an SSRI and has no demonstrated antidepressant activity. Cl is decreased by up to 40% in the elderly. Steady-state half-life is 27 hr. Adverse Reactions. Frequent adverse effects include nausea, diarrhea, ejaculatory delay, tremor, and increased sweating. It causes less agitation, anxiety, and insomnia than fluoxetine and is a less potent inhibitor of the CYP2D6 isoenzyme at a dosage of 50 mg/day. Use with caution in patients with renal or hepatic impairment and do not use it within 14 days of using an MAOI. SIADH has been reported.172 VENLAFAXINE Effexor Pharmacology. Venlafaxine is a potent reuptake inhibitor of serotonin and norepinephrine, like many TCAs, but lacks effects on muscarinic, -adrenergic, or histamine receptors.173–176 (See Antidepressants Comparison Chart.) Administration and Adult Dosage. PO for depression (immediate-release) 75 mg bid or tid initially, increasing q 4–7 days to an effective antidepressant dosage of 225–375 mg/day in 2 or 3 divided doses; (sustained-release) 75 mg once daily initially, increasing in increments of up to 75 mg/day at intervals of 4 or more days to a maximum of 225 mg/day. The sustained-release preparation does not reduce side effects but allows once-daily administration. PO for generalized anxiety disorder 75–225 mg/day in 2–3 divided doses. Patients with renal impairment or on hemodialysis require a 25–50% dosage reduction. Dosage Forms. Tab 25, 37.5, 50, 75, 100 mg; SR Cap 37.5, 75, 150 mg (Effexor XR). Pharmacokinetics. Venlafaxine is well absorbed orally; food has no effect on absorption. Serum concentrations in elderly patients are no different from those in younger patients. Unlike SSRIs, venlafaxine has minimal protein binding (27–30%). It undergoes extensive hepatic metabolism. Venlafaxine has an elimination half-life of 5 hr, and one major active metabolite has an 11-hr half-life. Venlafaxine exhibits linear pharmacokinetics over the recommended dosage range, and steady state is reached in 3 days. Adverse Reactions. Frequent adverse effects include expected serotonin-related effects (eg, nausea, headache, insomnia or somnolence, and sexual dysfunction). At higher dosages (375 mg/day), venlafaxine is unique in causing a consistent but mild elevation in diastolic blood pressure (6 mm Hg). Regular blood pressure monitoring is required for all patients. Drug Interactions. Venlafaxine is not a potent inhibitor of the cytochrome P450 enzyme system, making it different from most of the SSRIs. Avoid it in patients who have received an MAOI within the past 14 days. 5.qxd 456 ANTIDEPRESSANTS COMPARISON CHARTa THERAPEUTIC SERUM LEVELS (µG/L) Sedation 15–45 b Moderate None None 300–450 b None None None 300–600 b Low Low Low Tab 15 mg. 45–90 b Moderate Low Very High Tab 10 mg. 30–60 b Low Low Very High 8–10 b Very Low Low Very Low DOSAGE FORMS RELATIVE FREQUENCY OF SIDE EFFECTS Anticholinergic Orthostatic Hypotension α2-ADRENERGIC BLOCKERS Tab (conventional and rapidly dissolving) 15, 30, 45 mg. 2:00 PM Mirtazapine Remeron CHLOROPROPIOPHENONES Tab 75, 100 mg SR Tab 100, 150 mg. Page 456 Bupropion Wellbutrin Zyban DIBENZOXAZEPINESc Amoxapine Asendin Various Tab 25, 50, 100, 150 mg. MONOAMINE OXIDASE INHIBITORS (MAOIs) Phenelzine Nardil Tranylcypromine Parnate MORPHOLINES Reboxetine Vestra 8/13/2001 USUAL DAILY ADULT DOSAGE RANGE (MG) CLASS AND DRUG (continued ) 5.qxd ANTIDEPRESSANTS COMPARISON CHARTa (continued ) DOSAGE FORMS USUAL DAILY ADULT DOSAGE RANGE (MG) THERAPEUTIC SERUM LEVELS (µG/L) RELATIVE FREQUENCY OF SIDE EFFECTS Sedation Anticholinergic Orthostatic Hypotension SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) Tab 20, 40 mg Soln 2 mg/mL. 20–60 b Very Low Very Low None Fluoxetine Prozac Cap, Tab 10, 20, 40 mg SR Cap 90 mg Soln 4 mg/mL Tab 10 mg. 10–80 b None Very Low None Fluvoxamine Luvox Tab 25, 50, 100 mg. 100–300d b None None None Paroxetine Paxil Tab 10, 20, 30, 40 mg SR Tab 12.5, 25 mg Susp 2 mg/mL. 20–50 b Low Low Very Low Sertraline Zoloft Tab 25, 50, 100 mg Soln 20 mg/mL. 50–200 b None None None 2:00 PM Citalopram Celexa Tab 25, 37.5, 50, 75, 100 mg SR Cap 37.5, 75, 150 mg. 225–375 b Very Low Very Low Very Low Tab 25, 50, 75 mg. 150–225 200–300b Moderate Moderate Moderate TETRACYCLICS c 457 Maprotiline Ludiomil Various (continued ) Page 457 SEROTONIN NOREPINEPHRINE REUPTAKE INHIBITORS (SNRIs) Venlafaxine Effexor Effexor XR 8/13/2001 CLASS AND DRUG 5.qxd 458 ANTIDEPRESSANTS COMPARISON CHARTa (continued ) DOSAGE FORMS USUAL DAILY ADULT DOSAGE RANGE (MG) THERAPEUTIC SERUM LEVELS (µG/L) RELATIVE FREQUENCY OF SIDE EFFECTS Sedation Anticholinergic Orthostatic Hypotension TRIAZOLOPYRIDINES Tab 50, 100, 150, 300 mg. 50–100 (hypnotic) 200–400 (antidepressant) b High Very Low High Nefazodone Serzone Tab 50, 100, 150, 200, 250 mg. 300–600 b Moderate Very low Moderate Amitriptyline Elavil Various Tab 10, 25, 50, 75, 100, 150 mg Inj 10 mg/mL. 150–300 75–175e High High High Clomipramine Anafranil Various Cap 25, 50, 75 mg. 100–250d 100–150f b High High High Desipramine Norpramin Various Tab 10, 25, 50, 75, 100, 150 mg. 150–300 100–160 Low Low Moderate Doxepin Adapin Sinequan Various Cap 10, 25, 50, 75, 100, 150 mg Soln 10 mg/mL. 150–300 110–250e High Moderate High 2:00 PM Trazodone Desyrel Various 8/13/2001 CLASS AND DRUG Page 458 TRICYCLICS (TCAs)d (continued ) 5.qxd ANTIDEPRESSANTS COMPARISON CHARTa (continued ) DOSAGE FORMS USUAL DAILY ADULT DOSAGE RANGE (MG) THERAPEUTIC SERUM LEVELS (MG/L) RELATIVE FREQUENCY OF SIDE EFFECTS Sedation Anticholinergic Orthostatic Hypotension 150–300 >200e Moderate Moderate High Nortriptyline Aventyl Pamelor Various Cap 10, 25, 50, 75 mg Soln 2 mg/mL. 100–200 50–150 Moderate Moderate Low Protriptyline Vivactil Various Tab 5, 10 mg. 30–60 70–260b Very Low Moderate Moderate Trimipramine Surmontil Cap 25, 50, 100 mg. 150–300 b Moderate Moderate High 459 a Antidepressants with serotonergic activity (SSRIs, nefazodone, venlafaxine, and mirtazapine) have established efficacy for many indications other than depression. Some have received approval from the Food and Drug Administration for generalized anxiety disorder, bulimia nervosa, obsessive-compulsive disorder, social phobia, panic disorder, posttraumatic stress disorder, and premenstrual dysphoric disorder. Effective doses for major depression for most patients are in the low to moderate ranges listed, which is also true for generalized anxiety disorder, social phobia, panic disorder, and premenstrual dysphoric disorder. The middle to high end of the listed dosage ranges is usually necessary for efficacy when treating bulimia nervosa, obsessivecompulsive disorder, and posttraumatic stress disorder.180 b Not well established. c Amoxapine, maprotiline, and the tricyclic antidepressants are categorized together as heterocyclic antidepressants because their therapeutic and side effect profiles are similar. d For obsessive-compulsive disorder. e Includes active metabolites. f Major depression. From references 106, 112, 122, 126, 127, 140, 141, 145, 146, 148, 153, 159, 160, 175, and 177–179. Page 459 Tab 10, 25, 50 mg Cap (as pamoate) 75, 100, 125, 150 mg. 2:00 PM Imipramine Tofranil Janimine Various 8/13/2001 CLASS AND DRUG 460 C ENTRAL N ERVOUS S YSTEM D RUGS Antipsychotic Drugs Class Instructions. Antipsychotics. This drug can cause drowsiness. Until the extent of this effect is known, use caution when driving, operating machinery, or performing other tasks requiring mental alertness. Avoid excessive concurrent use of alcohol or other drugs that cause drowsiness. Missed Doses. If you miss a dose, take it as soon as you remember. If it is almost time for your next dose, skip it and resume your normal schedule. Do not double doses. ANTIPSYCHOTIC DRUGS Pharmacology. Antipsychotic efficacy is most likely related to blockade of postsynaptic dopaminergic receptors in the mesolimbic and prefrontal cortexes of the brain, although other neurotransmitter systems also are involved.181 Administration and Adult Dosage. (See Antipsychotic Drugs Comparison Chart for oral dosage ranges.) Initiate therapy with divided doses until therapeutic dosage is found; then, for most patients, once-daily hs administration is preferred. For maintenance, decrease acute dosage by 25% q 3 months, with a target maintenance dosage being 50–67% of the acute treatment dosage.182 Recent concern has focused on the need to establish a minimum effective dosage for antipsychotic drugs, and treatment regimens at the low end of the dosage range are preferred. Oral dosages of high-potency antipsychotics (eg, fluphenazine, haloperidol) in the range of 5–20 mg/day are better tolerated and equal in efficacy to dosages >20 mg/day.183 Most patients can be given a maintenance dosage of 50% the acute dosage by the end of 1 yr, although 10–15% of chronically ill patients require a maintenance dosage >15 mg/day of haloperidol or its equivalent.184,185 For manic episodes, no additional benefit is achieved with dosages >10 mg/day of haloperidol.186 Mesoridazine and thioridazine are indicated only in patients who fail with other drugs because of inefficacy or intolerable side effects. Special Populations. Pediatric Dosage. As with adults, dosage is determined primarily by titration to individual response. No precise dosage range exists, but in general the initial dosage is lower and increased more gradually in children. Geriatric Dosage. Initial dosage is 20–25% of the dosage used in younger adults. Typical starting dosages in the elderly are haloperidol 0.5–2 mg/day. Dosage adjustments also must be done more slowly than in younger adults.187 Other Conditions. Dosages in the lower range are sufficient for most elderly patients, and the rate of dosage titration is slower. Dosage Forms. (See Antipsychotic Drugs Comparison Chart.) Patient Instructions. (See Antipsychotics Class Instructions.) These drugs usually take several weeks for clinical response and up to 8 weeks for full therapeutic response. Pharmacokinetics. Onset and Duration. Onset of antipsychotic activity is variable, with noticeable response requiring days to weeks. Serum Levels. Correlation of serum levels with clinical response is not consistently established. The best evidence exists for haloperidol, with serum concen-