* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Gastrointestinal Tract 07
Survey
Document related concepts
Transcript
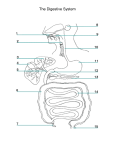
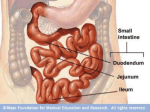
Gastrointestinal Tract (Effective February 2007) (1%-5%) Anatomy of GI Tract Esophagus • bulls-eye or “target” • EG junction seen on sagittal scan posterior to left lobe of liver and anterior to aorta Anatomy of GI Tract Stomach – stores food and aids in digestion • Fundus • body or corpus – lesser curvature – greater curvature • Pylorus – Antrum – canal or bulb 1 supporting ligaments greater curvature • greater omentum • gastrophrenic ligament • gastrosplenic ligament • lienorenal ligament. lesser curvature • gastrohepatic ligament • lesser omentum. Small intestines Most of the digestion and absorption of food takes place (pancreatic enzymes and bile) • three parts: duodenum, jejunum, and ileum. – • about 23 feet long and 1 inch wide avalvulae conniventes (valves of Kerckring) – linear echoes representing mucosal folds spaced 3 – 5mm apart that slow down the passage of food to create a greater absorbing area → “Keyboard sign” duodenum is divided into four parts • #1 pylorus and runs upward and backward on the right side of the first lumbar vertebra #2 runs anterior to the right kidney on the right side of the second and third lumbar vertebrae • – The common bile duct and main pancreatic duct pierce the duodenal wall midway down its posterior aspect. 2 duodenum is divided into four parts • • #3 horizontally to the left, following the inferior margin of the pancreatic head #4 runs upward and to the left, and then runs forward at the duodenojejunal junction. – ligament of Treitz ascends to the right crus and holds the junction in position Jejunum and Ileum • jejunum arises from the duodenum and extends for 2 m • inner walls – – circular folds of the mucous membrane, – villi; the valvulae conniventes are large folds of mucous membrane • ileocecal orifice – marks the entry into the large intestine and serves as a landmark to find the appendix. Large Intestine • divided into the – – – – – – – vermiform appendix Cecum ascending (to hepatic flexure) Transverse descending (to splenic flexure) colon, rectum. The colon is divided into segments called haustra.Ψ 3 Vascular Supply Esophagus • inferior thyroid branch supplies the upper esophagus. • The descending thoracic aorta supplies the midesophagus • The left inferior phrenic artery supplies the lower end of the esophagus. Varices may arise from gastroesophageal arteries. Vascular Supply Stomach • branches of the hepatic artery, – • right gastric arterial branch, the pyloric and right gastroepiploic left gastric artery. Gastrointestinal Tract The five layers of bowel: • Mucosa: directly contacts intraluminal contents; line with epithelial folds, echogenic • Submucosa: contains blood vessels and lymph channels • Muscularis: contains circular and longitudinal bands of fiber • • Serosa: thin, loose layer of connective tissue Mesothelium: covers intraperitoneal bowel loops 4 Measurements • wall of the GI tract should measure <5 mm, or <3 mm when distended – from the edge of the echogenic core to the outer border of the anechoic halo Stomach • Could look like cystic mass in LUQ • GE Junction seen to the left of the midline as a bull’s-eye or target structure • gastric antrum can be seen as a target in the midline Duodenum • Usually, a gas- or fluid-filled duodenal cap is seen lateral to the pancreatic head. 5 Small Bowel • fluid or contrast media filled small bowel can visualize the valvulae conniventes – seen as linear echo densities spaced 3 to 5 mm apart – known as a keyboard sign – The small bowel wall is <3 mm thick. Appendix • located on the abdominal wall under McBurney’s point. – McBurney’s point - drawing a line from the right ASIS to the umbilicus—at the midpoint of this line lies the root of the appendix. Ψ • Fusiform structure <6 mm in caliber, 8 to 10 cm long Ψ Appendix Technique • high-resolution linear array transducer should be used • Graded compression over the area of maximum tenderness • visibility of the retrocecal and paracecal areas is improved by displacing gas and other bowel loop contents from the scanning field 6 Abnormalities of the Appendix • appendicitis – lesion in the RLQ. – noncompressible mass – diameter is >6 mm – muscular wall thickness is >3 mm. Abnormalities of the Appendix • Perforation or Abscess – loculated pericecal fluid – prominent pericecal fat – circumferential loss of the submucosal layer of the appendix. • Crohn’s Appendicitis – With Crohn’s ileocolitis the appendix may be involved 25% of the time Abnormalities of the Appendix Appendiceal Tumors • Primary adenocarcinomas of the appendix are rare. • A primary adenocarcinoma may manifest as acute appendicitis with perforation. • Often only seen by pathologist 7 Colon • haustral markings 3 to 5 cm apart in the ascending and transverse colon When fluid filled • descending colon appears as a tubular structure with an echogenic border. • Layers of the colon : – mucosa, submucosa, muscularis propria, serosa, and subserous fatty tissue. Benign Tumors Polyp • seen with fluid distention of the stomach – solid masses adherent to the gastric wall • Leiomyomas – most common tumor of the stomach – hypoechoic mass continuous with the muscular layer of the stomach Malignant Tumors Gastric Carcinoma • 90-95% malignant tumors of the stomach are carcinomas • ½ of the tumors occur in the pylorus, and ¼ in the body and fundus. • ultrasound study will show – a target or pseudokidney sign Ψ – possibly gastric wall thickening. 8 Malignant Tumors • Leiomyosarcoma – second most common gastric sarcoma – globular or irregular and may become huge – outstrips blood supply → central necrosis → cystic degeneration and cavitation. • Metastatic Disease – rare - originates as melanoma or lung or breast cancer. Crohn’s Disease Ψ • AKA regional enteritis – recurrent granulomatous inflammatory disease that affects the terminal ileum and/or any level of the colon. • involves entire thickness of the bowel wall. • Physical symptoms include diarrhea, fever, and RLQ pain.Ψ • There is rigidity to pressure exerted from the transducer. • Peristalsis is absent or sluggish. • There is dilation with hyperperistalsis and water and air stasis. 9 Laboratory values Gastrin • blood hormone – stimulates intestinal movement and secretion of juices – elevates in acute and chronic peptic ulcer disease Serum Amylase • elevates in intestinal obstruction, perforated ulcers; pancreatitis Feces • examined for presence of blood, fat, bile, and • parasites Hernia Peritoneal Fluid (including Inflammatory Fluid Collections) 10