* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Echocardiographic Variables After Left Ventricular Assist Device
Remote ischemic conditioning wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Artificial heart valve wikipedia , lookup
Aortic stenosis wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
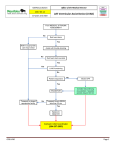
Echocardiographic Variables After Left Ventricular Assist Device Implantation Associated With Adverse Outcome Yan Topilsky, MD; Tal Hasin, MD; Jae K. Oh, MD; Daniel D. Borgeson, MD; Barry A. Boilson, MD; John A. Schirger, MD; Alfredo L. Clavell, MD; Robert P. Frantz, MD; Rayji Tsutsui, MD; Mingya Liu, MD; Simon Maltais, MD; Sudhir S. Kushwaha, MD; Naveen L. Pereira, MD; Soon J. Park, MD Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Background—Operative mortality after left ventricular assist device (LVAD) implantation is heavily influenced by patient selection and the technical difficulty of surgery. However, how we treat our patients and LVAD setting may affect the patient outcome beyond this period. We postulated that the presence of echocardiographic variables 1 month after surgery suggesting appropriate degree of LV unloading and an adequate forward flow would be important in determining clinical outcomes after the initial successful LVAD implantation. Methods and Results—We retrospectively analyzed various variables in echocardiographic examinations performed 30 days after LVAD implant in 76 consecutive patients receiving continuous flow device for their association with a compound end point (90-day mortality, readmission for heart failure, or New York Heart Association class III or higher at the end of the 90-day period). The echocardiographic associations examined included estimated LVAD flow, with and without native LV contribution, interventricular septal position, the status of aortic valve opening, an estimated left atrial pressure (ELAP), the mitral flow E-wave deceleration time, and the ratio of deceleration time to E-wave velocity (mitral deceleration index [MDI]). Four patients died during the 30- to 90-day period, 6 patients were readmitted for heart failure, and 25 patients were considered to have New York Heart Association class III or higher at the end of the 90-day period. Variables associated with adverse outcome included increased ELAP (odds ratio, 1.30 [1.16 –1.48]; P⬍0.0001), MDI ⬍2 ms/[cm/s] (odds ratio, 4.4 implantation [1.22–18]; P⫽0.02) and decreased tricuspid lateral annulus velocity (odds ratio, 0.70 implantation [0.48 – 0.95]; P⫽0.02). A leftward deviation of interventricular septum was associated with a worse outcome (odds ratio, 3.03 implantation [1.21–13.3]; P⫽0.01). Conclusions—Mortality and heart failure after LVAD surgery appear to be predominantly determined by echocardiographic evidence of inefficient unloading of the left ventricle and persistence of right ventricular dysfunction. Increased estimated LA pressure and short MDI are associated with worse mid term outcome. Leftward deviation of the septum is associated with worse outcome as well. (Circ Cardiovasc Imaging. 2011;4:648-661.) Key Words: left ventricular assist device 䡲 echocardiography L unloading may be associated with failure to improve heart failure symptoms after LVAD surgery. Furthermore, other factors, especially those related to right ventricle (RV) function, may have a strong influence as well, as RV performance is the limiting factor of total cardiac output after LVAD implantation. We retrospectively examined various echocardiographic and clinical variables 30 days after LVAD implantation for their association with lack of improvement in heart failure 3 months after discharge from hospital. eft ventricular assist devices (LVAD) are designed for mechanical support for patients with severe systolic heart failure and provide effective long term circulatory support.1– 4 In most cases, axial flow pumps have replaced pulsatile LVADs because of improved survival and less device failure.5,6 Postoperative transthoracic echocardiography (TTE) has a major role in the treatment of LVAD patients. It is frequently used to evaluate native heart and LVAD function and for troubleshooting possible device malfunctions.7–11 Although continuous LVAD therapy has been in clinical use for a number of years, a comprehensive analysis of post operative echocardiographic variables associated with failure of therapy has not been reported to date. Because LVAD therapy is supposed to improve cardiac output and unload the left cardiac chambers, we postulated that variables estimating total or LVAD output, as well as those estimating the efficiency of left ventricular or left atrial Clinical Perspective on p 661 Methods Patient Population, LVAD Pump Setting, and Study Design The study cohort included 76 consecutive patients (62 males, 14 females) undergoing LVAD (HeartMate II) implantation in our Received March 22, 2011; accepted August 15, 2011. From the Division of Cardiovascular Diseases (Y.T., T.H., J.K.O., D.D.B., B.A.B., J.A.S., A.L.C., R.P.F., R.T., M.L., S.S.K., N.L.P.) and the Division of Cardiovascular Surgery (S.M., S.J.P.), Mayo Clinic, Rochester, MN. Correspondence to Soon J. Park, MD, FACC, Mayo Clinic, St Marys Hospital, 2nd St SW GO-138SE, Rochester, MN 55902. E-mail [email protected] © 2011 American Heart Association, Inc. Circ Cardiovasc Imaging is available at http://circimaging.ahajournals.org 648 DOI: 10.1161/CIRCIMAGING.111.965335 Topilsky et al Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 institution between February 2007 and August 2010. Our practice of patient selection, surgical techniques, preoperative and postoperative treatments, and follow-up care remained constant over time. Transesophageal echocardiography was routinely utilized in all patients to help us with the revolutions per minute (rpm) setting in the operating room. The initial pump speed was selected to provide an adequate forward flow (cardiac index measured by Swan-Ganz catheter ⬎2.2 L/min/m2), while ensuring the absence of LV collapse under TEE guidance. Subsequently, the patients were discharged home after optimizing their LVAD settings so that pump speed was 0 – 400 rpm below the rpm in which their aortic valve remained closed during the entire systole. We retrospectively analyzed different variables in echocardiographic examinations performed 1 month after LVAD implantation for their association with the composite end point of persistence of New York Heart Association (NYHA) class III or higher, readmission for heart failure during the 30- to 90-day period or death at 90 days as the primary aim of the study. Only variables obtained at 1 month after LVAD implantation were used for our analysis. The LVAD speed was maintained between discharge and the 1 month evaluation in all patients. However, during the subsequent 3 months of follow-up, the rpms were changed in some of the patients with heart failure symptoms and echocardiographic evidence of inefficient LV unloading. Any patient with symptoms of heart failure during the follow-up period, with or without rpm increased, was included in the adverse outcome group. LV and Valvular Echocardiographic Measurements Two-dimensional transthoracic echocardiography was performed in a standard manner using Sonos 5500 (Philips Medical Systems, Andover, MA), Sequoia 512 (Siemens, Mountainview, CA), or Vivid 7 (GE Medical Systems, Milwaukee, WI). LV diameters and interventricular septal and posterior wall width were measured from the parasternal short axis using 2D, or 2D guided M-Mode echocardiogram of the LV at the papillary muscle level using the parasternal short-axis view from the trailing edge of the septum to the leading edge of the posterior wall as recommended.12 Ejection fraction was calculated by the Quinones method13 assuming an akinetic apex, and LV mass was calculated by the method proposed by Devereux and associates,14 using the same LV dimensions made with M-mode or 2D as described above. Valvular regurgitation was qualitatively assessed using color Doppler according to the guidelines of the American Society of Echocardiography (normal/trivial⫽1, mild⫽2, moderate⫽3, severe⫽4).15 RV Echocardiographic Measurements RV chamber size and function was measured according to the guidelines of the American Society of Echocardiography.12 RV size and systolic function were evaluated by measuring the RV end-diastolic area (4-chamber view), RV end-systolic area (4 chamber view), tricuspid annulus end systolic diameter (4-chamber view), and calculating the RV fractional area change. RV function was qualitatively graded using a 4-scale grading system (normal, mild, moderate, severe) using all apical views, RV inflow, parasternal long-axis, parasternal short-axis, and subcostal views. Care was taken to obtain a true nonforshortened apical or para-apical 4-chamber view, oriented to obtain the maximum RV dimension before making the RV estimation.12 RV function was then assessed by 3 other methods: 2D lateral tricuspid annular motion,16 the timing interval between the cessation and the onset of tricuspid regurgitation flow corrected for heart rate (TRDc), using the formula TRDc⫽TR flow time/公RR,17 a surrogate for early systolic equalization of RV and right atrial pressure and the RV index of myocardial performance (RIMP), as previously described by others.18,19 Mean pulmonary artery pressure was estimated using the modified Bernoulli formula (4⫻TRVmax2)⫹RAP, where TR Vmax is the peak systolic tricuspid regurgitation velocity at end expiration, and RAP is the right atrial pressure. Post-LVAD Echo Variables 649 LVAD Echocardiographic Variables Measurements of the LVAD components were performed, including the inflow cannula, outflow graft flow velocities, and variables estimating the LVAD flow and efficiency of left sided chamber unloading17,20,21 (Figures 1, 2, 3, and 4). Inflow Cannula The inflow cannula and its orientation within the left ventricular apex was visualized on the apical 4- and 2-chamber views, and sometimes required off-axis imaging as well.21,22 Doppler assessment of the inflow cannula was done in the 4- and 2-chamber views as well, as they are usually aligned with the central axis of a properly positioned inflow cannula. Continuous or pulsed Doppler was used for measurement of the maximal velocity along the inflow pathway from the ventricle to the LVAD (Figure 1). Outflow Cannula Interrogation of the outflow cannula was performed from the high left parasternal long-axis view, which shows the end-to-side anastomosis of the outflow cannula to the mid ascending aorta, and the right parasternal view, which shows the long axis of the outflow cannula traversing from the pump toward the right aspect of the ascending aorta.21 Color flow, PW, and CW Doppler was used to evaluate flow patterns of the outflow cannula. To measure flow velocity the PW sample volume was positioned at least 1 cm proximal to the aortic anastomosis and the flow was recorded away or toward the transducer, depending on the transducer position. For the right parasternal view, the patient was positioned on his right side, and the image recorded with the transducer immediately rightward to the sternum (Figure 1). LVAD Output The product of a pulsed-wave spectral Doppler velocity-time integral (VTI) from the outflow cannula and its cross-sectional area equals the flow volume created by the pump. This technique is well known and was recently validated with the Heart Mate II in a wellconducted in vitro study.23 The same method was applied here to calculate the LVAD minute flow rate. LVAD outflow cannula diameter was measured in the right parasternal view, and outflow TVI was measured using the right parasternal view or the high left parasternal view, depending on which view afforded the lowest Doppler angle of interrogation.21 Total Cardiac Output The RVOT VTI was measured from pulse-wave Doppler, and RVOT diameter was measured from the parasternal short axis at the level of the great arteries. Total RV output (which is the sum of LVAD output and the flow ejected through the LVOT) was calculated using the formula (RV outflow diameter/2)2⫻⫻RV outflow TVI.12 Right Atrial Pressure Estimation Right atrial (RA) pressure was estimated by the inferior vena cava diameter as well as its response to inspiration as previously described.24 Briefly, expiratory and inspiratory inferior vena cava (IVC) diameters and percent collapse were measured in subcostal views within 2 cm of the right atrium. IVC diameter ⬍2.1 cm that collapsed ⬎50% with a sniff suggested a normal RA pressure (assigned as 5 mm Hg), whereas an IVC diameter ⬎2.1 cm that collapsed ⬍50% with a sniff suggested a high RA pressure (15 mm Hg). In patients with IVC diameter ⬍2.1 cm and no collapse (⬍20%) with a sniff, RA pressure was upgraded to 20 mm Hg. In indeterminate cases in which the IVC diameter and collapse did not fit this paradigm, secondary indices of elevated RA pressure were integrated. If uncertainty remained, RA pressure was left as intermediate value of 10 mm Hg. Efficiency of LV Unloading Several echocardiographic variables have been evaluated for the assessment of optimal unloading of left-sided chambers. These include the following: 650 Circ Cardiovasc Imaging November 2011 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Figure 1. A, Interrogation of the inflow cannula. The inflow cannula and its orientation within the left ventricular (LV) apex visualized on the apical 4-chamber view, aligned with the LV inflow tract, not touching any wall. B, Pulsed Doppler assessment showing laminar, low velocity forward flow without regurgitation with a pulsatile inflow pattern because the pump inflow originates from the beating LV, resulting in periodic changes in flow throughout the cardiac cycle, reaching a maximum during systole (S), and minimum during diastole (D). The difference between systolic to diastolic inflow velocities is related to LV contraction in a geometry-independent way. C, Interrogation of the outflow cannula in the high left parasternal long-axis view showing the end-to-side anastomosis of the outflow cannula to the mid ascending aorta. D, Interrogation of the outflow cannula in the mid right parasternal view as it transverses upward toward the ascending aorta. In the mid sternum the cannula is parallel to the transducer and its diameter can be easily measured. E, We follow the outflow cannula to the high parasternal area. The flow will change direction away from the transducer (blue) bending toward the ascending aorta. F, This is usually the best view to measure flow velocity with the PW sample (the angle of interrogation will be optimal) positioned at least 1 cm proximal to the aortic anastomosis, the flow moving away from the transducer. AO indicates ascending aorta; OC, outflow cannula. (1) Left ventricular dimension in end diastole (LVEDD) and end systole (LVESD),25 and the change in both calculated as (LVEDD pre LVAD⫺LVEDD post LVAD)/LVEDD pre LVAD or (LVESD pre LVAD⫺LVESD post LVAD)/ LVESD pre LVAD, respectively. (2) Preserving a neutral position of the interventricular septum, not shifting to the right or to the left26 (Figure 2). (3) Degree of aortic valve opening (closed, opens intermittently every 1:3 cycles, opens every cycle).26,27 We assessed novel variables for proper unloading of left-sided chambers. These included: (1) Estimation of the mean left atrial (LA) pressure by a multistep process including the following: First we estimated the mean right atrial pressure by the inferior vena cava diameter as well as its response to inspiration.24 Second we checked the interatrial position at diastole using the left parasternal shortaxis view and/or 4-chamber views and defined it as deviated to the right, neutral, or deviated to the left. The interatrial septum (IAS) is a thin membranous structure between the left and right atria, and its configuration is altered by minor changes of up to 5 mm Hg in the interatrial pressure gradient.28 –30 When LA pressure is higher than the right, the IAS configuration is convex toward the right atrium and if right atrial pressure is higher than the left, the IAS is convex toward the left atrium. Thus, we arbitrarily estimated the mean LA pressure as LA pressure⫽RA pressure if inter atrial septum was neutral, LA⫽RA pressure⫺5 mm Hg if interatrial position was deviated to the left and LA pressure⫽RA pressure⫹5 mm Hg if inter atrial position was deviated to the right (Figure 3). (2) Mitral inflow deceleration time is negatively related to left ventricular filling pressure.31,32 For any given rate of deceleration of early mitral inflow, a higher E-wave velocity is associated with increased deceleration time.33 To correct for this potential artifact, we indexed the deceleration time for peak E-wave velocity (mitral deceleration index [MDI]) as previously described,33,34 and hypothesized that it may be a useful marker of LV unloading in patients with continuous LVAD (Figure 4). Echocardiographic Determinants of Outcome The associations used as potential determinants of outcome included left ventricular diastolic diameter (mm), left ventricular systolic diameter (mm), color Doppler qualitative grading of mitral regurgitation, aortic regurgitation and tricuspid regurgitation (TR), vena contracta of TR, tricuspid regurgitation velocity (m/s), tricuspid lateral annulus velocity, qualitatively estimated RV function, RIMP, RV end-diastolic and end-systolic area, RV fractional area shortening, total cardiac output, LVAD output, inflow and outflow cannula velocities, mitral inflow deceleration time, mitral inflow deceleration time divided by E-wave velocity (MDI), interventricular septal position, interatrial septal position, aortic valve opening status, estimated RA pressure, estimated LA pressure (ELAP), and the change in LV end diastolic and end-systolic diameters from the baseline measurements performed before LVAD implantation. Tricuspid and Aortic Valve Procedures Candidates for LVAD implantation are evaluated by echocardiography to assess native tricuspid valve regurgitation (TR) and aortic regurgitation (AR). Those with at least moderate TR (jet area/right atrial area ⱖ20%, or vena contracta ⬎4.5 mm) underwent tricuspid Topilsky et al Post-LVAD Echo Variables 651 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Figure 2. Apical 4-chamber view assessing the interventricular septal position in different patients after left ventricular assist device (LVAD) implantation. A, Inefficient left ventricular (LV) unloading with interatrial and interventricular septa deviated to the right, suggesting high left atrial (LA) and LV pressure. B, Interventricular septum deviated to the left, suggesting markedly unloaded LV that can be associated with adverse outcomes, right ventricular (RV) dysfunction, and functional TR. C, Interventricular septum is neutral suggesting efficient LV decompression. Note that the interatrial septum is deviated to the left as opposed to the interventricular septum. This is because the interatrial septum is thinner than the thick muscular interventricular septum and the relation between the interatrial position and the pressure difference between the right atrium and the left atrium is much tighter than between the right and left ventricles. A patient is shown before (D) and after (E) increasing the pump’s speed. D, The patient was admitted due to persistent heart failure. On echo examination, both interatrial (large arrow) and interventricular septa (small arrows) were deviated to the right suggesting inefficient unloading of left chamber. Note the significant functional mitral regurgitation. E, After optimization of pump’s speed the interatrial septum is deviated to the left (large arrow) but the interventricular septum maintains a neutral position (small arrows), suggesting optimal unloading of left chambers. Note the functional mitral regurgitation has improved considerably, as did the patient’s symptoms. valve repair or replacement. Those with aortic insufficiency due to significant structural defects in the aortic valve underwent aortic valve replacement or patch closure of the valve. However, the majority of the patients with aortic insufficiency were corrected with a simple coaptation stitch placed at the central portion of the aortic cusps as previously described.35,36 Interobserver and Intraobserver Variability Interobserver variability was assessed by comparing the readings made by another independent echocardiographer in 10 randomly selected patients. Intraobserver variability was determined by having the first observer who measured the data in all patients remeasure the velocities in 10 patients at least 3 month apart. Interobserver and intraobserver variability were assessed by the correlation coefficient (r value) between the matched parameters, paired t test to evaluate the difference between these measurements (P⬍0.05 for a significant difference) the Bland-Altman method and by the within-subject coefficient of variation. The within-subject coefficient of variation (calculated as ratio of the standard deviation of the measurement difference to the mean value of all measurements) provides a scale-free unitless estimate of variation expressed as a percentage. We measured the intra- and interobserver reproducibility for the deceleration time, the MDI, and estimated LA pressure, and expressed them using the coefficient of variation. Statistical Analysis Data were checked visually looking for heavy tails or outliers and analyzed using the Shaprio-Wilk test for normality. Continuous normally distributed variables were presented as mean⫾SD and compared using the Student t test. Ordinal and/or nonnormally distributed data were presented by median, 1st and 3rd quartiles and compared using the nonparametric Wilcoxon rank sum test. Categorical data were compared between groups using the 2 or Fisher exact test, as appropriate. To analyze potential factors that are associated with the adverse combined 90-day outcome individual-predictor analyses based on logistic regression were performed on various variables (clinical and echocardiographic). The associations between wedge pressure and ELAP or MDI in 8 patients in which an invasive right heart catheterization was performed simultaneously with the echocardiographic examination were assessed using the Pearson correlation coefficient. All probability values were 2-sided, and values of ⬍0.05 were considered to indicate statistical significance. All data were analyzed with the JMP System software version (SAS Institute, Inc, Cary, NC). All authors participated in designing the study, collecting and analyzing data, and drafting and revising the manuscript. The authors had full access to and take full responsibility for the integrity of the data. All authors have read and agreed to the manuscript as written. Results Baseline Characteristics Table 1 shows the baseline characteristics (before LVAD implantation) of the patients enrolled, divided into 2 groups, those (30 patients) with adverse LVAD outcomes 90 days after surgery (mortality or admission for heart failure during the 90-day period, or persistence of NYHA class III or higher at the end of the period), and those (46 patients) considered to have normal 90-day outcome. The patients’ mean age was 63.2⫾12 years, and 80.0% were men. The most common etiology for heart failure was ischemic heart disease (51%) followed by dilated cardiomyopathy (38%). Eleven percent of patients (8 patients) had restrictive cardiomyopathy as the indication for LVAD surgery.35 Most patients (65%) were implanted for destination therapy. Most patients were Caucasian, 39% had hypertension and 27% had diabetes. We have calculated and included the clinical score proposed by Lietz-Miller37 for all patients (Table 1). 652 Circ Cardiovasc Imaging November 2011 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Figure 3. A through C, A patient was readmitted for persistent heart failure 30 days after left ventricular assist device (LVAD) surgery. A, M-mode examination of the aortic valve affirms permanent closure of the valve suggesting efficient decompression of the left ventricle. B, Short-axis view on the level of great arteries shows an interatrial septum deviated to the right, suggesting that the left atrial pressure is higher than right atrial pressure. C, Subcostal view showing a dilated inferior vena cava with a less than 50% change during inspiration. The right atrial pressure was estimated to be 15 mm Hg, suggesting that left atrial pressure is even higher. D, The pump’s speed was increased by 600 rpm, resulting in a left atrial septum deviated to the left. E, Four-chamber view showed that the interventricular septum is not deviated to the left. F, Echo performed 24 hours after the change in pump’s speed showed that the right atrial pressure has decreased (the inferior vena cava is not dilated and collapses during inspiration). The interatrial septum was neutral, suggesting normally decompressed left atrium estimated to be 5 mm Hg. The pre LVAD echocardiographic variables associated with worse outcome included a smaller LV end-systolic diameter, lower TR velocity, shorter TRDc, and lower hemoglobin. Variables estimating LV systolic function, and LV filling pressures before LVAD surgery were not different between the groups. These results are consistent with our previous report assessing pre LVAD echocardiographic predictors of adverse outcome after LVAD surgery.17 Ninety-Day Post-LVAD Adverse Outcomes Table 2 compares the echocardiographic, functional, laboratory, and pump variables measured 30 days after surgery between patients with and without the compound 90-day adverse outcome. We divided the echocardiographic variables into those assessing the native left ventricle, valves, right ventricle, LV unloading, and pump flows. Four patients died between days 30 to 90 after surgery. The causes of deaths included uncontrolled right heart failure and multiorgan failure in 3 and intracerebellar bleeding in 1. Six patients were readmitted for heart failure, 25 patients were considered to have NYHA class III or higher at the end of the 90-day period. None of the variables assessing the valve function, native left ventricle function, or size at the 30 days examination showed significant association with 90-day outcome. Patients with adverse outcome 90 days after surgery had significantly lower tricuspid lateral annular motion, increased prevalence of RV dysfunction (⬎moderate, qualitatively estimated), suggesting worse RV function. Patients with adverse outcome had increased ELAP, higher prevalence of MDI ⬍2 m/[cm/s]), higher prevalence of inter atrial septum deviated to the right, all suggesting inefficient LV unloading. Of note, patients with worse outcome had increased prevalence of inter ventricular septum deviated to the left. There was no significant difference in the status of aortic valve opening, pump speed (rpm), pump flow (estimated by the controller or echocardiography), or pulse index between the groups. We have evaluated the clinical characteristics, as well as laboratory variables at the time of the echo (30 days after surgery) and presented them in Table 2. The patients with adverse 90-day outcome were clinically worse at 30 days as evidenced by significantly more patients in NYHA III or IV functional class, higher creatinine, higher BUN and a trend for increased NT-BNP. Patients with adverse outcome had lower 6-minute walk distance 3 months after surgery, as expected. Thirty-Day Post-LVAD Echocardiographic Variables Associated With 90-Day Adverse Outcome Individual-predictor analyses for prediction of the 90-day combined outcome (Table 3) revealed no significant associ- Topilsky et al Post-LVAD Echo Variables 653 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Figure 4. A and B, A patient was readmitted for persistent heart failure 30 days after left ventricular assist device (LVAD) surgery. A, Mitral inflow PW interrogation showing a markedly short deceleration time (red arrow), E-wave velocity of 0.86 m/s (yellow arrow), and a very steep slope of mitral valve deceleration index (MDI) calculated as 1.37 ms/[cm/s] (white arrow). The pump’s speed was increased by 400 rpm. C, M-mode examination of the aortic valve shows that the aortic valve is now permanently closed. D, Mitral inflow PW interrogation showing prolongation of the deceleration time (red arrow), E-wave velocity of 0.79 m/s (yellow arrow), and a milder slope of MDI calculated as 2.17 ms/[cm/s] (white arrow). The patient’s symptoms improved considerably, and NT-BNP decreased a few days after the change in rpm. ation with the compound outcome measure for the variables related to the valvular function, left ventricle function or size or pump flows, and output. The only variables assessing RV function that were significantly associated with worse 90-day outcome were a lower tricuspid lateral annulus velocity and an interventricular septum deviated to the left, suggesting that the RV flow is not rapid enough to fill the left ventricle. We have recently shown that the most significant predictor of outcome using the pre LVAD echocardiographic examination was the decreased timing interval between the cessation and the onset of TRDc.17 Surprisingly, TRDc measured 30 days after LVAD implantation was not associated with adverse outcome (P⫽0.8). Patients with NYHA class III/IV at 30 days were more likely to have adverse 90-day outcome, with a RR of 12.0 (4.1–39.9; P⬍0.0001).We have analyzed whether NT-BNP (evaluated 30 days after LVAD implantation) is associated with the adverse outcome at 90 days. We found that 30 day NT-BNP is associated with increased risk for adverse outcome at the 90-day period by a risk ratio of 1.18 (0.98 –1.56) for every increase in NT-BNP by 1 ng/mL, with marginal statistical significance (P⫽0.08). When we log-transformed the 1-month NT-BNP data it became nonsignificant as a predictor of outcome (P⫽0.3). The decrease (%) in NT-BNP from baseline (before LVAD) to 30 days after LVAD implantation was significantly associated with the 90-day adverse outcome (RR, 0.6 [0.21– 0.96]; P⫽0.02 for 1% change). When we log transformed the NT-BNP change from baseline to one month it became nonsignificant as a predictor of outcome as well (P⫽0.6) (Table 3). Most of the variables suggesting non efficient LV unloading were associated with worse outcome. These included MDI ⬍2 m/[cm/s], higher ELAP (using the multistep process described in the methods section) and an atrial septum deviated to the right. To analyze the significance of ELAP, deceleration time and MDI we compared them to the wedge pressure in 8 patients in which the echocardiographic and hemodynamic evaluation were performed simultaneously. The ELAP was positively and significantly correlated to the wedge pressure (r⫽0.74; P⫽0.03). Both deceleration time (r⫽⫺0.69; P⫽0.056) and MDI (r⫽⫺0.72; P⫽0.04) were negatively correlated to the wedge pressure but the correlation was better when the deceleration time was corrected for the E-wave velocity. Intraobserver and Interobserver Variability Comparison of intraobserver timing intervals showed good agreement between measurements: estimated LA pressure (mean difference, ⫺1.0⫾3.1 mm Hg; r⫽0.93; P⫽0.34), Deceleration time (mean difference, 5.0⫾12.9 ms; r⫽0.96; P⫽0.25), and MDI (mean difference, 0.04⫾0.25 ms/[cm/s]; r⫽0.98; P⫽0.62). The Bland-Altman plot showed a random scatter of points around 0, indicating no systematic bias or measurement error proportional to the measurement value. Measurement variability (within-subject coefficient of variation and 95% confidence interval of the Bland-Altman method) for measurements for intraobserver differences was as follows: estimated LA pressure 27.4% and ⫾1.0 mm Hg, Deceleration time 7.1% and ⫾4.1 ms and MDI 9.4% and ⫾0.08 ms/[cm/s] Comparison of interobserver timing intervals showed good agreement as well: estimated LA pressure (mean difference, ⫺0.1⫾3.2 mm Hg; r⫽0.88; P⫽0.92), deceleration time (mean difference, 4.9⫾12.2 ms; r⫽0.97; P⫽0.24), and MDI (mean difference, ⫺0.02⫾0.25 ms/[cm/s]; r⫽0.98; P⫽0.84). The Bland-Altman plot showed a random scatter of points around 0, indicating no systematic bias or measurement error proportional to the measurement value. Measurement variability (within-subject coefficient of variation and 95% confidence interval of the Bland-Altman method) for measurements for interobserver differences was as follows: estimated LA pressure, 26.6% and ⫾3.2 mm Hg; deceleration time, 6.7% and ⫾12.2 ms; and MDI, 9.6% and ⫾0.25 ms/[cm/s]. 654 Circ Cardiovasc Imaging November 2011 Table 1. Baseline Characteristics (Before LVAD Implant) for Patients Divided Into Groups With and Without Adverse 90-Day Outcome (Mortality, Hospitalization for Heart Failure, NYHA Class III or Higher) Characteristic Age, y Sex, male, % Race, % No Adverse Outcome (n⫽46) 61.9⫾14 Adverse 90-Day Outcome (n⫽30) 63.9⫾11 P Value 0.5 Continued No Adverse Outcome (n⫽46) Adverse 90-Day Outcome (n⫽30) P Value VO2 max, mL/kg per min㛳 10.3⫾2.5 10.0⫾3.2 0.7 Left ventricular diastolic diameter, mm* 69.3⫾8 64.8⫾11 0.06 63.2⫾7 58.2⫾11 0.05 Characteristic 75 90 0.3 Left ventricular systolic diameter, mm* Caucasian, 96 Caucasian, 94 0.4 Ejection fraction, %* 18.8⫾7 22.7⫾11 0.1 African American, 2 African American, 3 Left atrial volume index, mL/m2* 65.7⫾28 67.2⫾18 0.8 E/e⬘ ratio* 0.9 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Asian, 2 Asian, 0 Native American, 0 Native American, 3 Hypertension, % 37 40 0.9 Diabetes, % 20 37 0.1 Chronic renal failure, % 44 63 0.1 Atrial fibrillation, % 15 20 0.6 AICD 44 37 0.4 Weight, kg Table 1. 26.5⫾12 26.3⫾10 Tricuspid regurgitation velocity, m/s* 3.1⫾0.6 2.8⫾0.6 0.05 Tricuspid valve lateral annulus velocity, m/s* 0.08⫾0.03 0.08⫾0.03 0.3 63 76 0.2 Right ventricle dysfunction ⬎MO*§ TRDc, ms 482⫾66 446⫾72 0.04 RIMP* 0.61⫾0.25 0.52⫾0.24 0.2 Mean right atrial pressure, mm Hg* 14.4⫾5 16.3⫾8 0.3 36.6⫾10 34.5⫾8 0.3 83.7⫾19 88.2⫾21 0.4 2.0⫾0.2 2.0⫾0.2 0.6 NYHA class IV, % 44 76 0.02 Prior sternotomy, % 42 50 0.7 Mean pulmonary pressure, mm Hg* Preoperative IABP, % 25 40 0.2 PVR, Woods Units‡ 4.6⫾3 3.8⫾3 0.3 Preoperative inotropic use 60 69 0.5 RV dP/dt*‡ 502⫾208 440⫾180 0.2 0 3 0.2 Mean Wedge pressure, mm Hg*‡ 23.1⫾6 22.9⫾6 0.9 BSA Preoperative mechanical ventilation Destination therapy, % 56 70 0.4 Cardiac output, L/min*‡ 3.7⫾1 4.1⫾1 0.1 Type of cardiomyopathy I (56); R (5) I (43); R (20) 0.2 2.0⫾0.6 0.2 D (37) Cardiac index, L/min/m2*‡ 1.9⫾0.5 D (39) Heart rate, beats per minute 75.5⫾15 75.5⫾13 0.9 Systolic blood pressure, mm Hg 98.3⫾11 98.3⫾17 0.9 Diastolic blood pressure, mm Hg 66.8⫾10 62.5⫾10 0.1 Hemoglobin† 12.5⫾2 11.4⫾12 0.02 Bilirubin† 1.23⫾0.6 1.12⫾0.8 0.5 AST 59⫾90 81⫾231 0.6 ALT 88⫾204 71⫾197 0.7 LVAD indicates left ventricular assist device; NYHA, New York Heart Association; AICD, automatic implantable cardioverter-defibrillator; AST, aspartate aminotransferase; ALT, alanine aminotransferase; BUN, blood urea nitrogen; PT INR, prothrombin international normalized ratio; NT-BNP, N-terminal pro-B-type naturetic peptide; ACE inhibitors, angiotensin-converting enzyme inhibitors; BB, beta-blocker; BSA, body surface area; IABP, intra-aortic balloon pump; I, ischemic; D, dilated; R, restrictive; MDI, mitral deceleration index; TRDc, tricuspid regurgitation time corrected for heart rate; RIMP, right index of myocardial performance; and PVR, pulmonary vascular resistance. *Last echocardiographic measurement before LVAD implantation. †Variables measured or calculated before LVAD implantation. ‡Last hemodynamic study before transplant. §Right ventricle dysfunction greater than moderate by the qualitative assessment. 㛳VO2 max measured in 10 patients in the adverse outcome group and 30 patients in the no adverse outcome group; 6-minute walk assessed in 6 patients in the adverse outcome group and 15 patients in the no adverse outcome group. BUN† 28⫾13 30⫾14 0.6 Creatinine† 1.5⫾0.8 1.6⫾0.6 0.5 PT INR 1.4⫾0.4 1.4⫾0.4 0.9 6567⫾6123 5652⫾6035 0.6 Log NT-BNP 8.4⫾0.9 8.1⫾1.1 0.4 Lietz-Miller score† 7.8⫾4 8.4⫾7 0.6 NT-BNP† ACE inhibitors 58 53 0.3 BB 77 88 0.9 Aldospirone, % 43 47 0.5 Digoxin 65 40 0.1 Diuretics 88 96 0.3 Statins, % 63 43 0.3 322⫾83 308⫾117 6-Minute walk, m㛳 0.8 (Continued) Long-Term Outcomes Mean follow-up duration after surgery was 321 [186 – 602] days. Eighteen patients (24%) died during follow-up, and 14 patients had their LVAD explanted for heart transplantation during the follow-up period. The causes of deaths in the 14 patients surviving the 90-day period were traumatic head trauma injury in 2, hemorrhagic stroke in 2, unexplained sudden death in 6, RV failure in 1, embolic stroke in 1, complication of myocardial biopsy after transplant in 1, and 1 patient who decided to withdraw support due to Topilsky et al Post-LVAD Echo Variables Table 2. Post-LVAD 30-Day Echocardiographic, LVAD Controller, and Laboratory and Clinical Variables Divided Into Patients With and Without Adverse 90-Day Outcome No Adverse Outcome (n⫽46) Adverse 90-Day Outcome (n⫽30) Left ventricular diastolic diameter, mm* 58.3⫾9 55.0⫾11 0.3 Left ventricular systolic diameter, mm* 50.2⫾10 47.4⫾13 0.4 Ejection fraction, %* 26.0⫾12 25.6⫾13 0.9 Characteristic P Value Native left ventricle and valves AR ⬎trivial* 41 53 0.4 MR ⬎mild* 9 27 0.4 Right ventricle function and size Tricuspid regurgitation velocity, m/s* Tricuspid valve lateral annulus velocity, m/s* Right ventricle dysfunction ⬎MO*§ 2.5⫾0.4 2.4⫾0.5 0.3 0.09⫾0.03 0.07⫾0.02 0.01 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 11 46 0.03 RVEDA, cm2* 28.8⫾7 29.2⫾7 0.8 RVESA, cm2* 18.1⫾5 19.8⫾6 0.3 RV FAC, %* 38.0⫾10 32.6⫾13 0.09 TRDc, ms 412⫾60 389⫾55 0.3 RIMP 0.28⫾0.12 0.34⫾0.2 0.2 TV annulus diameter* 3.2⫾0.4 3.3⫾0.5 0.7 TR vena contracta* 3.6⫾2.4 4.4⫾2.5 0.3 E-wave velocity* 0.72⫾0.1 0.79⫾0.18 0.2 E/e⬘ ratio* 14.5⫾4 22.8⫾13 0.3 0 (29); I (12); C (59) 0 (18); I (11); C (71) 0.5 R (3); N (71); L (26) R (24); N (51); L (25) 0.01 LV unloading Aortic valve status, %* Atrial septal position, %* Atrial septal position to right, %* Ventricular septal position, %* Ventricular septal position to left, %* 3 R (57); N (39); L (4) 4 24 R (43); N (40); L (17) 17 0.07 0.6 Left ventricular diastolic diameter change, %* ⫺15.8⫾11 ⫺13.2⫾19 Left ventricular systolic diameter change, %* ⫺20.5⫾17 ⫺13.7⫾25 Estimated LA pressure* Estimated LA pressure ⬎15 mm Hg, %* Deceleration time* Deceleration time ⬍150* MDI, ms/关cm/s兴* MDI ⬍2 m/关cm/s兴* 0.004 0.2 0.4 7.4⫾4 14.1⫾6 ⬍0.0001 7 55 ⬍0.0001 189⫾51 15 288⫾137 20 170⫾63 42 219⫾121 56 0.3 0.04 0.09 0.01 LVAD flows by echocardiography Total output* 5.6⫾2 5.8⫾2 0.8 LVAD output* 5.3⫾1.3 4.7⫾1.2 0.3 LVAD output index* 2.7⫾0.7 2.4⫾0.6 0.4 Inflow velocity* 77.4⫾41 75.5⫾32 0.8 109.7⫾39 97.3⫾41 0.3 9538⫾221 9542⫾301 0.9 Pump flow† 5.5⫾0.8 5.3⫾0.7 0.5 Pump flow index† 2.6⫾0.4 2.6⫾0.4 0.8 PI† 5.0⫾0.6 4.9⫾0.8 Outflow velocity* Controller pump parameters Pump speed† 0.7 (Continued) 655 656 Circ Cardiovasc Imaging Table 2. November 2011 Continued No Adverse Outcome (n⫽46) Characteristic Adverse 90-Day Outcome (n⫽30) P Value Laboratory and clinical parameters at the day of echo NYHA class NYHA class III/IV, % I (7); II (68) I (0); II (20) III (23); IV (2) III (43); IV (37) 25 80 ⬍0.0001 ⬍0.0001 Heart rate, beats per minute 85.7⫾11 88.7⫾10 0.3 Mean blood pressure, mm Hg 88.7⫾7 87.1⫾11 0.6 Atrial fibrillation, % NT-BNP Log NT-BNP Hemoglobin† Albumin† 11 16.6 0.7 2840⫾1411 3981⫾4188 0.2 7.8⫾0.5 8.0⫾0.7 0.3 10.7⫾2 10.2⫾1 0.2 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 3.5⫾0.7 3.3⫾0.6 0.3 Creatinine† 0.94⫾0.3 1.3⫾0.7 0.02 BUN† 20.1⫾9 27.6⫾16 0.05 Bilirubin† 0.94⫾0.5 2.3⫾6.3 0.3 ACE inhibitors, %† 30 10 0.03 BB, %† 52 20 0.008 Diuretics, %† 83 92 0.3 90-Day postdischarge parameters NYHA‡ NT-BNP‡ 6-Minute walk, m‡ I (36); II (64) I (0); II (4) III (0); IV (0) III (81); IV (15) 1885⫾1509 3125⫾2067 273⫾128 239⫾95 ⬍0.0001 0.05 0.0009 LVAD indicates left ventricular assist device; AR, aortic regurgitation; MR, mitral regurgitation; RVEDA, right ventricle end-diastolic area; RVESA, right ventricle end-systolic area; RV FAC, right ventricle fractional area change; TV, tricuspid valve; O, opening every cycle; I, intermittent opening; C, permanently closed; R, deviated to the right; N, neutral position; L, deviated to the left; LA, left atrium; ELAP, estimated left atrial pressure; MDI, mitral deceleration index; and NYHA, New York Heart Association. *Echocardiographic measurement performed 30 days after LVAD implant. †Variables measured 30 days after LVAD implantation. ‡Variables measured at the end of 90-day period after LVAD implantation. §Right ventricle dysfunction greater than moderate by the qualitative assessment. persistent RV failure and need for dialysis. The actuarial survival rate was 83.2⫾17% and 68.0⫾8% at 1 and 2 years, respectively. There were too few events to permit meaningful analyses of the association between echocardiographic variables and long term outcome. ELAP was significantly but weakly correlated with pump speed (r⫽⫺0.27; P⫽0.02) as well as MDI (r⫽0.24; P⫽0.04) suggesting that increasing the speed may decrease LA pressure and lengthen the mitral deceleration time. Our experience in several different patients corroborates this assumption (Figures 2 and 3). Discussion This study is one of the first to report on echocardiographic variables after LVAD surgery associated with adverse outcome and persistence of heart failure. We found that adverse events in the 90 days after surgery period were associated with evidence of decreased RV contraction (lower tricuspid lateral annulus velocity) and inadequate LV unloading (ELAP, MDI) in the 30-day echocardiographic examination. Deviation of the interventricular septum to the left, which may be related to reduced RV forward flow or over decompression of the LV, was associated with adverse outcomes as well. RV Dysfunction RV dysfunction is very common immediately after LVAD surgery and was shown to contribute to the perioperative mortality,1,3,7 as well as decreased long term survival. We believe that postoperative RV dysfunction is comprised of 2 processes: one of secondary RV dysfunction related to LV failure and the second due to intrinsic RV dysfunction. We do not offer LVAD therapy in patients with primary RV dysfunction such as RV dysplasia. However, we believe that secondary RV dysfunction usually improves with an effective LVAD therapy in the overwhelming majority of patients with LV dysfunction as the primary cause of heart failure. Therefore, we consider LVAD therapy in all patients with end stage heart failure due to primary LV failure regardless of the degree of RV dysfunction. The only variables we found to be related to RV function in the echocardiographic examination Topilsky et al Table 3. Individual-Variable Analyses of Mid Term Compound 90-Day Adverse Event in Patients Undergoing LVAD Implantation Table 3. OR (95% CI) Variable Left ventricular diastolic diameter, mm 0.96 (0.89 –1.03) Left ventricular systolic diameter, mm 0.97 (0.92–1.03) MR Mi/No: 0.48 (0.15–1.6) P Value 0.3 0.4 0.5 Mo/Mi: 2.0 (0.20–23.5) AR Mi/No: 2.4 (0.48–15.4) 0.3 TR vena contracta 1.14 (0.91–1.44) 0.2 Tricuspid regurgitation velocity, m/s 0.46 (0.12–1.62) 0.2 0.7 (9.48–0.95) 0.02 Tricuspid lateral annulus velocity, m/s Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Right ventricle dysfunction ⬎moderate RIMP, 0.1 increase 1.07 (0.57–2.0) 0.8 1.3 (0.89–1.96) 0.2 RVEDA, cm2 1.01 (0.93–1.09) 0.8 RVESA, cm2 1.05 (0.96–1.16) 0.3 RV FAC, % 0.96 (0.91–1.00) 0.07 Total output 1.07 (0.65–1.8) 0.8 LVAD output 0.67 (0.31–1.3) 0.2 LVAD output index 0.56 (0.14–1.95) 0.4 Inflow velocity 0.99 (0.98–1.01) 0.8 Outflow velocity 0.99 (0.98–1.01) 0.3 E/e⬘ ratio 1.15 (0.95–1.68) 0.2 Deceleration time 0.99 (0.98–1.0) 0.3 Deceleration time ⬍150 ms 2.04 (1.04–4.3) 0.04 MDI 0.99 (0.98–1.00) 0.07 MDI ⬍2 ms/关cm/s兴 4.4 (1.22–18.0) 0.02 ELAP 1.3 (1.16–1.48) ⬍0.0001 ELAP ⬎15 mm Hg Atrial septal position 15.6 (4.4–73.7) ⬍0.0001 N/R: 0.18 (0.02–0.89) 0.07 L/N: 2.02 (0.69–6.05) Atrial septal position to the right Ventricular septal position 2.1 (1.02–5.6) 0.05 N/R: 2.25 (0.86–6.0) 0.01 L/N: 5.9 (1.12–119.1) Ventricular septal position to the left Aortic valve status 3.03 (1.21–13.3) 0.01 I/O: 1.09 (0.17–6.2) 0.7 C/I: 1.46 (0.32–7.8) 657 Continued NT-BNP, 100 pg/mL Variable Post-LVAD Echo Variables Log NT-BNP OR (95% CI) P Value 1.18 (0.98 –1.56) 0.08 1.5 (0.71–3.6) 0.3 NT-BNP change, % 0.6 (0.21–0.96) 0.02 Log NT-BNP change 0.8 (0.4–1.6) 0.6 NYHA class III or IV 12.0 (4.1–39.9) ⬍0.0001 LVAD indicates left ventricular assist device; OR, odds ratio; CI, confidence interval; AR, aortic regurgitation; MR, mitral regurgitation; RVEDA, right ventricle end-diastolic area; RVESA, right ventricle end-systolic area; RV FAC, right ventricle fractional area change; TV, tricuspid valve; O, opening every cycle; I, intermittent opening; C, permanently closed; R, deviated to the right; N, neutral position; L, deviated to the left; LA, left atrium; ELAP, estimated left atrial pressure; MDI, mitral deceleration index; and NYHA, New York Heart Association. performed 30 days after LVAD implantation associated with the 90-day adverse outcome were decreased tissue Doppler tricuspid valve lateral velocity and a interventricular septum deviated to the left. This is in marked discordance with the echocardiographic variables before LVAD surgery in which the main variable associated with outcome was the TR duration corrected for heart rate (TRDc). TRDc is related to the pressure difference in mean systolic right ventricular pressure and mean right atrial pressure.17 In other words, it describes hemodynamic interactions between the pulmonary vasculature (pulmonary hypertension), venous system (right atrial pressure) and right ventricular contractility. Once an LVAD is in place, left ventricular end-diastolic pressure, and secondary pulmonary hypertension usually improve considerably21 and TRDc is no longer predictive of outcome. On the other hand, the tissue Doppler tricuspid valve lateral velocity is a sensitive measure of right ventricular contraction. In patients with severe LV dysfunction before LVAD implantation, it was markedly reduced in all patients due to the excessive after load imposed on the RV and could not discriminate between patients with reversible/secondary or irreversible/primary RV damage. After LVAD implantation, tissue Doppler tricuspid valve lateral velocity increased considerably in the patients in which RV dysfunction was secondary to the increased after load imposed by the failing LV but did not improve in patients who had irreversible RV damage, making it a sensitive indicator of RV reserve after LVAD. LV Unloading Left ventricular diastolic diameter change, % 1.00 (0.96–1.06) 0.7 Left ventricular systolic diameter change, % 1.00 (0.98–1.04) 0.5 Because LVAD therapy is supposed to increase cardiac output and unload the left-sided chambers, we postulated that variables estimating the cardiac output and the efficiency of left ventricular or left atrial decompression may be predictive of failure to improve heart failure. Hemoglobin 0.77 (0.55–1.01) 0.06 Aortic Valve Opening Status Bilirubin 1.09 (0.93–1.69) 0.3 Albumin 0.18 (0.03–0.61) 0.003 3.4 (0.84–19.2) 0.03 In a patient on LVAD support, the total forward blood flow in the ascending aorta is the sum of contributions from both LVAD and the LV. In the setting of a high LVAD pump speed, the flow contribution by the native LV would be minimal, the LV would not be able to generate any stroke volume, and the entire forward flow would be from the LVAD. On the other hand, if the LVAD pump speed settings Laboratory and clinical parameters at the day of echo Creatinine BUN 1.04 (1.01–1.1) Platelets 0.99 (0.98–0.99) 0.04 0.04 (Continued) 658 Circ Cardiovasc Imaging November 2011 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 are low, the native LV generates a stroke volume by opening of the native aortic valve which contributes to the overall forward flow. Thus, we expected the status of aortic valve opening to reflect the efficiency of LV unloading and to be associated with outcome. Our analysis did not prove the “aortic valve opening status” to be significantly associated with the 90-day outcome. The status and rate of aortic valve opening depends on the relation between LV intracavitary pressure and aortic pressure during systole. In patients with very poor LV contractility, the aortic valve may not open despite inefficient LV unloading and high LV filling pressure (Figure 2). On the other hand, when LV function recovers the aortic valve may open with each cardiac contraction even if the LV is unloaded because the LV effectively competes with the LVAD. Therefore, the degree of aortic opening is influenced by the complex interaction between the native heart and the LVAD in each patient. The lack of statistical significance for “aortic valve opening status” does not suggest that it is not useful. Aortic valve opening may be an important variable as it is a surrogate marker of preserved pulse pressure, but it is important to note that there is still no data that indicates that short or long-term outcomes are best with intermittent AV opening. We believe that when setting LVAD rpm, we should aim for 3 objectives: adequate cardiac output, ameliorate congestion, and maximize pulse pressure. Of course, it would be ideal to emulate nature as much as possible, that is, produce near normal pulse pressure. Therefore, we aim to minimize LVAD pump speed to increase pulse pressure as much as possible as long as we do not compromise the first 2 objectives for the third. Estimated LA Pressure It has been previously shown that because the IAS is a thin membranous structure between the left and right atria, its configuration is altered by the interatrial pressure gradient in normal patients, as well as in patients with mitral stenosis, mitral regurgitation, and tricuspid regurgitation.28,29,38 In normal subjects, the IAS protrudes slightly toward the right atrium in end-systole. However, it flattens or retracts slightly toward the left atrium in end-diastole. These changes in IAS position corresponded to a left-to-right pressure gradient of 3–5 mm Hg during the peak of the “v” point with a transient reversal of the left-to-right gradient during atrial contraction observed in normal patients.30 Based on these observations, suggesting that a change in inter atrial pressure gradient of less than 5 mm Hg shifts the inter atrial septum either to the left or to the right we have arbitrarily estimated the mean LA pressure as LA pressure⫽RA pressure if inter atrial septum was neutral, LA⫽RA pressure⫺5 mm Hg if interatrial position was deviated to the left, and LA pressure⫽RA pressure⫹5 mm Hg if interatrial position was deviated to the right. Because estimation of RA pressure using the inferior vena cava diameter and its response to inspiration has been previously validated,24,39,40 we hypothesized that combining the estimated RA pressure and the position of the interatrial septum may prove valuable in estimating the efficiency of LA and LV unloading and LVAD function. To try to validate our approach to assess left atrial pressure we compared the estimated left atrial pressure by echocardiography (ELAP) to the wedge pressure in 8 patients in which an invasive right heart catheterization was performed simultaneously with the echocardiographic examination. The correlation was significant (r⫽0.74; P⫽0.03), suggesting that the ELAP may be considered a reasonable surrogate (although not perfect estimation) for wedge pressure. A higher estimated LA pressure (ELAP), especially above a cutoff of 15 mm Hg was found to be associated with increased risk for early adverse outcome. We believe that elevated LA pressure may reflect inefficient LV unloading, and worse RV function (as it is influenced by RA pressure as well), or the combination of both, making it a useful parameter for estimating proper LVAD function. Furthermore, it may be changed using manipulation of the pump’s speed (Figure 3), making it an attractive parameter to use during “ramp/optimization” studies. In simple words, if a patient has an estimated RA pressure ⱖ15 mm Hg (estimated by the inferior vena cava diameter and its response to inspiration) the clinician may consider increasing the pump speed to the point the interatrial position assumes a leftward or at least neutral position. Mitral Deceleration Index There is an inverse relation between the mitral inflow deceleration time and the LV end-diastolic pressure.31,32 For any given rate of deceleration of early mitral inflow, a higher E-wave velocity (E) is associated with a longer deceleration time. In patients with LVADs, E-wave velocity will represent the complex interaction between the left atrial pressure in early diastole and the negative pressure created by the LVAD in the left ventricle. We postulated that deceleration time normalized for E-velocity will better predict cardiovascular (CV) events compared with deceleration time or E-velocity alone, as been previously shown in patients with hypertrophic cardiomyopathy and/or hypertension.33,34 MDI is inversely related to the deceleration slope and positively related to the pressure half-time.33,34 Just as in patients with mitral stenosis, a long MDI suggests slower increase in left ventricular pressure and slower pressure equilibration between left atrium and left ventricle. In patients with mitral stenosis the slow increase in ventricular pressure is related to the obstruction to inflow, but in patients with an LVAD, it is due to the increased rate of clearance of blood out of the left ventricle. To try to validate the association between the mitral inflow deceleration time, or MDI and LV end-diastolic pressure, we compared these parameters to the wedge pressure (which in patients with no mitral stenosis can be considered a good surrogate for LV end-diastolic pressure) in 8 patients in which an invasive right heart catheterization was performed simultaneously with the echocardiographic examination. We found that both the mitral inflow deceleration time, and MDI were negatively correlated to the wedge pressure, but the correlation was better for the MDI. These results suggest that the MDI is a reasonable surrogate for LV end diastolic pressure. A short MDI ⬍2 ms/[cm/s] was found to be associated with early adverse outcome. We believe that a short MDI reflects rapid rise in LV diastolic pressure, equilibrating early with LA pressure reflecting inefficient clearance of blood by Topilsky et al the LVAD. The mitral deceleration index was related to pump speed and could be increased with increasing pump speed, suggesting it can be another parameter to use during “ramp/ optimization” studies (Figure 3), especially in patients in which the aortic valve is already closed but still have clinical or hemodynamic evidence of insufficient LV decompression. In other words, if a patient has MDI ⬍2 ms/[cm/s] and symptoms of pulmonary congestion, an increase in pump speed until the MDI is ⬎2 ms/[cm/s] may improve outcomes. Interventricular Septal Position Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 The interventricular septum is muscular and stiffer than the interatrial septum and thus needs higher interventricular gradient to be shifted to the right or to the left. In patients with an LVAD, an increase in pump speed up to the point that the left ventricular pressure is so low that it results in leftward shift of the ventricular septum, may represent a right ventricle that cannot generate enough flow to “fill” the left ventricle at the same rate as the flow created by the LVAD. The shift in the interventricular position may impair RV output by itself, diminishing the left ventricular cavity even further. This worsening spiral may cause the septum to encroach on the inflow cannula resulting in ventricular arrhythmias or drastically decreasing LVAD preload. Furthermore, this shift may also induce tricuspid regurgitation, resulting in systemic congestion and lower forward output.20 Of note, this is in marked discordance with the interatrial septum, which can be shifted to the left with smaller transatrial pressure gradients, which may be of use when right atrial pressure is ⬎15 mm Hg. We believe that LVAD unloading to the extent of interventricular septum shift to the left, resulting in severe TR or potential RV dysfunction should be avoided, but, fortunately, this occurs infrequently. In some of these patients, hemodynamic guidance with right heart catheterization to optimize cardiac output and LA pressure during speed adjustment may be helpful. Echocardiographic Evaluation of LVAD Performance and Optimization Studies The present study is a retrospective analysis of the echocardiographic variables obtained at 1 month after LVAD implantation. LVAD settings during those echocardiographic exams were not changed between discharge and the 1-month evaluation. We did not perform optimization studies using the newer variables (deceleration time, MDI, and ELAP) at the time of our primary analysis. The concept of “optimization” of LVAD settings, based on echocardiographic appearance has only been formulated recently, and thus we are unable to answer the questions of whether optimization is associated with best short term or long-term outcomes. Nevertheless, we find it intriguing that adverse outcomes were associated with echocardiographic variables suggestive of poor LV unloading or RV failure at 1 month. Based on these findings, our present routine is to perform “optimization” echocardiographic studies in every patient that presents with heart failure symptoms (NYHA class III or higher) during follow-up. Because LAVD is placed to address low cardiac output and LV congestion, we believe that speed setting should be set to address both of these issues. At the Post-LVAD Echo Variables 659 first step in LVAD optimization we assess RV cardiac output (which is the total cardiac output), or LVAD output, as described in the Methods section. LVAD speed setting should be altered to optimize cardiac output to be compatible with life (we use a cutoff of cardiac index ⬎2.2 L/min/m2). In some, it may be beyond what we could achieve by LVAD setting adjustment due to severe intrinsic RV failure, but these patients are rare and usually have uncontrollable RV dysfunction or are in need of an RV assist device. In the second step, we believe echo should help to set LVAD rpm to improve LV filling pressures by assessing mitral valve inflow deceleration time, MDI, or by judging RA pressure and LA pressure by using the inferior vena cava method and the interatrial septal position, respectively. As to the “aortic valve opening status,” it was not found to be a significant predictor of short-term outcome. The lack of statistical significance for “aortic valve opening status” does not suggest that it is not useful because it may be a surrogate marker of preserved pulse pressure. We believe that it would be ideal to preserve near normal pulse pressure, although there is no data that indicates that long-term outcomes are best with intermittent AV opening. On the other hand, we should not compromise the first 2 objectives (cardiac output and LV unloading) for the third. We also believe that LVAD unloading to the extent of interventricular septum shift to the left, resulting in severe TR or potential RV dysfunction should be avoided. In some of these patients, if intermittent AV opening, or neutral interventricular position cannot be achieved without elevated ELAP or shortened MDI, hemodynamic guidance with right heart catheterization to optimize cardiac output and LA pressure during speed adjustment may be helpful. It is important to note that the present study was not aimed to find one “perfect” echo variable to predict failure or success, and we do not believe such a variable exists. For evaluating or optimizing LVAD performance a multifaceted approach is essential. We should estimate the 3 goals of optimal LVAD therapy: improved cardiac output, LV unloading and preserved pulsatility. The availability of different variables assessing these 3 objectives of LVAD function (total cardiac output, LVAD output, aortic valve status, LV diameter, interventricular position, MDI, ELAP) provides an internal verification and corroboration of LVAD function, particularly when technical or physiological conditions preclude the use of one or the other of these indexes. The interpreter must integrate the different variables and disregard “outlying” data, making the best estimate of LVAD function. Finally, the echocardiographic and Doppler data are best interpreted within the clinical context at the time of the examination. The different variables (aortic valve status, MDI, ELAP) may be influenced by LVAD speed, and hemodynamic conditions such as blood pressure, fluid status, or inotropic use. Therefore, it is essential to record the pump’s rpm and patient’s blood pressure at the time of the study and note the patient’s medications whenever possible. LV Recovery Dandel et al41 have previously reported echo variables that were useful in predicting successful recovery, which were mostly related to LV geometry and systolic function (LV 660 Circ Cardiovasc Imaging November 2011 Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 diameter and ejection fraction) rather than echo hemodynamics. Their study was very different from our study in many aspects. First, they aimed for echocardiographic predictors of LV recovery, which is rare and would likely require a totally different approach than support intended for a lifetime as in our cohort. Second, they used “off-pump” echocardiographic examinations as opposed to our exams, which were performed on full LVAD support. Third, their study involved mostly pulsatile LVADs, whereas ours was restricted to evaluation of continuous-flow LVADs alone. Nonetheless, ability to assess myocardial recovery during LVAD support would be enormously helpful. An important provision is that both LV preload and after load need to be consistent to be able to compare LV recovery variables over time. We hypothesize that if we could estimate LV end diastolic pressure, using MDI or deceleration time, concurrent with assessment of variables of LV contractility as LV ejection fraction, these would be reasonable variables to screen for myocardial recovery. Conclusion Mortality and persistent heart failure after LVAD surgery appear to be predominantly determined by inefficient unloading of left chambers and persistent RV dysfunction. Increased ELAP, MDI ⬍2 ms/[cm/s], and the degree of RV dysfunction, reflected by decreased tissue Doppler tricuspid lateral annulus velocity, or an interventricular septum deviated to the left are all associated with worse mid-term outcome. An appropriate combination of flow, unloading and pulse pressure is yet to be determined for the best long-term outcome. Our study was not designed to establish the causeand-effect relationship between “optimizing” LVAD variables and better clinical outcome, but it seems to suggest that such a concept should be explored further in a larger prospective study using serial changes in echo variables during long-term support. Study Limitations At the present time, we lack conclusive hemodynamic evidence proving our approach to assess left atrial pressure, which will need validation in prospective studies using simultaneous hemodynamic and echocardiographic studies. Because of the relatively small number of patients and events we lacked the statistical power to predict long-term outcome or to show associations between echo variables and individual end points (mortality, heart failure admissions) and thus were forced to use a combined end point. Furthermore, the same limitation may have resulted in that some potentially important associations (aortic valve opening status, LVAD output) did not reach significance. Results of the present study were based on a retrospective, observational analysis that precluded us from defining the cause and effect relationship between “optimizing” LVAD parameters and better clinical outcome. Given the exploratory nature of the results and the relatively limited number of patients validation in larger patient samples will be required. There is selection bias in that patients who died earlier than 30 days were omitted. Patients who died had significantly lower LVAD output than the survivors (4.6⫾0.5 L/min versus 5.2⫾0.6 L/min; P⫽0.05), which may have resulted in the non significant impact of calculated LVAD flow on outcome. Acknowledgments We thank Zhou Li for her help with statistical analyses. Disclosures None. References 1. Frazier OH, Rose EA, Oz MC, Dembitsky W, McCarthy P, Radovancevic B, Poirier VL, Dasse KA. Multicenter clinical evaluation of the HeartMate vented electric left ventricular assist system in patients awaiting heart transplantation. J Thorac Cardiovasc Surg. 2001;122: 1186 –1195. 2. Frazier OH, Rose EA, Oz MC, Dembitsky WP, McCarthy PM, Radovancevic B, Poirier VL, Dasse KA. Multicenter clinical evaluation of the Heartmate; vented electric left ventricular assist system in patients awaiting heart transplantation. J Heart Lung Transplant. 2001;20: 201–202. 3. Park SJ, Tector A, Piccioni W, Raines E, Gelijns A, Moskowitz A, Rose E, Holman W, Furukawa S, Frazier OH, Dembitsky W. Left ventricular assist devices as destination therapy: a new look at survival. J Thorac Cardiovasc Surg. 2005;129:9 –17. 4. Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, Long JW, Ascheim DD, Tierney AR, Levitan RG, Watson JT, Meier P, Ronan NS, Shapiro PA, Lazar RM, Miller LW, Gupta L, Frazier OH, Desvigne-Nickens P, Oz MC, Poirier VL. Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med. 2001; 345:1435–1443. 5. Miller LW, Pagani FD, Russell SD, John R, Boyle AJ, Aaronson KD, Conte JV, Naka Y, Mancini D, Delgado RM, MacGillivray TE, Farrar DJ, Frazier OH. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357:885– 896. 6. Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, Sun B, Tatooles AJ, Delgado RM III, Long JW, Wozniak TC, Ghumman W, Farrar DJ, Frazier OH. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361: 2241–2251. 7. Horton SC, Khodaverdian R, Chatelain P, McIntosh ML, Horne BD, Muhlestein JB, Long JW. Left ventricular assist device malfunction: an approach to diagnosis by echocardiography. J Am Coll Cardiol. 2005;45: 1435–1440. 8. Scalia GM, McCarthy PM, Savage RM, Smedira NG, Thomas JD. Clinical utility of echocardiography in the management of implantable ventricular assist devices. J Am Soc Echocardiogr. 2000;13:754 –763. 9. Catena E, Milazzo F, Merli M, Paino R, Garatti A, Colombo T, Vitali E. Echocardiographic evaluation of patients receiving a new left ventricular assist device: the Impella recover 100. Eur J Echocardiogr. 2004;5: 430 – 437. 10. Lam KM, Ennis S, O’Driscoll G, Solis JM, Macgillivray T, Picard MH. Observations from non-invasive measures of right heart hemodynamics in left ventricular assist device patients. J Am Soc Echocardiogr. 2009;22: 1055–1062. 11. Chumnanvej S, Wood MJ, MacGillivray TE, Melo MF. Perioperative echocardiographic examination for ventricular assist device implantation. Anesth Analg. 2007;105:583– 601. 12. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440 –1463. 13. Quinones MA, Waggoner AD, Reduto LA, Nelson JG, Young JB, Winters WL Jr, Ribeiro LG, Miller RR. A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 1981;64:744 –753. 14. Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450 – 458. Topilsky et al Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 15. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. Recommendations for evaluation of the severity of native valvular regurgitation with twodimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16:777– 802. 16. Hammarstrom E, Wranne B, Pinto FJ, Puryear J, Popp RL. Tricuspid annular motion. J Am Soc Echocardiogr. 1991;4:131–139. 17. Topilsky Y, Oh JK, Shah DK, Boilson BA, Schirger JA, Kushwaha SS, Pereira NL, Park SJ. Echocardiographic predictors of adverse outcomes after continuous left ventricular assist device implantation. J Am Coll Cardiol Cardiovascular imaging. 2011;4:211–222. 18. Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, Tajik AJ, Seward SB. Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr. 1996;9:838 – 847. 19. Tei C, Dujardin KS, Hodge DO, Kyle RA, Tajik AJ, Seward JB. Doppler index combining systolic and diastolic myocardial performance: clinical value in cardiac amyloidosis. J Am Coll Cardiol. 1996;28:658 – 664. 20. Topilsky Y, Maltais S, Oh JK, Atchison FW, Perrault LP, Carrier M, Park SJ. Focused review on transthoracic echocardiographic assessment of patients with continuous axial left ventricular assist devices. Cardiol Res Pract. 2011;2011:1–11. 21. Topilsky Y, Oh JK, Atchison FW, Shah DK, Bichara VM, Schirger JA, Kushwaha SS, Pereira NL, Park SJ. Echocardiographic findings in stable outpatients with properly functioning HeartMate II left ventricular assist devices. J Am Soc Echocardiogr. 2011;24:157–169. 22. Estep JD, Stainback RF, Little SH, Torre G, Zoghbi WA. The role of echocardiography and other imaging modalities in patients with left ventricular assist devices. J Am Coll Cardiol Cardiovasc Imaging. 2010; 3:1049 –1064. 23. Schwarz KQ, Parikh SS, Chen X, Farrar DJ, Steinmetz S, Ramamurthi S, Hallinan W, Massey HT, Chen L. Non-invasive flow measurement of a rotary pump ventricular assist device using quantitative contrast echocardiography. J Am Soc Echocardiogr. 2010;23:324 –329. 24. Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493– 496. 25. Myers TJ, Frazier OH, Mesina HS, Radovancevic B, Gregoric ID. Hemodynamics and patient safety during pump-off studies of an axial-flow left ventricular assist device. J Heart Lung Transplant. 2006;25:379 –383. 26. Slaughter MS, Pagani FD, Rogers JG, Miller LW, Sun B, Russell SD, Starling RC, Chen L, Boyle AJ, Chillcott S, Adamson RM, Blood MS, Camacho MT, Idrissi KA, Petty M, Sobieski M, Wright S, Myers TJ, Farrar DJ. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant. 2010;29: S1–S39. 27. John R, Kamdar F, Liao K, Colvin-Adams M, Miller L, Joyce L, Boyle A. Low thromboembolic risk for patients with the Heartmate II left ventricular assist device. J Thorac Cardiovasc Surg. 2008;136: 1318 –1323. 28. Tei C, Tanaka H, Kashima T, Yoshimura H, Minagoe S, Kanehisa T. Real-time cross-sectional echocardiographic evaluation of the interatrial 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. Post-LVAD Echo Variables 661 septum by right atrium-interatrial septum-left atrium direction of ultrasound beam. Circulation. 1979;60:539 –546. Tei C, Tanaka H, Nakao S, Yoshimura H, Minagoe S, Kashima T, Kanehisa T. Motion of the interatrial septum in acute mitral regurgitation: clinical and experimental echocardiographic studies. Circulation. 1980; 62:1080 –1088. Braunwald E, Fishman AP, Cournand A. Time relationship of dynamic events in the cardiac chambers, pulmonary artery and aorta in man. Circulation research. 1956;4:100 –107. Nishimura RA, Abel MD, Hatle LK, Holmes DR Jr, Housmans PR, Ritman EL, Tajik AJ. Significance of Doppler indices of diastolic filling of the left ventricle: comparison with invasive hemodynamics in a canine model. Am Heart J. 1989;118:1248 –1258. Nishimura RA, Abel MD, Hatle LK, Tajik AJ. Relation of pulmonary vein to mitral flow velocities by transesophageal Doppler echocardiography: effect of different loading conditions. Circulation. 1990;81: 1488 –1497. Mishra RK, Galloway JM, Lee ET, Best LG, Russell M, Roman MJ, Devereux RB. The ratio of mitral deceleration time to E-wave velocity and mitral deceleration slope outperform deceleration time alone in predicting cardiovascular outcomes: the Strong Heart Study. J Am Soc Echocardiogr. 2007;20:1300 –1306. Chinali M, Aurigemma GP, de Simone G, Mishra RK, Gerdts E, Wachtell K, Boman K, Dahlof B, Devereux RB. Mitral E wave deceleration time to peak E velocity ratio and cardiovascular outcome in hypertensive patients during antihypertensive treatment (from the LIFE echosubstudy). Am J Cardiol. 2009;104:1098 –1104. Topilsky Y, Pereira NL, Shah DK, Boilson B, Schirger JA, Kushwaha SS, Joyce LD, Park SJ. LVAD Therapy in patients with restrictive and hypertrophic cardiomyopathy. Circ Heart Fail. 2011;4:266 –275. Park SJ, Liao KK, Segurola R, Madhu KP, Miller LW. Management of aortic insufficiency in patients with left ventricular assist devices: a simple coaptation stitch method (Park’s stitch). J Thorac Cardiovasc Surg. 2004;127:264 –266. Lietz K, Long JW, Kfoury AG, Slaughter MS, Silver MA, Milano CA, Rogers JG, Naka Y, Mancini D, Miller LW. Outcomes of left ventricular assist device implantation as destination therapy in the post-REMATCH era: implications for patient selection. Circulation. 2007;116:497–505. Tei C, Tanaka H, Kashima T, Nakao S, Tahara M, Kanehisa T. Echocardiographic analysis of interatrial septal motion. Am J Cardiol. 1979; 44:472– 477. Moreno FL, Hagan AD, Holmen JR, Pryor TA, Strickland RD, Castle CH. Evaluation of size and dynamics of the inferior vena cava as an index of right-sided cardiac function. Am J Cardiol. 1984;53:579 –585. Brennan JM, Blair JE, Goonewardena S, Ronan A, Shah D, Vasaiwala S, Kirkpatrick JN, Spencer KT. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr. 2007;20: 857– 861. Dandel M, Weng Y, Siniawski H, Potapov E, Drews T, Lehmkuhl HB, Knosalla C, Hetzer R. Prediction of cardiac stability after weaning from left ventricular assist devices in patients with idiopathic dilated cardiomyopathy. Circulation. 2008;118:S94 –S105. CLINICAL PERSPECTIVE A successful acute outcome after left ventricular assist device (LVAD) implantation depends on patient selection and the technical difficulty of surgery. However, how we treat our patients and LVAD settings may affect the patient outcome beyond the postsurgical period. In the present study, we retrospectively analyzed various variables in echocardiographic examinations performed 30 days after LVAD implant for their association with a compound end point (90-day mortality, readmission for heart failure, or New York Heart Association class III or higher at the end of the 90-day period). We found that mortality and persistent heart failure after LVAD surgery are predominantly associated with echocardiographic variables assessing the efficiency of unloading of the left ventricle and atrium, and those assessing right ventricular function. The only right ventricular variable significantly associated with adverse outcome was a decreased tissue Doppler velocity of the lateral tricuspid annulus. The variables assessing LV unloading, associated with adverse outcome were a high estimated left atrial pressure (⬎15 mm Hg) and a short mitral inflow deceleration time divided by the E wave velocity (⬍2 ms/[cm/s]). An interventricular septum deviated to the left was associated with worse outcome as well. In conclusion, echocardiographic variables suggestive of efficient but not excessive LV unloading are associated with favorable mid and long-term outcome after LVAD surgery. Echocardiographic Variables After Left Ventricular Assist Device Implantation Associated With Adverse Outcome Yan Topilsky, Tal Hasin, Jae K. Oh, Daniel D. Borgeson, Barry A. Boilson, John A. Schirger, Alfredo L. Clavell, Robert P. Frantz, Rayji Tsutsui, Mingya Liu, Simon Maltais, Sudhir S. Kushwaha, Naveen L. Pereira and Soon J. Park Downloaded from http://circimaging.ahajournals.org/ by guest on May 14, 2017 Circ Cardiovasc Imaging. 2011;4:648-661; originally published online September 21, 2011; doi: 10.1161/CIRCIMAGING.111.965335 Circulation: Cardiovascular Imaging is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2011 American Heart Association, Inc. All rights reserved. Print ISSN: 1941-9651. Online ISSN: 1942-0080 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circimaging.ahajournals.org/content/4/6/648 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation: Cardiovascular Imaging can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation: Cardiovascular Imaging is online at: http://circimaging.ahajournals.org//subscriptions/