* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Simulation of Pulsatile Left Ventricular Assist Device - AMAC-2017
Saturated fat and cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Jatene procedure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
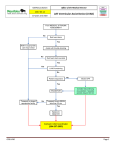
Simulation of Pulsatile Left Ventricular Assist Device Therapy Using Aplysia CardioVascular Lab Elira Maksuti* and Michael Broomé** *Department of Medical Engineering, KTH Royal Institute of Technology, Stockholm, Sweden **ECMO Department, Karolinska University Hospital, Stockholm, Sweden Introduction: Mechanical left ventricular assist devices (LVADs) have been developed for bridging patients to transplantation, but are increasingly being used as destination therapy or temporary aid until recovery. When selecting a pulsatile flow LVAD therapy, the interaction between the mechanical device and the native heart must be taken into account in order to optimize the benefits of the treatment. The aim of this study was to exemplify this complex pathophysiology by assessing the effect of 3 different pulsatile LVAD therapies using Aplysia CardioVascular Lab. Methods: Aplysia software is based on a closed-loop lumped-parameter model consisting of 27 vascular segments, the 4 cardiac chambers, the cardiac valves, the pericardium and intrathoracic pressure [1]. The LVAD were modelled based on the working principle of a commercially available device (Berlin Heart EXCOR, Germany) and was connected between the left ventricle (LV) and the ascending aorta. Heart failure was simulated by reducing the end systolic pressure-volume (PV) relationship of the LV from 2.8 to 0.80 mmHg/mL and increasing the end diastolic PV relationship of the LV from 0.05 to 0.08 mmHg/mL. Three different LVAD therapies were simulated in addition to heart failure: unsynchronized LVAD, LVAD with systolic pulsation and LVAD with diastolic pulsation. Results: All investigated LVAD therapies unloaded the LV and improved cardiac output (Figure 1). LVAD with diastolic pulsation performed better than systolic pulsation since it resulted in lower mechanical load of the LV (total work of 1320 versus 2084 mmHg∙mL, O2 consumption of 3.8 versus 4.8 mL/min) and increased coronary flow (mean flow of 107 versus 95 mL/min), improving LV myocardial oxygen demand and supply balance. Conclusion: Patient specific clinical data together with computer simulation may be a valuable tool in evaluating LVAD treatments. Validation of the simulations results still presents challenges. Figure 1: (a) Simulated pressure-volume loops for a healthy individual in black and for a patient with heart failure in red; heart failure patient coupled to (b) unsyncronized LVAD, (c) LVAD with systolic pulsation and (d) LVAD with diastolic pulsation. Considerations about the “Reuse, Reduce, Recycle” theme of AMAC 2017 Aplysia CardioVascular Lab is a standalone software application with a friendly graphical user interface (GUI). The GUI options can be “basic, standard or advanced” depending on the expertise of the user. Aplysia is commercially available for educational, research and clinical purposes. References [1] M. Broomé, E. Maksuti, A. Bjällmark, B. Frenckner, and B. Janerot-Sjöberg, “Closed-loop real-time simulation model of hemodynamics and oxygen transport in the cardiovascular system.,” Biomed. Eng. Online, vol. 12, no. 1, p. 69, Jan. 2013.