* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Articles in PresS. Am J Physiol Heart Circ Physiol (September 25
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Echocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart failure wikipedia , lookup
Transcript
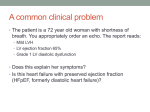
Articles in PresS. Am J Physiol Heart Circ Physiol (September 25, 2015). doi:10.1152/ajpheart.00397.2015 1 2 3 4 5 Afterload-induced diastolic dysfunction contributes to high filing pressures in experimental heart failure with preserved ejection fraction 6 Sara Leite1,2*, Sara Rodrigues1,2*, Marta Tavares-Silva1,2,3, José Oliveira-Pinto1,2,4, Mohamed Alaa1,2,5, Mahmoud Abdellatif1,2, Dulce Fontoura1,2, Inês Falcão-Pires1,2, Thierry C. Gillebert6, Adelino F. LeiteMoreira1,2,7, André P. Lourenço1,2,8 7 8 9 10 1 11 12 13 14 15 16 17 Department of Physiology and Cardiothoracic Surgery, Faculty of Medicine, University of Porto, Porto, Portugal; 2Cardiovascular Research Centre, Faculty of Medicine, University of Porto, Porto, Portugal; 3Department of Cardiology, Hospital São João, Porto, Portugal; 4Department of Vascular Surgery, Hospital São João, Porto, Portugal; 5 Department of Cardiothoracic Surgery, Suez Canal University, Egypt; 6Department of Cardiology, Ghent University, Ghent, Belgium; 7Department of Cardiothoracic Surgery, Hospital São João, Porto, Portugal; 8Department of Anesthesiology, Hospital São João, Porto, Portugal 18 *these authors equally contributed to the manuscript. 19 20 21 Running Head: Afterload induced diastolic dysfunction in HFpEF 22 23 24 Corresponding author: 25 André P. Lourenço 26 Department of Physiology and Cardiothoracic Surgery, Faculty of Medicine, University of Porto 27 Medical Research Centre 28 Alameda Professor Hernâni Monteiro 29 4200-319 Porto, Portugal 30 Tel.: +351 225 513 644; fax: +351 225 513 646 31 E-mail address: [email protected] 1 Copyright © 2015 by the American Physiological Society. 32 Abstract 33 Myocardial stiffness and upward-shifted end-diastolic (ED) pressure-volume (P-V) relationship 34 (EDPVR) are the key to high filling pressures in heart failure with preserved ejection fraction (HFpEF). 35 Nevertheless, many patients may remain asymptomatic unless hemodynamic stress is imposed on 36 the myocardium. Whether delayed relaxation induced by pressure challenge may contribute to high 37 end-diastolic pressure (EDP) remains unsettled. Our aim was to assess the effect of suddenly 38 imposed isovolumic afterload on relaxation and EDP exploiting a highly controlled P-V experimental 39 evaluation setup in the ZSF1 obese rat model of HFpEF. Twenty-week old ZSF1 obese (ZSF1 Ob, 40 n=12), healthy Wistar-Kyoto (WKY, n=11) and hypertensive ZSF1 lean control rats (ZSF1 Ln, n=10) 41 underwent open-thorax left ventricular (LV) P-V hemodynamic evaluation under anesthesia with 42 sevoflurane. EDPVR was obtained by inferior vena cava occlusions to assess LV ED chamber stiffness 43 constant β and single-beat isovolumic afterload acquisitions were obtained by swift occlusions of the 44 ascending aorta. ZSF1 Ob showed increased ED stiffness, delayed relaxation, as assessed by time 45 constant of isovolumic relaxation (τ), and elevated EDP with normal ejection fraction. Isovolumic 46 afterload increased EDP without concomitant changes in ED volume or heart rate. In isovolumic 47 beats relaxation was delayed to the extent that time for complete relaxation as predicted by 3.5*τexp 48 exceeded effective filling time. EDP elevation correlated with reduced time available to relax which 49 was the only independent predictor of EDP rise in multiple linear regression. Our results suggest 50 delayed relaxation during pressure challenge to be an important contributor to lung congestion and 51 effort intolerance in HFpEF. 52 Keywords: afterload; relaxation; diastolic function; heart failure with preserved ejection fraction 53 2 54 New and Noteworthy 55 In a highly controlled hemodynamic evaluation set up in experimental heart failure with preserved 56 ejection fraction we demonstrate that delayed relaxation independently explains end-diastolic 57 pressure elevation during suddenly imposed afterload. This is an important contribution to 58 understand the response to exercise or hypertensive stress in preserved ejection fraction heart 59 failure. 60 3 61 Glossary 62 BSA, body surface area 63 CO, cardiac output 64 dP/dtmax, maximum rate of pressure rise 65 dP/dtmin, maximum rate of pressure fall 66 67 E/E’, ratio of peak early transmitral pulsed-wave Doppler flow velocity (E) to peak early diastolic tissue Doppler velocity (E’) 68 EDP, end-diastolic pressure 69 EDPVR, end-diastolic pressure volume relationship 70 EDV and EDVi, end-diastolic volume and indexed end-diastolic volume 71 EES, end-systolic elastance 72 EF, ejection fraction 73 HFpEF, heart failure with preserved ejection fraction 74 HR, heart rate 75 LV, left ventricle or left ventricular 76 LVMi, left ventricular mass index 77 NO, nitric oxide 78 Pmax, maximum developed pressure 79 PRSW, preload recruitable stroke work 80 S’, peak systolic tissue Doppler motion velocity 81 TAR, time available to relax 82 τ, time constant of isovolumic relaxation 83 4 84 Introduction 85 Heart failure with preserved ejection fraction (HFpEF) remains a major unsolved health issue and a 86 complex disease in which the contribution of various aspects is still incompletely understood (22, 87 24). Although HFpEF pathophysiology is multifarious and HFpEF patients constitute a heterogeneous 88 group comprising several risk factors (26) most experts would agree upon abnormalities of left 89 ventricular (LV) relaxation and high passive stiffness as underlying hemodynamic mechanisms (31) as 90 well as upon comorbidity and systemic inflammation-induced microvascular coronary endothelium 91 disturbances, decreased cardiomyocyte nitric oxide (NO) availability and protein kinase G activity as 92 key 93 hypophosphorylation, and interstitial fibrosis that ultimately lead to LV stiffening (23). On top of 94 these essential aspects, vascular stiffening and the effects of vascular reflection on myocardial load 95 and function are often underscored. Both magnitude and timing of load play a role in diastolic 96 function (5, 18). We have recently characterized a new cardiometabolic risk model of HFpEF that 97 recapitulates this paradigm. Despite preserved systolic function, hypertensive, obese and diabetic 98 ZSF1 obese rats show high end-diastolic pressure (EDP) and increased cardiomyocyte stiffness which 99 can be ascribed mostly to titin hypophosphorylation (9). Moreover, these animals show impaired 100 max and decreased anaerobic threshold in effort testing and low diastolic function tolerance to 101 both afterload and preload closely mimicking clinical HFpEF (20). Indeed, many patients who have 102 high passive stiffness may not show symptoms at rest. Underlying disturbances are only revealed 103 during exercise or hemodynamic stress suggesting that further diastolic function abnormalities come 104 into play (2). Our group has pioneered the investigation of the effects of sudden single-beat 105 afterload elevations in diastolic function. This in situ experimental preparation allows a full and 106 unique understanding of the interplay between afterload, relaxation and filling pressures without 107 the confounding of neurohumoral and reflex responses, overall hemodynamic status, ventricular 108 interdependence and pericardial constraint (16-19). In dogs and rabbits we have demonstrated a 109 biphasic response between afterload and relaxation. Small afterload elevations accelerate relaxation determinants to molecular remodeling (namely myocardial hypertrophy) titin 5 110 whereas large elevations delay relaxation (18) to the point where it becomes incomplete at end- 111 diastole enabling the build-up of residual EDP (17) defying the rough dichotomy between 112 independent active relaxation and passive elastance determinants of diastolic function and the view 113 that no matter how delayed relaxation is it may never impart on EDP (8). We have proposed that 114 delayed and incomplete relaxation might contribute to residual active force development at end- 115 diastole and thus constitute a pathophysiological mechanism in acute hypertensive lung edema (7) 116 which we labelled afterload-induced diastolic dysfunction (16, 17). Indeed, we have documented 117 that the diseased myocardium tolerates afterload elevations poorly both in patients with impaired 118 ejection fraction (19) and in a rat disease model (6). In healthy rats however likely owing to 119 particularities in myofilament composition and Ca2+ kinetics (21) only isovolumic afterload 120 significantly impaired relaxation with faint consequences in EDP (6). Most importantly, although it 121 may provide important mechanistic views on myocardial response to sudden afterload this 122 experimental set-up was never applied to the stiff HFpEF myocardium. 123 The aim of this study was to explore diastolic function response to sudden single-beat isovolumic 124 afterload elevation in ZSF1 obese rats and to ascertain the potential role of afterload-induced 125 diastolic dysfunction in experimental HFpEF. 6 126 Methods 127 Animal model 128 ZSF1 obese (ZSF1 Ob, n=12), ZSF1 lean (ZSF1 Ln, n=10) and Wistar-Kyoto rats (WKY, n=11; Charles 129 River Laboratories, Barcelona, Spain) were fed with standard diet (Purina diet 5008) to achieve 130 metabolic syndrome and HFpEF, systemic arterial hypertension or absence of any cardiovascular risk 131 factor, respectively, as previously reported (9). Animals were kept in individually ventilated 132 chambers, in groups of 2-per cage under controlled environment with a 12-h-light-dark cycle at 22°C 133 room temperature. All animals received humane care. Experimental procedures were approved by 134 the ethical committee of the Faculty of Medicine of Porto and were performed in accordance with 135 Portuguese law on animal welfare, EU Directive 2010/63/EU for animal experiments and the 136 National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH publication no. 137 85-23, revised 2011). Although we have formerly reported echocardiography data for this 138 experimental model (9), we performed confirmation echocardiography in 6 animals per group, as 139 previously described (9). 140 Hemodynamic studies 141 Briefly, animals were anaesthetized with sevoflurane (8 and 2.5–3% sevoflurane for induction and 142 maintenance, respectively; Penlon Sigma Delta) after sedation and analgesia with 100 µg.kg-1 and 5 143 mg.kg-1 intraperitoneal midazolam and fentanyl, respectively. Mechanical ventilation with positive 144 end-expiratory pressure held at 5 cmH2O, tidal volume set at 6 mL.Kg-1 and respiratory rate adjusted 145 to achieve normocapnia (MouseVent™ - Automatic Ventilator, Physiosuite, Kent Scientific) was 146 instituted upon endotracheal intubation (14G). Electrocardiogram (Animal Bio Amp, FE136, 147 ADInstruments), peripheral oximetry (MouseSTAT™ - Pulse Oximeter & Heart Rate Monitor, 148 Physiosuite, Kent Scientific), capnography, minute ventilation (CapnoScan™ - End-Tidal CO2 Monitor, 149 Physiosuite, Kent Scientific) and body temperature were recorded throughout. Temperature was 150 kept at 38oC on a heating pad (RightTemp™ - Temperature Monitor & Homeothermic Controller, 151 Physiosuite, Kent Scientific). Fluid replacement with heated Ringer’s lactate at 32 mL.kg-1.h-1 (NE- 7 152 1000, New Era Pump Systems) was instituted through a peripheral dorsal foot vein catheter (24G). 153 The heart was exposed by a left thoracotomy and the pericardium was widely opened. A flowmeter 154 probe was transiently placed in the ascending aorta for cardiac output (CO) calibration (2.5PS, 155 Transonic), a pressure-volume catheter (SPR-847 Millar Instruments) was inserted through the apex 156 and positioned along the LV long axis and 3-0 silk threads were passed around the inferior vena cava 157 and through a plastic tube to enable transient occlusions. Parallel conductance was determined by 158 40 μL 10% hypertonic saline injection and slope factor α was derived by simultaneous measurement 159 of CO by a flowmeter (TS420, Transonic). After a stabilization period of 30 mins, recordings were 160 obtained at suspended end-expiration. Transient 5-7 cycle occlusions of the inferior vena cava 161 occlusions were performed to obtain load independent indexes of LV contractility and chamber 162 stiffness by fitting the end-systolic and end-diastolic pressure-volume relationships (EDPVR) to a 163 linear and an exponential function, respectively, as previously described (9). After careful dissection, 164 single beat occlusions of the ascending aorta were performed with a non-traumatic vascular clamp 165 to assess diastolic response to isovolumic afterload. Clamping was performed during diastole and 166 maintained throughout systole, as reported (16). Three separate acquisitions were obtained and 167 averaged in every animal. Data with arrhythmia, heart rate (HR) changes higher than 2% or evidence 168 of incomplete afterload elevations were excluded. When several heartbeats were spanned in the 169 occlusion only the first beat after clamping was analyzed. Resting periods were allowed between 170 each intervention. Signals were continuously acquired (MPVS 300, Millar Instruments), digitized at 171 1000 Hz (ML880 PowerLab 16/30, ADinstruments), and analyzed offline (PVAN 3.5, Millar 172 Instruments). Time constant of isovolumic relaxation (τ) was computed by the logistic (τ log) and the 173 monoexponential (τ exp) methods. Prediction of time to complete relaxation was derived as 3.5* τ exp 174 based on Weisfeldt, et al.(29) and effective diastolic filling time was established as the time interval 175 from the maximum rate of pressure fall (dP/dtmin) to end-diastole (peak R wave of the ECG). To 176 account for large differences in body weight between groups, volumes were indexed for body 8 177 surface area (BSA) as estimated by 9.1*body weight in grams¾. Upon completion of experiments, 178 animals were euthanized by exsanguination under anesthesia. 179 Statistical analysis 180 Groups were compared regarding baseline hemodynamic parameters with one-way ANOVA or 181 Kruskal-Wallis according to normal or non-normal distribution, respectively, as verified by Shapiro- 182 Wilk’s test. Homogeneity of variances in ANOVA was checked by Levene’s test and corrected by 183 Welch’s F-ratio with adjusted degrees of freedom whenever violations occurred. Post hoc 184 comparisons were performed with Kramer’s modification for unequal group sizes of Tukey’s 185 method. The effects in isovolumic beats were assessed with mixed general linear models with group 186 and change from baseline to isovolumic as between-effect and within effect predictors, respectively. 187 Homogeneity of variances was verified with Bartlett’s test. Multivariate general linear models with 188 overall model estimation by Pillai’s trace followed by univariate test were used to compare groups 189 regarding joint changes in end-diastolic pressure and volume and to assess the influence of τ and 190 time available to relax on EDP. Deviations from sphericity were corrected with Huynh-Feldt’s 191 method. The influence of time available to relax and LV chamber stiffness constant β on EDP rise 192 during isovolumic beats was assessed by best subsets multiple linear regression with group recoded 193 as dummy variables. Standardized residual were carefully checked for normal distribution. Statistical 194 significance level was set at two-tailed 0.05. Data are presented as mean±standard error of mean. 195 9 196 Results 197 Baseline hemodynamic and single beat isovolumic parameters are summarized in Table 1 and 198 illustrated in Figures 1 and 2. Compared with WKY, ZSF 1 Ln showed higher maximum pressure 199 reached during systole (Pmax) which was further increased in ZSF 1 Ob. Chronic afterload was 200 accompanied by higher LV mass indexed for BSA (LVMi) which was significantly increased only in 201 ZSF1 Ob compared with WKY (Table 2). LV hypertrophy was confirmed on morphometric evaluation, 202 the ratio between LV plus interventricular septum mass to tibial length was increased (P=0.02) in 203 ZSF1 Ob (29.8 ± 2.1 mg.mm-1) compared with WKY (23.0 ± 0.7 mg.mm-1) but not with ZSF1 Ln (24.9 ± 204 1.2 mg.mm-1). ZSF1 Ob also showed baseline elevation in τexp, delayed onset of diastole as assessed 205 by dP/dtmin, higher EDP and an upward shift in EDPVR (Figure 2) as assessed by the LV chamber 206 stiffness constant for indexed volumes βi (Table 1). Cardiac index, ejection fraction (EF) and indexed 207 end-diastolic volume (EDVi) did not differ between groups (Table 1). Baseline maximum velocity of 208 pressure rise (dP/dtmax) was increased in ZSF1 Ob compared with WKY whereas end-systolic 209 elastance (EES) was increased in both ZSF1 groups compared with WKY, but the chamber size- 210 independent preload recruitable stroke work (PRSW) was unchanged (Table 1). Preserved EF and 211 unaltered peak systolic tissue Doppler motion velocity (S’) were confirmed on echocardiography, 212 along with an increase in the ratio of peak early transmitral pulsed-wave Doppler flow velocity to 213 peak early diastolic tissue Doppler velocity (E/E’), a surrogate of higher filling pressures, in ZSF1 Ob 214 compared with both ZSF1 Ln and WKY (Table 2). Changes in monoexponentially-derived τ were 215 confirmed by the logistic method. Because τexp is commonly used to predict the length of relaxation 216 and because τlog behaved like τexp we present results simply for τexp. No group differences were 217 observed in the maximum systolic pressure developed during isovolumic single beats Pmax (ISO) or 218 active developed pressures. Nevertheless, Pmax rose by 88 ± 11 % in WKY in the isovolumic beat 219 which was significantly higher (P<0.005) compared with both ZSF1 Ln and Ob (50 ± 4 and 33 ± 5 %, 220 respectively), denoting baseline work at a lower pressure level and better contractile reserve when 221 subjected to pressure challenge (represented by arrow in panel A of Figure 1). Indeed, if EES is 10 222 calculated by a single beat method that linearly fits the end-systolic pressure-volume of the baseline 223 beat and Pmax (ISO) at the corresponding volume (dotted lines in the lower panels of figure 1) ZSF1 Ob 224 has a slope of 0.16 ± 0.02 mmHg.μL-1.cm-2 which is significantly lower (P=0.002) than WKY (0.33 ± 225 0.04 mmHg.μL-1.cm-2) while ZSF1 Ln present intermediate values (0.25 ± 0.03 mmHg.μL-1.cm-2) 226 suggesting impaired contractility in the high pressure range in ZSF1 Ob. Regarding filling pressures, 227 the rise in EDP at the completion of the isovolumic beat however was higher in ZSF1 Ob compared 228 with both ZSF1 Ln and WKY (Table 1 and figure 1) independently of EDVi as confirmed by 229 multivariate analysis. Indeed, EDVi was virtually unchanged (Figure 3). To evaluate the determinants 230 of EDP elevation in ZSF1 Ob we conducted multivariate analysis of τexp and time available to relax 231 (TAR). Since prolongation of relaxation (τexp) can only impart on EDP in as much as its completeness 232 is delayed beyond the point of end-diastole, the variable TAR was defined as the difference between 233 effective diastolic filling time and time predicted to complete relaxation. Though time to dP/dtmin 234 was similarly increased by the isovolumic intervention in all groups (Table 1, Figure 4), τexp and TAR 235 were significantly prolonged and curtailed, respectively, in ZSF1 Ob compared with ZSF1 Ln and WKY 236 (Figure 4). Indeed, 7 out of 12 ZSF1 Ob animals presented negative TAR values, denoting incomplete 237 predicted relaxation at end-diastole whereas all of ZSF1 Ln and WKY animals showed positive values. 238 To further clarify the determinants of EDP rise in isovolumic beats we explored correlations with the 239 independent variables TAR and βi. Because individual subjects had a single observation for stiffness 240 constant but two for TAR the influence of TAR was assessed by expressing it as percentage change 241 from baseline to isovolumic beat (Figure 5). Although both correlations were significant, a stronger 242 correlation coefficient was observed for percent drop in TAR. Indeed, accounting for group as a 243 potential confounder, and after recoding as dummy variables, in multiple linear regression analysis 244 change in TAR and not βi was the only independent predictor of EDP rise (Table 3). 11 245 Discussion 246 We demonstrate that sudden single-beat isovolumic elevations of afterload delay relaxation and 247 shorten the time available to relax leading to residual high EDP independently from end-diastolic 248 stiffness in ZSF1 Ob rats with metabolic syndrome and HFpEF compared with hypertensive ZSF1 Ln 249 and healthy normotensive WKY controls. 250 Based on computer model simulations of the human cardiovascular system Hay et al. have predicted 251 that isolated impairment of active myocardial relaxation could generate elevated filling pressures in 252 the setting of rapid HR and increased systolic intervals (11). Our previous works with this 253 experimental set-up have been mainly conducted on healthy rabbits and dogs. The magnitude of 254 afterload that leads to incomplete relaxation and residual EDP was more obvious in the dog than in 255 the rabbit (17) and unremarkable in the healthy rat (6). Compared with previous works which were 256 carried out using volume estimation by sonomicrometry we used gold standard volume assessment 257 by conductance catheters clearly demonstrating that any changes in EDP cannot be attributed to 258 slight shifts in EDV. With this work we also further extend the role of afterload-induced diastolic 259 dysfunction to the setting of HFpEF. Contrarily to healthy WKY controls and hypertensive ZSF1 Ln 260 controls, ZSF1 Ob showed delayed and prolonged relaxation as assessed by τ and time to dP/dtmin, 261 respectively, that altogether led to insufficient time to relax, incomplete relaxation and high residual 262 EDP. Independently of LV myocardial diastolic stiffness, in this open thorax preparation a single 263 isovolumic beat raised EDP on average from 13 to 20mmHg. Moreover, as aforementioned rats are 264 particularly resistant to afterload induced diastolic dysfunction thus it is foreseeable that the effect 265 may be more relevant in closed-chest unanesthetized large animal and human physiology. This 266 finding addresses an important unsolved issue in HFpEF pathophysiology whether delayed relaxation 267 during exercise or afterload elevation can lead to EDP elevation per se. Westermann et al. compared 268 the response to handgrip exercise in HFpEF patients and controls and reported that despite similar 269 rises in systolic blood pressure up to 179 mmHg EDP rose from 15 to 24 mmHg in HFpEF patients 12 270 while no change were observed from the 6 mmHg baseline in controls (30). Curiously, and though no 271 significant changes were reported for EDV the authors attributed the rise in EDP to the steeper 272 EDPVR in HFpEF. In a similar study on another small subset of HFpEF patients with pressure-volume 273 evaluation during handgrip exercise Kawaguchi et al. on the other hand reported prolonged 274 relaxation and filling pressure elevation and suggested that ventricular-arterial stiffening 275 exacerbates hypertensive stress responses by delaying relaxation, limiting filling and raising diastolic 276 pressures (15). Our experimental results with isovolumic beats clearly indicate that the rise in EDP 277 can neither be attributed to a steeper EDPVR nor to increased end-diastolic volume. Indeed, in order 278 to achieve end-diastolic pressures of 20 mmHg, ZSF1 Ob would require an important increase in end 279 diastolic volume as represented in Figure 2 which was clearly ruled out by the conductance 280 methodology (Figures 1 and 3). Indeed, according to our multivariate analysis relaxation 281 disturbances clearly influenced EDP to a larger extent than chamber stiffness itself. Finally, we must 282 emphasize that our results in isovolumic beats were obtained under constant HR, increasing HR 283 during exercise will predictably enhance the effects of afterload–induced diastolic dysfunction. 284 Nevertheless, we must acknowledge that handgrip exercise is not a good representative of activities 285 of daily living. Borlaug et al. examined changes with supine dynamic exercise in HFpEF patients and 286 found enhanced relaxation. Although this was inadequate to compensate for tachycardia-induced 287 shortening of diastolic filling period, relaxation was still estimated to be complete by 50% of the 288 filling period (1). This can be partly explained by the distinct hemodynamic responses elicited by 289 isotonic aerobic exercise and isometric exercise. Indeed, isometric exercise usually evokes higher 290 blood pressure rise (15). Though isovolumic pressure challenge has no clinical counterpart, the 291 results from our proof-of-concept work underscore the role of sudden pressure challenge, during 292 effort or psychological, environmental, pharmacological and other forms of acute cardiovascular 293 stress, as a mechanism of acute decompensation in a stiff high-gain and poor-reserve ventricular- 294 arterial system as HFpEF. The pathophysiology of effort intolerance in HFpEF is multifarious but 13 295 delayed relaxation elicited by sudden pressure challenge may importantly contribute to elevate EDP 296 and cause an HFpEF patient to become symptomatic, as proposed by Borlaug et al. (4). 297 Beyond load and ventricular stiffening, many cellular and molecular determinants likely contribute 298 to impaired relaxation in HFpEF. Changes in protein kinase G activity (28), changes in myofilament 299 composition namely regarding titin a giant sarcomeric protein that mediates restoring forces and 300 length-dependent deactivation during the early phase of diastole (12) and that we have shown to be 301 hypophosphorylated in this experimental model (9) as well as disturbances in calcium kinetics (13) 302 may justify disturbed cross-bridge detachment and relaxation kinetics. Relaxation is both dependent 303 on cross-bridge detachment and calcium kinetics and impaired protein kinase G signaling which has 304 been reported in HFpEF patients (28) may be involved not only in titin hypophosphorylation but also 305 in increased calcium sensitivity of the myofilaments and slow cross-bridge detachment (14). 306 Recently, in old hypertensive dogs with HFpEF decreased troponin I, Myosin binding protein C and 307 myosin light-chain 2 hypophosphorylation along with increased calcium sensitivity were also 308 described and related to altered protein kinase activity (10) further supporting changes in regulatory 309 myofilament proteins as a likely molecular explanation for delayed relaxation in HFpEF. Moreover, 310 impaired myocardial bioenergetics may also be involved in delayed relaxation, as observed in HFpEF 311 patients (25). All of the aforementioned mechanisms that are already disturbed at baseline 312 explaining delayed relaxation in HFpEF will likely exacerbate load-induced slowing of relaxation in 313 HFpEF although their relative contribution and that of other potential molecular determinants 314 remains to be established. 315 Finally, though contractility indexes such as EES and dP/dtmax suggest hypercontractility in ZSF1 Ob, 316 PRSW which is not confounded by the size and geometry of the LV was unaltered. In fact, isovolumic 317 beats unmasked an impaired response to pressure challenge in ZSF1 Ob. Accordingly, we have 318 previously demonstrated that relaxation and contractility are closely related in sudden pressure 319 challenge (18) and subtle impairment of systolic function has been shown in HFpEF patients 14 320 particularly during effort (27). As proposed by Borlaug, et al. the inability to enhance contractility 321 upon imposed afterload may limit cardiac output reserve during effort and contribute to effort 322 intolerance (3). 323 In conclusion, in a highly controlled experimental setup that assesses the interplay between 324 afterload, relaxation and filling in the intact heart we have demonstrated in the ZSF1 obese rat 325 model of metabolic syndrome and HFpEF that acutely imposed afterload delays relaxation to the 326 extent that it imparts on end-diastole. Based on our experimental observations, incomplete 327 relaxation and build-up of residual EDP may contribute to high filling pressures and lung congestion 328 during hypertensive stress in HFpEF. 329 Grants 330 This work was supported by grants from the Portuguese Foundation for Science and Technology to 331 the Cardiovascular Research Centre of the Faculty of Medicine of Porto (EXCL/BIM-MEC/0055/2012 332 and PEST-C/SAU/UI 0051/2014) and from the European Commission (FP7-Health-2010; MEDIA- 333 261409). 334 Disclosures 335 The authors have no conflict of interest do disclose. 336 337 15 338 References 339 1. 340 relaxation and compliance reserve during dynamic exercise in heart failure with preserved ejection 341 fraction. Heart (British Cardiac Society) 97: 964-969, 2011. 342 2. 343 enhance diagnosis of early heart failure with preserved ejection fraction. Circulation Heart failure 3: 344 588-595, 2010. 345 3. 346 cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J Am Coll Cardiol 347 56: 845-854, 2010. 348 4. 349 diagnosis, and treatment. Eur Heart J 32: 670-679, 2011. 350 5. 351 St John Sutton M, and Gillebert TC. Early and late systolic wall stress differentially relate to 352 myocardial contraction and relaxation in middle-aged adults: the Asklepios study. Hypertension 61: 353 296-303, 2013. 354 6. 355 G, Vasques-Novoa F, Gillebert TC, and Leite-Moreira AF. Time course and mechanisms of left 356 ventricular systolic and diastolic dysfunction in monocrotaline-induced pulmonary hypertension. 357 Basic Res Cardiol 104: 535-545. Epub 2009 Mar 2014., 2009. 358 7. 359 pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 344: 17-22, 360 2001. 361 8. 362 pressure-volume relation. Circ Res 64: 827-852, 1989. Borlaug BA, Jaber WA, Ommen SR, Lam CS, Redfield MM, and Nishimura RA. Diastolic Borlaug BA, Nishimura RA, Sorajja P, Lam CS, and Redfield MM. Exercise hemodynamics Borlaug BA, Olson TP, Lam CS, Flood KS, Lerman A, Johnson BD, and Redfield MM. Global Borlaug BA, and Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, Chirinos JA, Segers P, Rietzschel ER, De Buyzere ML, Raja MW, Claessens T, De Bacquer D, Correia-Pinto J, Henriques-Coelho T, Roncon-Albuquerque R, Jr., Lourenco AP, Melo-Rocha Gandhi SK, Powers JC, Nomeir AM, Fowle K, Kitzman DW, Rankin KM, and Little WC. The Gilbert JC, and Glantz SA. Determinants of left ventricular filling and of the diastolic 16 363 9. Hamdani N, Franssen C, Lourenco A, Falcao-Pires I, Fontoura D, Leite S, Plettig L, Lopez B, 364 Ottenheijm CA, Becher PM, Gonzalez A, Tschope C, Diez J, Linke WA, Leite-Moreira AF, and Paulus 365 WJ. Myocardial titin hypophosphorylation importantly contributes to heart failure with preserved 366 ejection fraction in a rat metabolic risk model. Circulation Heart failure 6: 1239-1249, 2013. 367 10. 368 Myofilament Phosphorylation and Function in Experimental Heart Failure with Preserved Ejection 369 Fraction. Cardiovasc Res 97: 464-471, 2013. 370 11. 371 in the production of elevated left ventricular filling pressure. American journal of physiology Heart 372 and circulatory physiology 288: H1203-1208, 2005. 373 12. 374 Starling relation in early diastole. The Journal of general physiology 121: 97-110, 2003. 375 13. 376 Platzer D, Sokolow S, Herchuelz A, Antoons G, Sipido K, Pieske B, and Heinzel FR. Intracellular 377 dyssynchrony of diastolic cytosolic [Ca(2)(+)] decay in ventricular cardiomyocytes in cardiac 378 remodeling and human heart failure. Circulation research 113: 527-538, 2013. 379 14. 380 Kim KH, Kim YJ, Kim SJ, and Zhang YH. Myofilament Ca2+ desensitization mediates positive 381 lusitropic effect of neuronal nitric oxide synthase in left ventricular myocytes from murine 382 hypertensive heart. Journal of molecular and cellular cardiology 60: 107-115, 2013. 383 15. 384 stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and 385 diastolic reserve limitations. Circulation 107: 714-720, 2003. 386 16. 387 pressure-volume relation. American journal of physiology Heart and circulatory physiology 280: H51- 388 59, 2001. Hamdani N, Bishu KG, von Frieling-Salewsky M, Redfield MM, and Linke WA. Deranged Hay I, Rich J, Ferber P, Burkhoff D, and Maurer MS. Role of impaired myocardial relaxation Helmes M, Lim CC, Liao R, Bharti A, Cui L, and Sawyer DB. Titin determines the Frank- Hohendanner F, Ljubojevic S, MacQuaide N, Sacherer M, Sedej S, Biesmans L, Wakula P, Jin CZ, Jang JH, Kim HJ, Wang Y, Hwang IC, Sadayappan S, Park BM, Kim SH, Jin ZH, Seo EY, Kawaguchi M, Hay I, Fetics B, and Kass DA. Combined ventricular systolic and arterial Leite-Moreira AF, and Correia-Pinto J. Load as an acute determinant of end-diastolic 17 389 17. Leite-Moreira AF, Correia-Pinto J, and Gillebert TC. Afterload induced changes in myocardial 390 relaxation: a mechanism for diastolic dysfunction. Cardiovascular research 43: 344-353, 1999. 391 18. 392 its regulation by load and contractile state. Circulation 90: 2481-2491, 1994. 393 19. 394 MJ, Almeida J, Pinho P, and Gillebert TC. Diastolic tolerance to systolic pressures closely reflects 395 systolic performance in patients with coronary heart disease. Basic research in cardiology 107: 251, 396 2012. 397 20. 398 Lourenco AP. Echocardiography and invasive hemodynamics during stress testing for diagnosis of 399 heart failure with preserved ejection fraction: an experimental study. American journal of physiology 400 Heart and circulatory physiology ajpheart 00076 02015, 2015. 401 21. 402 research: advantages and disadvantages. Pharmacology & therapeutics 141: 235-249, 2014. 403 22. 404 prevalence and outcome of heart failure with preserved ejection fraction. The New England journal 405 of medicine 355: 251-259, 2006. 406 23. 407 fraction: comorbidities drive myocardial dysfunction and remodeling through coronary 408 microvascular endothelial inflammation. J Am Coll Cardiol 62: 263-271, 2013. 409 24. 410 inconvenient truth! Journal of the American College of Cardiology 55: 526-537, 2010. 411 25. 412 Steendijk P, Ashrafian H, Henning A, and Frenneaux M. Heart Failure With Preserved Ejection 413 Fraction Is Characterized by Dynamic Impairment of Active Relaxation and Contraction of the Left Leite-Moreira AF, and Gillebert TC. Nonuniform course of left ventricular pressure fall and Leite-Moreira AF, Lourenco AP, Roncon-Albuquerque R, Jr., Henriques-Coelho T, Amorim Leite S, Pinto JO, Silva MT, Abdellatif M, Fontoura D, Falcao-Pires I, Leite-Moreira AF, and Milani-Nejad N, and Janssen PM. Small and large animal models in cardiac contraction Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, and Redfield MM. Trends in Paulus WJ, and Tschope C. A novel paradigm for heart failure with preserved ejection Paulus WJ, and van Ballegoij JJ. Treatment of heart failure with normal ejection fraction: an Phan TT, Abozguia K, Shivu GN, Mahadevan G, Ahmed I, Williams L, Dwivedi G, Patel K, 18 414 Ventricle on Exercise and Associated With Myocardial Energy Deficiency. J Am Coll Cardiol 54: 402- 415 409, 2009. 416 26. 417 and Deo RC. Phenomapping for novel classification of heart failure with preserved ejection fraction. 418 Circulation 131: 269-279, 2015. 419 27. 420 The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography 421 reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, 422 untwist, and longitudinal motion. J Am Coll Cardiol 54: 36-46, 2009. 423 28. 424 JG, van der Velden J, Stienen GJ, Laarman GJ, Somsen A, Verheugt FW, Niessen HW, and Paulus 425 WJ. Low myocardial protein kinase G activity in heart failure with preserved ejection fraction. 426 Circulation 126: 830-839, 2012. 427 29. 428 relaxation in the dog: prediction from the time constant for isovolumic pressure fall. The Journal of 429 clinical investigation 62: 1296-1302, 1978. 430 30. 431 Poller W, Pauschinger M, Schultheiss HP, and Tschope C. Role of left ventricular stiffness in heart 432 failure with normal ejection fraction. Circulation 117: 2051-2060, 2008. 433 31. 434 and passive stiffness of the left ventricle. N Engl J Med 350: 1953-1959, 2004. Shah SJ, Katz DH, Selvaraj S, Burke MA, Yancy CW, Gheorghiade M, Bonow RO, Huang CC, Tan YT, Wenzelburger F, Lee E, Heatlie G, Leyva F, Patel K, Frenneaux M, and Sanderson JE. van Heerebeek L, Hamdani N, Falcao-Pires I, Leite-Moreira AF, Begieneman MP, Bronzwaer Weisfeldt ML, Frederiksen JW, Yin FC, and Weiss JL. Evidence of incomplete left ventricular Westermann D, Kasner M, Steendijk P, Spillmann F, Riad A, Weitmann K, Hoffmann W, Zile MR, Baicu CF, and Gaasch WH. Diastolic heart failure--abnormalities in active relaxation 435 19 436 Figure Legends 437 Figure 1. Superimposed representative baseline (dashed line) and isovolumic (continuous line) 438 pressure (panels A-C) and pressure-volume tracings (panels D-F) from Wistar-Kyoto (WKY, black 439 lines, panels A and D), ZSF1 lean (ZSF1 Ln, light gray lines, panels B and E) and ZSF1 obese rats 440 (ZSF1 Ob, dark gray lines, panels c and f). Tracings were obtained by averaging 20 evenly spaced 441 isophasic determinations in each of the animals from every group. Notice the conspicuous rise in 442 end-diastolic pressure (EDP) in the isovolumic beats from ZSF1 Ob compared with ZSF1 Ln and WKY. 443 Not only maximum pressure (Pmax) rises in the isovolumic beat (Pmax (ISO)) but also EDP (EDP (ISO)). In 444 the upper panels dotted lines are added to improve visualization of the differences between Pmax and 445 Pmax (ISO) between groups. In the lower panels dotted lines represent end-systolic elastance (EES) as 446 derived from the slope of single beat end-systolic pressure-volume relationships. In panel A the 447 arrow represents the higher contractile reserve in WKY (see text for detailed results). 448 Figure 2. End-diastolic pressure volume relationships (EDPVR) derived from transient inferior vena 449 cava (IVC) occlusions in Wistar-Kyoto (WKY, black lines), ZSF1 lean (ZSF1 Ln, light gray lines) and 450 ZSF1 obese rats (ZSF1 Ob, dark gray lines). Baseline (continuous) and sequential loops after IVC 451 occlusion (progressive shading) are represented. Tracings were obtained by averaging 20 evenly 452 spaced isophasic determinations in each of the animals from every group. A thick continuous line 453 represents the exponential fitting of the EDPVR. Notice the upward shift in ZSF1 Ob compared with 454 ZSF1 Ln and WKY. 455 Figure 3. End-diastolic pressure (EDP) and indexed volume (EDVi) at baseline (circles) and 456 isovolumic beats (triangles) in Wistar-Kyoto (WKY, white symbols), ZSF1 lean (ZSF1 Ln, light gray 457 symbols) and ZSF1 obese (ZSF1 Ob, dark grey symbols). Results for main effects of group (G), 458 intervention (I) and interactions (G*I) in multivariate (Multiv) and univariate (Univ) analyses are 459 provided. P<0.05 in post hoc tests: *vs WKY, †vs ZSF1 Ln, ‡vs rise of EDP in WKY and ZSF1 Ln. 20 460 Figure 4. Time available to relax (TAR) as a function of isovolumic relaxation time constant 461 calculated by the monoexponential method (τexp) at baseline (circles) and isovolumic beats 462 (triangles) in Wistar-Kyoto (WKY, white symbols), ZSF1 lean (ZSF1 Ln, light gray symbols) and ZSF1 463 obese (ZSF1 Ob, dark gray symbols). TAR was calculated as the difference between predicted 464 relaxation time as estimated by 3.5*τexp and effective diastolic filling time as assessed by the time 465 interval from the maximum rate of pressure fall (dP/dtmin) to end-diastole. Results for main effects of 466 group (G), isovolumic beat intervention (I) and interactions (G*I) in multivariate (Multiv) and 467 univariate (Univ) analyses are provided. ZSF1 Ob showed longer τexp compared with ZSF1 Ln 468 (†P<0.001) and WKY (*P<0.001) and shorter TAR compared with WKY (*P<0.01). Changes in τexp and 469 TAR during the isovolumic beat were more pronounced in ZSF1Ob compared with the other groups 470 (‡P<0.001). 471 Figure 5. Correlations between upward shift in end-diastolic pressure (ΔEDP) and curtailing of time 472 available to relax as percentage (panel A) and chamber stiffness constant for indexed volumes (βi, 473 panel B). Individual data from Wistar-Kyoto (WKY, white circles), ZSF1 lean (ZSF1 Ln, light gray 474 squares) and ZSF1 obese rats (ZSF1 Ob, dark gray triangles) are differentiated. Correlation 475 coefficients (R) and significance levels are presented. 476 477 478 479 480 21 Table 1. Hemodynamics. WKY ZSF1 Ln ZSF1 Ob HR, min-1 330 ± 12 374 ± 8 319 ± 16† BSA, cm2 454 ± 6 504 ± 6 659 ± 4*† CI, μL.min-1.cm-2 125 ± 9 128 ± 10 136 ± 6 EF, % 60 ± 3 55 ± 3 61 ± 4 EDVi, μL.cm-2 0.65 ± 0.03 0.68 ± 0.07 0.76 ± 0.07 dP/dtmax, mmHg.s-1 7860 ± 571 9340 ± 386 10240 ± 582* 0.077 ± 0.007 0.197 ± 0.031* 0.156 ± 0.020* 67 ± 3 64 ± 12 70 ± 9 0.016 ± 0.004 0.022 ± 0.006 0.027 ± 0.009† 109 ± 4 135 ± 2* 170 ± 6*† 204 ± 10‡ 204 ± 5‡ 223 ± 3‡ EDP, mmHg 6±1 5±1 13 ± 1*† EDP (ISO), mmHg 9 ± 1‡ 9 ± 1‡ 20 ± 2*†‡ § 8.7 ± 0.4 8.2 ± 0.4 12.5 ± 0.5*† 12.3 ± 0.8‡ 11.9 ± 1.4‡ 25.6 ± 1.6*†‡§ Time at dP/dtmin, ms 80 ± 4 81 ± 3 109 ± 8*† Time at dP/dtmin (ISO), ms 99 ± 5‡ 100 ± 6‡ 130 ± 6*†‡ ESPVR EES i, mmHg.μL-1.cm-2 PRSW, mmHg EDPVR βi, μL-1.cm2 Pmax, mmHg Pmax (ISO), mmHg τexp, ms τexp (ISO), ms Summary of hemodynamic variables for Wistar-Kyoto (WKY, n=11), ZSF1 lean (ZSF1 Ln, n=10) and ZF1 obese rats (ZSF1 Ob, n=12). HR, heart rate; BSA, body surface area, CI, cardiac index; EF, ejection fraction; EDVi, end-diastolic volume indexed for BSA; dP/dtmax, maximum rate of pressure rise; ESPVR EES i, end-systolic elastance derived from end-systolic pressure-volume relationship; PRSW, preload recruitable stroke work; EDPVR βi, left ventricular chamber stiffness constant derived from enddiastolic pressure-volume relationships; Pmax, maximum pressure; EDP, end-diastolic pressure; τexp, time constant of isovolumic relaxation derived by the monoexponential method; dP/dtmin, maximum rate of pressure fall. Data: mean ± SEM; P<0.05: * vs WKY and †vs ZSF1 Ln in post hoc group comparisons, ‡vs control beat as main effect, §rise vs other groups, denoting an interaction term. 1 Table 2. Echocardiography. WKY ZSF1 Ln ZSF1 Ob HR, min-1 286 ± 18 336 ± 10* 345 ± 13* LVMi, g.cm-2 1.0 ± 0.1 1.2 ± 0.1 1.3 ± 0.2* 74 ± 3 73 ± 4 74 ± 3 S’, cm.s-1 4.3 ± 0.9 5.7 ± 0.9 6.1 ± 1.2 E/E’ 11.4 ± 0.9 12.4 ± 0.7 18.0 ± 0.5*† EF, % Summary of echocardiography data for Wistar-Kyoto (WKY), ZSF1 lean (ZSF1 Ln) and ZF1 obese rats (ZSF1 Ob). HR, heart rate; LVMi, left ventricular mass indexed for body surface area; EF, ejection fraction; S’, maximum systolic tissue Doppler velocity at the lateral mitral annulus; E/E’, ratio between peak velocity of early filling in transmitral flow pulsed-wave Doppler and maximum velocity of early diastolic myocardial motion at the lateral mitral annulus. Data: mean ± SEM; P<0.05: * vs WKY and †vs ZSF1 Ln in post hoc group comparisons; n=6 per group. Table 3. Multiple linear regression of end-diastolic pressure elevation determinants. Standardized β ± SE 95% CI of β T (28) P value ΔTAR 0.549 ± 0.14 0.29 to 0.88 3.85 <0.001 CSC βi 0.05 ± 0.17 -0.38 to 0.42 0.26 0.80 Group 1 -0.03 ± 0.17 -0.40 to 0.36 -0.15 0.87 Group 2 0.16 ± 0.22 -0.38 to 0.66 0.71 0.48 Intercept 1.10 ± 0.90* -1.84 to 3.98 1.22 0.22 Overall model assessment: adjusted R2=0.30, F(1,31)=14.844, P<0.001. Standardized coefficients (β), standard errors (SE) and confidence intervals (CI) are provided as well as T test results for the appropriate degrees of freedom. Group 1 and 2 are dummy variables that recode the 3 groups in 2 binary variables. ΔTAR, percentage change from baseline to isovolumic beat of time available to relax; CSC βi, chamber stiffness constant for indexed volumes.