* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download cardiovascular examination
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
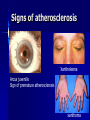
Common Approach to Cardiovascular Diseases / Physical Examination Prof. Dr. Muzaffer Değertekin [email protected] Yeditepe Univ. Hospital – 3rd Floor March 2015 Cardiology Physical Examination Coronary Artery Disease ECG Heart Failure Heart Valve Disease Acute Coronary Syndromes Restrictive and Hypertrophic Cardiomyopathy Cardiac Rhythm Problems EXAMINATION of the CARDIOVASCULAR SYSTEM General inspection Specific inspection Pulse Carotid Neck veins Praecordium Auscultation Lung bases,liver, ankles Veins and arteries in the legs GENERAL INSPECTION General build and appearence Colour Respiration (abnormal breathing pattern, shortness of breath) Signs of distress and response Conscious level SPECIFIC INSPECTION Cyanosis – Central: mucous membranes-tongue – Peripheral: extremities Clubbing Anemia Edema Peripheral perfusion Body habitus Specific signs of cardiac pathologies: IE stigmata, arcus senilis, xanthome and xanthelasma CYANOSIS and CLUBBING Signs of atherosclerosis Xanthelesma Arcus juvenilis Sign of premature atherosclerosis xanthoma IE/specific signs Body habitus: Marfan syndrome, thorax abnormalities Apical Impulse: Visualization to assess ventricular size/thickness Normally distinct and located at 4ICS at/inside the midclavicular line Apical Impulse (abnormal): Hyperdynamic impulse in normal location: think increased cardiac output or LVH Hyperdynamic and downward/leftwardly displaced: think LVE Indistinct impulse associated with RVH Precordial heave is seen with RVE Thrills: Palpation of a loud murmur Found in the precordial, suprasternal, or carotid artery area If low intensity murmur, probably just a pulsation and NOT a thrill Juguler venous pulse Patient position for JVP assessment JVP measurement HJR and Kussmaul’s sign Jugular Venous Pressure Waveform The PULSE Rate – Normal sinus 60-100bpm – Sinus bradycardia <60 bpm – Sinus tachycardia >100 bpm Regularity – Sinus arrhytmia: varies with respiration – Intermittant irregularity: ectopic beats – Continously irregular: atrial fibrillation Pulse volume and contour Palpation of large vessels Forearm, brachial, carotid, femoral Volume: normal/increased/decreased Pulse pattern: •Slow rising+/ brachial-radial delay (AS) •Collapsing (waterhammer) pulse (AR) •Bifid-Bisferiens (AS+AR, IHSS) •Pulsus paradoxus (Pericardial tamponade, COPD) •Pulsus alternans (LV dysfunction) Nabız Tipleri / Pulsation Types Pulsus Tardus (Yavaş Yükselen) Pulsus Parvus (Küçük Amplitüdlü) Dolgun Nabız (Nabız Basıncı Artmış) Corrigan Nabız Pulsus Altus ve Celer Pulsus Bisferiens Pulsus Alternans Pulsus Bigeminus Pulsus Paradoksus Dikrotik Nabız Auscultation Heart Sounds Timing of Heart Sounds S1 (cont.): If split heard better at the apex, may actually be S4 or ejection click Tends to be more low-pitched and long as compared to S2 Differentiate S1 from S2 by palpating carotid pulse: S1 comes before and S2 comes after carotid upstroke Decreased S1: Slowed ventricular ejection rate/volume Mitral insufficiency Increased chest wall thickness Pericardial effusion Hypothyroidism Cardiomyopathy LBBB Shock Aortic insufficiency First degree AV block Other Abnormal S1 (cont.): Increased S1: Increased cardiac output Increased A-V valve flow velocity (mitral stenosis) S2: From closure vibrations of aortic and pulmonary valves Divided into A2 and P2 (aortic and pulmonary closure sounds) Best heard at LMSB/2LICS Higher pitched than S1/better heard with diaphragm S2 splitting (normal): Normally split due to different impedance of systemic and pulmonary vascular beds Audible split with > 20 msec difference Split in 2/3 of newborns by 16 hrs. of age, 80% by 48 hours Harder to discern in heart rates > 100 bpm S2 splitting (normal, cont.): Respiratory variation causes splitting on inspiration: pulmonary vascular resistance When supine, slight splitting can occur in expiration When upright, S2 usually becomes single with expiration S2 splitting (abnormal, cont.): Fixed splitting ASD S2 splitting (abnormal, cont.): Wide /mobile splitting Mild PS RVOTO Large VSD or PDA Idiopathic PA dilation Severe MR RBBB PVC’s S2 splitting (abnormal, cont.): Reversed splitting LBBB WPW Paced beats PVC’s AS PDA LV failure Extra heart sounds S3 (gallop): Usually physiologic Low pitched sound, occurs with rapid filling of ventricles in early diastole Due to sudden intrinsic limitation of longitudinal expansion of ventricular wall S3 (cont.): Best heard with patient supine or in left lateral decubitus Increased by exercise, abdominal pressure, or lifting legs LV S3 heard at apex and RV S3 heard at LLSB S3 (abnormal): Seen in HF, severe MR--disappears after treatment S4 (gallop): Nearly always pathologic Can be normal in elderly or athletes Low pitched sound in late diastole Due to elevated LVEDP (poor compliance) causing vibrations in stiff ventricular myocardium as it fills S4 (cont.): Better heard at the apex or LLSB in the supine or left lateral decubitus position Occurs separate from S3 or as summation gallop (single intense diastolic sound) with S3 S4 Associations: CHF!!! HCM severe systemic HTN pulmonary HTN Ebstein’s anomaly myocarditis S4 Associations (cont.): Tricuspid atresia TAPVR CoA AS Kawasaki’s disease Ejection clicks Timing of Heart Sounds Cardiac murmurs Basic Pathophysiology Systolic Diastolic Describing a heart murmur 1. Timing – murmurs are longer than heart sounds – HS can distinguished by simultaneous palpation of the carotid arterial pulse – systolic, diastolic, continuous 2. Shape – crescendo (grows louder), decrescendo, crescendodecrescendo, plateau 3. Location of maximum intensity – is determined by the site where the murmur originates – e.g. A, P, T, M listening areas Describing a heart murmur con’t: 4. Radiation – reflects the intensity of the murmur and the direction of blood flow 5. Intensity – graded on a 6 point scale Grade 1 = very faint Grade 2 = quiet but heard immediately Grade 3 = moderately loud Grade 4 = loud Grade 5 = heard with stethoscope partly off the chest Grade 6 = no stethoscope needed *Note: Thrills are assoc. with murmurs of grades 4 - 6 Describing a heart murmur con’t: 6. Pitch – high, medium, low 7. Quality – blowing, harsh, rumbling, and musical 8. Others: i. Variation with respiration Right sided murmurs change more than left sided ii. Variation with position of the patient iii. Variation with special maneuvers Valsalva/Standing => Murmurs decrease in length and intensity EXCEPT: Hypertrophic cardiomyopathy and Mitral valve prolapse Systolic Murmurs Derived from increased turbulence associated with: 1. Increased flow across normal SL valve or into a dilated great vessel 2. Flow across an abnormal SL valve or narrowed ventricular outflow tract - e.g. aortic stenosis 3. Flow across an incompetent AV valve - e.g. mitral regurg. 4. Flow across the interventricular septum Systolic Murmurs Early Systolic murmurs 1. Acute severe mitral regurgitation – decrescendo murmur – best heard at apical impulse – Caused by: i. Papillary muscle rupture ii. Infective endocarditis iii. Rupture of the chordae tendineae iv. Blunt chest wall trauma 2. Congenital, small muscular septal defect 3. Tricuspid regurg. with normal PA pressures Midsystolic (ejection) murmurs Are the most common kind of heart murmur Are usually crescendo-decrescendo They may be: 1. Innocent common in children and young adults 2. Physiologic can be detected in hyperdynamic states e.g. anemia, pregnancy, fever, and hyperthyroidism 3. Pathologic are secondary to structural CV abnormalities e.g. Aortic stenosis, Hypertrophic cardiomyopathy, Pulmonic stenosis Pansystolic (Holosystolic) Murmurs Are pathologic Murmur begins immediately with S1 and continues up to S2 1. Mitral valve regurgitation – Loudest at the left ventricular apex – Radiation reflects the direction of the regurgitant jet i. To the base of the heart = anterosuperior jet (flail posterior leaflet) ii. To the axilla and back = posterior jet (flail anterior leaflet – Also usually associated with a systolic thrill, a soft S3, and a short diastolic rumbling (best heard in left lateral decubitus 2. Tricuspid valve regurgitation 3. Ventricular septal defect Diastolic Murmurs Almost always indicate heart disease Two basic types: 1. Early decrescendo diastolic murmurs – signify regurgitant flow through an imcompetent semilunar valve e.g. aortic regurgitation 2. Rumbling diastolic murmurs in mid- or late diastole – suggest stenosis of an AV valve e.g. mitral stenosis Diastolic Murmurs Continuous Murmurs Begin in systole, peak near s2, and continue into all or part of diastole. 1. Cervical venous hum – Audible in kids; can be abolished by compression over the IJV 2. Mammary souffle – Represents augmented arterial flow through engorged breasts – Becomes audible during late 3rd trimester and lactation 3. Patent Ductus Arteriosus – Has a harsh, machinery-like quality 4. Pericardial friction rub – Has scratchy, scraping quality Back to the Basics 1. When does it occur - systole or diastole 2. Where is it loudest - A, P, T, M I. Systolic Murmurs: 1. Aortic stenosis - ejection type 2. Mitral regurgitation - holosystolic 3. Mitral valve prolapse - late systole II. Diastolic Murmurs: 1. Aortic regurgitation - early diastole 2. Mitral stenosis - mid to late diastole SUMMARY A. Presystolic murmur – Mitral/Tricuspid stenosis B. Mitral/Tricuspid regurg. C. Aortic ejection murmur D. Pulmonic stenosis (spilling through S20 E. Aortic/Pulm. diastolic murmur F. Mitral stenosis w/ Opening snap G. Mid-diastolic inflow murmur H. Continuous murmur of PDA Summary Innocent murmurs Characteristics of Pathologic Murmurs Ankle-brachial index (ABI)