* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download pharmacology-lect-9-n-7-macrolide
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Drug discovery wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
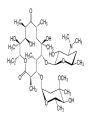
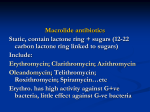
Protein Synthesis Inhibitors Dr. Naza M. Ali 9-1-2017 Lec-9 • These drugs selectively inhibit bacterial protein synthesis. • The selectivity is due to the differences between bacterial and human ribosomal proteins, RNA, and associated enzymes. • Bacteria have 70S ribosomes with 50S and 30S subunits • Mammalian cells have 80S ribosomes with 60S and 40S subunits. Classification of some antibacterial agents by their sites of action Macrolides The macrolides are a group of antibiotics with a Large cyclic lactone structure to which one or more deoxy sugars are attached. Macrolides -Erythromycin 125mg , 250mg, 500mg -Clarithromycin 500mg -Azithromycin 200mg, 250 mg, 500mg -Roxithromycin 150mg, 500mg -Spiramycin 1,500,000 IU 3,000,000 IU Mechanism of action • Macrolides bind irreversibly to a site on the 50S subunit of the bacterial ribosome, inhibiting the translocation steps of protein synthesis. • Also interfere with transpeptidation steps. • Bacteriostatic, or bactericidal higher doses Antibacterial spectrum Erythromycin: -is effective against many of the same organisms as penicillin G -it is used in patients who are allergic to the penicillins (syphilis) - It is used in Corynebacterium Diphtheriae Clarithromycin: -Same of erythromycin, active H.influenzae -Its has higher activity than that of erythromycin against Chlamydia, Legionella, Moraxella, H. pylori Azithromycin: -less active against strepto & staphyl than erythromycin -more active against respiratory infections due to H.influenzae , Moraxella catarrhalis. -preferred therapy for urethritis due to Chlamydia trachomatis (single dose). -Community acquired pneumonia (4 day course ) Resistance 1) The inability of the organism to take up the antibiotic or the presence of an efflux pump, both of which limit the amount of intracellular drug. 2) A decreased affinity of the 50S ribosomal subunit for the antibiotic. 3) The presence of a plasmid-associated erythromycin esterase. Pharmacokinetic: Absorption • The erythromycin base is destroyed by gastric acid So, either enteric-coated tablets or esterified forms of the antibiotic are administered. • All are adequately absorbed upon oral administration Clarithromycin, azithromycin, and telithromycin are stable to stomach acid and are readily absorbed. • Food interferes with the absorption of erythromycin & azithromycin, but can increase that of clarithromycin. Distribution: • Erythromycin distributes well to all body fluids except CSF. • It is one of the few antibiotics that diffuses into prostatic fluid, and it also accumulates in macrophages. • Clarithromycin, azithromycin are widely distributed in the tissues. • Azithromycin concentrates in neutrophils, macrophages, and fibroblasts. • Azithromycin concentration in phagocyte lysosomes can be 40 times higher than in blood and they can enhanced intracellular killing of bacteria by phagocytes • Inflammation allows for greater tissue penetration. • It has the longest half-life and the higher volume of distribution Pharmacokinetics Elimination: • Erythromycin and telithromycin are extensively metabolized hepatically. • They inhibit the oxidation of a number of drugs through their interaction with the CYP450 system. Excretion: • Erythromycin and azithromycin are primarily concentrated and excreted in the bile as active drugs. • Partial reabsorption occurs through the enterohepatic circulation. • Clarithromycin and its metabolites are eliminated by the kidney as well as the liver. • The dosage of this drug should be adjusted in patients with renal impairment. Excretion Adverse effects 1. GIT irritation 2. Cholestatic jaundice: ( erythromycin estolate form) 3. Ototoxicity: transient deafness at high dosage Contraindication: Patients with hepatic dysfunction should be treated with caution, because these drugs accumulate in the liver. Interactions: -Erythromycin, telithromycin, clarithromycin inhibit hepatic metabolism of a number of drugs, lead to toxic accumulations of these compounds. Telithromycin -Is a ketolide structurally related to macrolides. -same mechanism of action as erythromycin & a similar spectrum of antimicrobial activity. -some macrolide–resistant strains are susceptible to telithromycin. Clinical use: Community acquired pneumonia, other upper respiratory tract infections. Telithromycin is given orally once daily. Fidaxomicin • Is a macrocyclic antibiotic with a structure similar to the macrolides; Mechansim of action • it has a unique mechanism of action. -acts on the sigma subunit of RNA polymerase, -thereby disrupting bacterial transcription, - terminating protein synthesis, -and resulting in cell death in susceptible organisms. • Fidaxomicin has a very narrow spectrum of activity limited to gram-positive aerobes and anaerobes. • it possesses activity against staphylococci and enterococci • It is used primarily against Clostridium difficile. • Following oral administration, has minimal systemic absorption and primarily remains within GIT . • This is ideal for the treatment of C. difficile infection, which occurs in the gut. • This characteristic also likely contributes to the low rate of adverse effects. • Hypersensitivity reactions may occur. • Fidaxomicin should be used with caution in patients with a macrolide allergy, as they may be at increased risk for hypersensitivity.