* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PD-L1 - Stem Cell Conferences
Survey
Document related concepts
Transcript
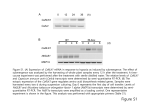
ACTIONS OF L-THYROXINE (T4) AND NANO-DIAMINO-TETRAC (NDAT, NANOTETRAC) ON PD-L1 IN CANCER CELLS Paul J. Davis, Hung-Yun Lin, Shaker A. Mousa Albany Medical College, Albany, NY, USA; Pharmaceutical Research Institute, Albany College of Pharmacy and Health Sciences; Taipei Medical University, Taipei, Taiwan The PD-1 (programmed death1)/PD-L1 (PD-ligand 1) checkpoint is a critical regulator of activated T cell-cancer cell interactions, serving to defend tumor cells against (T cell-mediated) immune destruction. Pharmaceutical interest is high in PD-L1 antibody use in solid tumor chemo-therapy to render cancer cells susceptible to host killer T cell action. We have developed a nonimmunological strategy for downregulation of PD-L1 gene expression and PD-L1 protein content in tumor cells. • The non-immunologic strategy is based on pharmacologic regulation of a target on the extracellular domain of plasma membrane integrin avb3. This target is a thyroid hormone-tetraiodothyroacetic acid (tetrac) receptor that controls—from the cell surface— the expression of a panel of cancer cell defense genes, including PDL1. -I - -I 3’ HO 3 NH2 CH2-CH-COOH O 5’ 5 -I - -I - Thyroxine (T4) -I - -I 3’ 3 CH2-CH-COOH O 5’ NH2 5 -I - 3,5,3’-Triiodothyronine (T3) -I - -I 3’ HO 3 CH2--COOH O 5’ 5 -I - -I - Tetrac Low-grade thyromimetic within cells TH antagonist at integrin avb3 TH receptor I O O N H N H I O O I I OH PLGA nanoparticle N O H H N I O O I I I O OH In Nanotetrac, shown here, tetrac is covalently bound to a linker (ether bond) which, in turn, is amide-bonded to a PLGA nanoparticle. The action of tetrac is limited in this formulation to the thyroid hormone-tetrac receptor on the extracellular domain of integrin avb3. Figure 1 • Human triple-negative breast cancer (MDA-MB-231) cells and human colon cancer (HCT116. HT29) cells were cultured in DMEM (breast) or RPMI-1640 (colon), each with 10% FBS. Two days prior to study of cells, 0.25% charcoal-stripped serum replaced 10% FBS. • Cells were treated with L-thyroxine (T4, 10-7 M total hormone, 10-10 M free), NDAT (10-7 M tetrac equivalent) or both for 24 h. • Tumor cell RNA was harvested and PD-L1 mRNA quantitated by qPCR. • PD-L1 protein was measured by western blotting. MDA-MB 231 cell mRNA abundance A. B. Figure 2 MDA-MB 231 cell PD-L1 protein content A. B. 50 kDa - ◄ PD-L1 36 kDa - ◄ GAPDH 36 kDa - 50 kDa - 2.7-fold increase 25-35% decrease in content with NDAT Figure 3 ◄ PD-L1 ◄ GAPDH HCT116 cell mRNA A. B. Figure 4 HCT116 cell PD-L1 protein A. B. 50 kDa - ◄ PD-L1 36 kDa - ◄ GAPDH 50 kDa - ◄ PD-L1 36 kDa - ◄ GAPDH 25-60% decrease in basal or stimulated content with NDAT Figure 5 HT-29 cell mRNA A. B. Figure 6 HT-29 cell protein A. 50 kDa - 36 kDa - B. ◄ PD-L1 50 kDa - ◄ PD-L1 36 kDa - ◄ GAPDH ◄ GAPDH 40% decrease in basal or stimulated content with NDAT Figure 7 Dependence on MAPK of induction by T4 of PD-L1 in cultured HCT116 cells - PD98059 NDAT (10-7 M) T4 (10-7 M) - + - - + + PD98059 + + - + - - + + + 50 kDa - ◄ PD-L1 36 kDa - ◄ GAPDH Figure 8 SUMMARY • In MDA-MB-231 breast cancer cells, T4 significantly stimulated PDL1 gene expression by 40% and increased PD-L1 protein 2.7-fold; these effects were blocked by NDAT. • In HCT116 and HT-29 colon carcinoma cells, T4 significantly increased PD-L1 gene expression by 20-60% and protein abundance by 25-65%; these effects were blocked by NDAT. • Basal levels of mRNA and protein were also reduced by NDAT. • MAPK mediates the T4 effects. CONCLUSIONS • The PD-1/PD-L1 defensive tumor cell checkpoint is T4 responsive. Host patient T4 supports this cancer cell defense. • Hormonal effects vary among cell lines. • NDAT eliminates the contribution of T4 to the checkpoint and also variably reduces basal levels of PD-L1.