* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Doctor I feeling Dizzy - ACM
Auditory system wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Hyperkinesia wikipedia , lookup
Auditory brainstem response wikipedia , lookup
Motion sickness wikipedia , lookup
Psychopharmacology wikipedia , lookup
Hemiparesis wikipedia , lookup
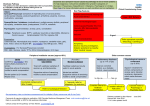
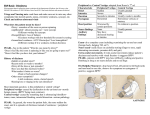
“Doctor I feel Dizzy” AIMGP Seminar 2004 Yash Patel Objectives Develop an approach to the evaluation of “dizziness” Review Etiology Prognosis Diagnostic Evaluation Treatment Background Acute Vestibular Syndrome NEJM 1998; 339:680-5 Vestibular Neuritis NEJM 2003; 348:102732 Benign Paroxysmal Positional Vertigo NEJM 1999; 341:1590-96 Vertigo Lancet 1998; 352: 1841-46 “Take Home Message” Dizziness is a common symptom Clinical History is very important in determining the “Type” of dizziness The Prognosis for most patients is good Investigations are helpful only in selected patients Real Cases… Case A 61 M Sudden onset dizziness, sweating, blurred vision Wobbling when walking, holding on to things Case B 79 F “Weak and dizzy” Episodic dizziness and “roaring in the ear” Felt unsteady on her feet Real Cases… Case A Nystagmus horizontal gaze, no diplopia Broad based gait Positive Romberg sign Normal motor and sensory exam CT head normal Case B CN II-XII normal Normal motor and sensory exam Cerebellar testing normal Gait was broad based Background Dizziness is a non-specific term used by patients to describe symptoms It is a common symptom 7 million clinic visits/year in U.S. Dizziness can represent many different overlapping sensations Caused by different pathophysiologic mechanisms Mechanism of Balance Visual receptors provide a stable retinal image during movement Proprioceptive receptors provide info on gravity, position, and motion of muscles and joints Vestibular receptors provide info on the direction and speed of motion Mechanism of Balance Integration of receptor information at the vestibular nuclei and cerebellum Perception of balance is the role of cortical integration and interpretation of signals Dizziness results when a mismatch occurs between these receptors or levels of the balance system Approach to Dizziness History important to ask open-ended questions and listen to the description of symptom Symptom Based Approach (Drachman and Hart, Neurology; 1972) Proposed a “complaint-oriented” approach to classifying patients with dizziness Although symptoms are described differently by each patient they can be classified into one of four categories Four symptom categories A. Sensation of Motion (vertigo) B. Sensation of Impending Faint (pre-syncope) C. Sensation of Losing one’s balance (dysequilibrium) D. Ill-Defined Lightheadedness (not A,B,C) A. Vertigo Experience an illusion of motion between self and environment. Perception that the world is moving or the body is moving Usually accompanied with excessive autonomic activity (Nx/Vx, pallor, diaphoresis) Disturbance of vestibular function “Central”: lesions of brainstem or cerebellum “Pheripheral”: lesions of labyrinth or VIIIth nerve A. Vertigo “Central” (lesions of brainstem or cerebellum) Vertigo is NOT the dominant symptom Signs/symptoms of brainstem or cerebellar involvement Causes Brainstem or cerebellar infarction Posterior fossa tumors Multiple sclerosis A. Vertigo “Peripheral” (lesion of the labyrinth or VIII nerve) vertigo ± auditory symptoms Causes Benign Paroxysmal Positional Vertigo Vestibular Neuronitis/Labyrinthitis Meniere’s Syndrome Post traumatic or Ototoxicity A. Vertigo Aids to differentiate Central vs Peripheral Nausea Imbalance Hearing Neurologic Compensation and Loss Symptoms Vomiting Peripheral Severe Mild Common Rare Rapid Central Moderate Severe Rare Common Slow A. Vertigo BPPV brief episodes of vertigo with position change usually lasts < 30s idiopathic, after viral infection or trauma no hearing change Vestibular Neuronitis sudden onset severe vertigo with nausea and vomiting lasts hours to days no hearing loss A. Vertigo Labyrinthitis sudden onset severe vertigo with nausea and vomiting lasts hours to days associated hearing loss or tinnitus usually follows viral upper respiratory tract infection Menieres episodic vertigo lasts hours fluctuating hearing loss, tinnitus A. Vertigo Vertigo lasting day or longer Vestibular neuritis, labyrinthitis Brainstem/Cerebellar infarction MS Vertigo lasting hours or minutes Meniere’s TIA or Migraine headache Vertigo lasting for seconds BPPV B. Presyncope Involves the patient’s perception that they are about to faint Can be associated with Nx, pallor, diaphoresis, or narrowing of visual field B. Presyncope No difference in the DDx of presyncope and syncope Cardiovascular (20%) Arrhythmic Obstruction to cardiac output Noncardiovascular (45%) Vasovagal orthostatic psychogenic Unknown (35%) C. Dysequilibrium Sensation of losing one’s balance without a feeling of illusionary movement Typically patients do not report symptoms sitting or lying, but notice unsteadiness standing or walking C. Dysequilibrium Neurologic disorder disruption in the integration of sensory inputs and motor output Causes Peripheral neuropathy alcohol, drugs, DM, B12 Central C-P angle or posterior fossa tumors Cerebellar degeration Extrapyramidal disorders (Parkinson’s) Drugs (carbamazepine, phenytoin) Multiple sensory deficits (decreased vision and sensation) D. Ill Defined Lightheadedness Vague sensation not characteristic of vertigo, pre-syncope, or dysequilibrium Psychophysiologic dizziness impaired central integration of sensory signals Psychiatric disorders primary cause of nonspecific dizziness D. Ill Defined Lightheadedness Causes Major depression (25%) Generalized anxiety or panic disorders (25%) Somatization disorders Alcohol dependence Personality disorders Focus of Evaluation Type of Dizziness Focus of Evaluation A. Vertigo Auditory and vestibular system B. Presyncope Cardiovascular system C. Dysequilibrium Visual, peripheral and central nervous system D. Ill-defined Psychosocial issues Physical Examination A. Vertigo B. Presyncope Eyes for nystagmus Assess hearing Signs of brainstem involvement Able to walk Hallpike maneuver (see next slide) Cardiac and vascular exam Heart rhythm Orthostatic blood pressure Hallpike Maneuver Physical Examination C. Dysequilibrium Vision Sensation and Position Cerebellar testing Gait D. Ill-defined No diagnostic physical signs Special Tests A. Vertigo Central: Peripheral: neuroimaging of brainstem audiometry, electronystagmography B. Presyncope Cardiac: ECG, Holter, Echocardiogram Noncardiac: Tilt table testing Special Tests C. Dysequilibrium Visual testing Neuroimaging Nerve conduction studies D. Ill-defined Psychiatric evaluation Treatment Treatment can be considered in terms of three categories 1. Specific Treat the underlying cause 2. Symptomatic Control symptoms of vertigo, nausea and vomiting Antihistamines (meclazine, diphenhydramine) Phenothiazines (CPZ) Anticholinergic (scopolamine) Treatment 3. Rehabilitative Vestibular exercises to stimulate “dizziness” is necessary for compensation to occur Physiotherapy Etiology, Prognosis, and Evaluation (Hoffman, Am J Med. 1999) Etiology (most common etiologies) Peripheral vestibular (35-55 %) Psychiatric (10-25 %) Cerebrovascular disease (5 %) Brain Tumors (< 1%) History and Physical lead to diagnosis in 75 % Etiology, Prognosis, and Evaluation (Hoffman, Am J Med. 1999) Prognosis Most symptoms were self limited Persistent dizziness impaired quality of life Diagnostic Testing Routine lab testing as well as cardiovascular and neurologic testing had a low yield in unselected patients Back to Cases… Case A 61 M Sudden onset dizziness, sweating, blurred vision Wobbling when walking, hold on to things Case B 79 F “Weak and dizzy” Episodic dizziness and “roaring in the ear” Felt unsteady on her feet Back to Cases… Case A Nystagmus horizontal gaze, no diploplia Broad based gait Positive Rhomberg sign Normal motor and sensory exam CT head normal Dx: Vestibular Neuronitis Case B CN II-XII normal Normal motor and sensory exam Cerebellar testing normal Gait was broad based Dx: Menieres Approach to Dizziness Veritigo (sensation of motion) Presyncope (sensation of fainting) Disturbance of vestibular function Decreased cerebral perfusion “I am dizzy” Dysequilibrium (unstedy gait) Ill-defined Neurologic disorder Psychosocial disorder Central Brainstem/Cerebellar infarction Posterior fossa tumors MS Peripheral BPPV/Vestibular neuritis Labyrinthitis/Meniere’s Post traumatic vertigo Cardiac Arrhythmia Aortic stenosis/HOCM Noncardiac Vasovagal Orthostatic Peripheral neuropathy Alcohol DM/B12 Drugs Central Cerebellar disease Posterior fossa tumors Extrapyramidal disorders Drugs Depression Anxiety or Panic disorder Personality disorder Hyperventilation “Take Home Message” Dizziness is a common symptom Clinical History is very important in determining the “Type” of dizziness The Prognosis for most patients is good Investigations are helpful only in selected patients