* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac CheckPoint study notes
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
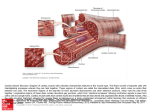
Review Tips for Adult Health Cardiac CarePoint as given by Dr. Cummings Mayo Clinic Hospital October 6, 2009 1. Know the signs and symptoms of heart failure a. Right-sided heart failure: congestion in the body. Peripheral edema Systemic Congestion [1] JVD [2] Enlarged liver and spleen [3] Anorexia and Nausea (Megase) [4]Dependent edema (legs and sacrum) [5] Swollen hands and fingers [6] Polyuria at night [7] Weight gain (most reliable indicator of fluid loss/gain) [8]Increased BP (from excess volume) or decreased BP (from failure) b. Left-sided heart failure: congestion in the lungs. Dsypnea, orthopnea Decreased Cardiac Output [1] Fatigue [2]Weakness [3] Oliguria during the day [4] angina [5] Confusion/restlessness [6] Dizziness [7]Tachycardia [8] Pallor [9] Weak peripheral pulses [10] Cool extremities Pulmonary Congestion [1] hacking cough, worse at night [2] Dyspnea [3] Crackles/wheezes in lungs [4] Frothy, pink-tinged sputum [5] Tachypnea [6] S3/S4 Gallop [7] AFIB is common 2. Know about the role of sodium retention in heart failure decreased blood flow to the kidneys stimulates production of renin. Activating the RAAS promotes retention of sodium and fluids to raise blood pressure. This causes increased afterload, which causes ventricular remodeling. Hypertrophied muscle uses more oxygen and also has decreased contractility. Decreased contractility leads to increased preload and further decrease in contractility. This decrease in contractility leads to decrease in cardiac output, which starts the whole cycle over again. 3. Weighing patients – can assess fluid volume changes by changes in weight. 4. Review CAD (Coronary Artery Disease) and atherosclerosis a. Definitions: CAD: a narrowing of the arteries that supply the heart with blood due to accumulation of plaque. Increases risk for an MI. Includes stable angina and acute coronary syndromes. When blood flow through coronary arteries is blocked, ischemia and/or infarction can occur. atherosclerosis: collecting of plaques (cholesterol, lipids, cellular debris) in the inner layer of the walls of arteries. b. Causes/risk factors i. Modifiable risk factors: HTN, hyperlipidemia, diabetes, smoking, obesity, sedentary lifestyle, stress ii. Non-modifiable risk factors: age, gender, race/ethnic background, heredity c. Dietary factors and dietary modifications as part of treatment plan 5. Know med classes for blood pressure control (the list below is from Dr. Ancheta’s PowerPoint presentation): a. Diuretics: thiazides are first. (most “gentle”) b. Beta-Blockers: “-olol” - block beta receptors (beta1 is specific to heart. Nonspecific for beta1 and beta2 can have pulmonary side effects) Beta1 is adrenergic (stimulatory). Blocking these prevents vasoconstriction → lower BP. c. Calcium channel Blockers: diltiazem, cardizem – block calcium from entering smooth muscle, prevents vasoconstriction → lower BP. Also slows heart rate. d. ACEIs / ARBs: ACEIs (“-pril”) act in lungs; ARBs (“-sartan”) act in kidneys. Both work by interrupting the RAAS, thus keeping overall volume and BP lower. e. Vasodilators: actually dilate blood vessels (whereas other HTN meds work by preventing vasoconstriction, but don't actually cause dilation). Examples include clonidine (Catapres), doxazosin (Cardura) 6. If you want to decrease blood pressure rapidly (you can’t wait for something like an ACEI or ARB to take effect), then use one of the following: a. Calcium channel blocker (e.g. – nicardipine, brand name Cardene) b. Alpha blocker (e.g. – phentolamine, brand name Regitine) i. NOTE: I believe Dr. Cummings said “alpha blocker”, but then went on to give an example, clonidine (brand name Catapres), which is an alpha agonist, not antagonist. Clonidine is available PO and as a transdermal patch, with an onset of action of 30 minutes or more. While this is still faster than the hour or more that it takes for an ACEI to start working, it’s still pretty slow—maybe clonidine was not what she intended to use as an example. I did some research, and phentolamine is an alpha blocker, works immediately to reduce blood pressure when given IV, and is used to treat hypertensive crisis. 7. A-fib – treat with both: a. Diltiazem (Cardizem) – a calcium channel blocker b. Warfarin (Coumadin) – anticoagulant (due to higher risk of clotting from A-fib) 8. Know the importance of the ST segment a. ST depression = ischemia. A non-STEMI means you are having an ischemic attack, not an infarction. Not good, but better than a STEMI. b. ST elevation = MI i. 80% of MIs are STEMIs (ST Elevation Myocardial Infarctions) 9. Know the labs for an MI (the list below is straight from Dr. Ancheta’s PowerPoints): a. Troponin T and I- myocardial muscle protein released into the bloodstream with injury to the myocardial muscle (not found in healthy clients) b. Creatine kinase - MB (CK-MB) is an enzyme specific to cells of the brain, myocardium and skeletal muscle. Indicates tissue necrosis or injury, Cardiac specificity is determined by measuring the isoenzyme activity CK-MB is found in myocardial muscle CK-MM (skeletal) CK-BB (brain) c. Myoglobin early marker of MI is a low-molecular-weight heme protein found in cardiac and skeletal muscle, appears as early as 2 hours after an MI with rapid decline after 7 hours d. C-Reactive Protein is a marker of inflammation. Any inflammatory process can increase CRP in the blood 10. “There may be something on there about the major EKG leads.” a. No details on this. Other notes/clarification: Systolic dysfunction – ejection fraction <40%. EF is decreased because ventricle is so full prior to contraction (increased preload) that the muscle fibers are so stretched and it doesn't contract efficiently enough to expel the blood from the chamber. diastolic dysfunction – ejection fraction is normal or higher than normal. Muscle is becoming thicker/hypertrophied. Pumps blood out, but less empty space in the ventricle for blood to fill, and the larger muscle is requiring more oxygen. *both are types of left-sided HF