* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Left Ventricular Assist Devices
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
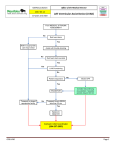
LVADs LeftVentricularAssistDevices MeganBoysen Osborn,MD,MHPE AlisaWray,MD Khuansiri Narajeenron,MD CommonMechanicalCirculatorySupportDevices Origin Destination Left VentricularAssist Device(LVAD) LeftVentricle Aorta RightVentricularAssist Device(RVAD) RightVentricle Pulmonary Artery ExtracorporealMembrane Oxygenation(ECMO) Veno-arterial(VA) Common femoralveinà IVC/RAjunction Common femoralarteryà Iliacartery ECMO Veno-venous (VV) VVDualChamber Rightcommon femoralvein Rightinternaljugular vein RIJ->SVC/IVC Rightatrium TandemHeart Leftatria Descending aorta Intraaortic Balloon Pump (IABP) Aorta Aorta Impella Left ventricularoutflow tract Aorta Whydopeoplehave anLVAD? • Bridgetohearttransplantation(BTT) • DestinationTherapy(DT) • Bridgetorecovery(BTR) FirstGeneration LVADs 1995 PulsatileFlow Intraabdominal Insertion “BridgetoTransplant” 18–24months* 2003:DestinationTherapy SecondGeneration LVADs 2003 Continuous Flow Intraabdominal Insertion “BridgetoTransplant”or “DestinationTherapy” Somearealive>10years ThirdGenerationLVADs 2012 Electromagnetic; Pulsatile,Continuous flow Intrathoracic Insertion “BridgetoTransplant” ImagefromReliantHeart:http://reliantheart.com/new-heart-assist-5/smallest-size-and-weight/ ImageCourtesy: ByNationalHeartLungandBloodInstitute(NIH)(NationalHeartLungand BloodInstitute(NIH))[Publicdomain],viaWikimedia Commons Cost MillerLW,Guglin M,RogersJ.CostofVentricularAssistDevices:CanWeAffordtheProgress?Circulation2012;127:743-748 Complications Mostcommoncausesofdeath • CardiacFailure • Infection • CNSEvent Source:Kirklin JK,etal.JHeartLungTransplant.2010Jan;29(1):1–10 Complications ReasonstheymightpresenttoyourED • Dysrhythmia • Infection/Sepsis(Driveline) • CNSEvent(Ischemicorhemorrhagicstroke) • Bleeding • Pumpfailure/thrombosis • Tamponade • PulmonaryEmbolism • AorticDissection • LVADSuctionEvent Management • CalltheLVADCoordinator • Checkwhetherdeviceisworking(skin signs,hum/vibration,MAP) • Checkconnections,plugintowall(need powerpack) • Checkalarms • Echo Management • Fluids,?pressors? • TrytoavoidCPR • Candefibrillate/cardiovert (avoiddirectlyover thedevice) • ConsiderTPA/heparinvs.reversalofanticoagulation • Checkpotassium • TRANSFER CommonAlarms iRAT individual Readiness Assessment Test gRAT group Readiness Assessment Test GAE group application exercise Post test kahoot! Left Ventricular Assist Device (LVAD) Complications Nick Stadlberger, MD C Partyka et al. Emerg Med Australas, 2014. PMID 24707998 M Anderson et. al. J Heart Lung Transplant, 2009 PMID 19560703 JC Greenwood et al. Emerg Med Clin North Am, 2014. PMID 25441039 Tips • These patients MAY NOT HAVE A PULSE o May need ABG since pulse ox may be inaccurate without pulse • Contact your hospital’s or network’s LVAD Coordinator immediately to help with management and troubleshooting. • Patients are usually on diuretics, and may intravascularly depleted or have electrolyte abnormalities Image used with permission of Mayo Foundation for Medical Education and Research 1 st 2 nd rd 3 th 4 LVAD Patient in Extremis: Step-Wise Diagnostic Approach Address airway, breathing, circulation; Obtain IV, O2, monitor Measure blood pressure: May need manual cuff with Doppler to obtain mean arterial pressure (MAP), or use arterial line (MAP goal 70-80 mmHg) • Assign someone to call LVAD Coordinator • Auscultate precordium. Is there a hum? − Yes ! LVAD is working. No ! LVAD is not working. • Battery – Make sure it is plugged in. • Controller – Check for alarms. • Driveline – Check device type, evidence of infection/damage • Echocardiogram • Obtain VAD variables: Flow, Power, Speed, Pulsatility Index • Obtain ECG • Obtain labs (CBC, electrolytes, coagulation studies, LDH, type and screen given GI bleed risk, ± blood cultures for infection concern, ± ABG) • • Echocardiogram Findings Big RV + Big LV Big RV + Small LV Small RV + Small LV Potential Causes Pump failure, Pump thrombosis Valve disorders Right heart failure, ST-elevation MI Pulmonary hypertension Note: If LV to outflow cannula size ratio is 1:1, then high risk for suction event Hypovolemia Sepsis GI bleed Management (with LVAD team) Heparin, antiplatelet agents, thrombolytics IV fluids, ECG, consider inotropes IV fluids, consider blood transfusion, antibiotics Updated 11/21/16 LVAD Complication Arrhythmia Infection Thrombus (pump thrombus, PE, stroke/TIA) Bleeding Suction Event (An underfilled LV causing suction of myocardium into LVAD) RV Failure Cannula Malposition Device Malfunction, Pump Failure Comment Up to 50% with sustained VT/VF in first 4 weeks after LVAD placement Difficult to determine primary vs. secondary cause: • Primary: compromised myocardium + scar tissue Secondary: electrolyte abnormalities, hypotension, suction events Up to 42% experience sepsis within 1 year (REMATCH Study). Most infections are in first 3 months. 9% are fungal. High risk despite anticoagulation. Pump thrombus suggested by warm device and increased power output. Elevated LDH Patients may have an acquired Von Willebrand Disease coagulopathy Can be caused by right heart failure, hypovolemia, sepsis, restrictive cardiomyopathy, arrhythmias Due to AMI or previous RV failure Consider in setting of new VT, suction event, chest compressions, or trauma Suggested if no hum and MAP <40 mmHg Management (with LVAD team) Depending on the cause: • IV fluid challenge is reasonable • Reduce pump speed • Correct electrolytes • Electrical or pharmacologic (amiodarone) cardioversion Broad spectrum antibiotics + antifungal Heparin, thrombolytics, antiplatelet agents If life-threatening, reverse anticoagulation and transfuse as needed. IV fluids to increase LV filling IV fluids and consider inotropes. Aspirin and heparin if AMI Requires surgical exploration Treat cardiogenic shock: IV fluids, vasopressors, ACLS protocols, consider heparin for thrombosis Cardiac Arrest Multiple potential causes ACLS algorithms except: including all those listed above • Chest compressions are controversial as they could dislodge the device. • Do NOT place defibrillation pads directly over device. • Assign one person to assess device placement during and after code. AMI: acute myocardial infarction; GI: gastrointestinal; LV: left ventricle; MAP: mean arterial pressure; PE: pulmonary embolism; ROSC: return of spontaneous circulation; RV: right ventricle; TIA: transient ischemic attack; VT: ventricular tachycardia; VF: ventricular fibrillation Updated 11/21/16 Updated 11/21/16 Left Ventricular Assist Device Team Based Learning individual Readiness Assessment Test (iRAT) 1. Which of the following is an INCORRECT method of assessing circulation in an LVAD patient? a. Using an arterial line to obtain mean arterial blood pressure (MAP) b. Auscultate and palpate the precordium, listening and feeling for a hum or vibration c. Checking a patient’s radial pulse d. Checking tissue perfusion (capillary refill, mental status, urine output, skin signs) e. Using a manual blood pressure cuff with doppler to measure mean arterial blood pressure (MAP) f. Using a manual blood pressure cuff with doppler to measure systolic and diastolic blood pressure (SBP and DBP) g. A&E h. C&F 2. What is an acceptable MAP in a patient with an LVAD? a. <60 mmHg b. 60-80 mmHg c. 80-110mm Hg d. >110 mmHg 3. Which of the following is an indication for cardiopulmonary resuscitation (CPR) in a patient with an LVAD? a. Absent pulses b. Loss of consciousness c. MAP < 60 mm Hg d. MAP = 0 mm Hg and pump stopped e. None of the above 4. A 65 yo LVAD patient presents with upper GI bleeding. Why is bleeding common in LVAD patients? a. b. c. d. e. Oral anticoagulant and anti-platelet use Acquired Von-Willebrand’s Disease Increased risk of AVM due to chronic low pulse pressure. Platelet dysfunction All of the above 5. You are monitoring an LVAD patient, who starts to become altered. Mean arterial pressure is measured as 50 mmHg. The patient’s capillary refill is 4 seconds. The controller alarm is flashing “low flow.” The cardiac monitor is shown below. What is your next step management? a. Check for battery power and line connection and contact the patient’s LVAD company. b. Check electrolytes (potassium, magnesium) and start amiodarone c. Synchronize cardioversion at 100 Joules d. Perform a 12 lead EKG and consult EP cardiologist to do a catheter ablation e. Defibrillation at 200 Joules 6.Your LVAD patient develops hypotension and the controller alarm flashes “low flow.” Match the following echo finding with their associated disease entities: Put each number in the appropriate box in the table below (more than one number can be in each box). 1. Pump not working or pump thrombosis 2. Significant AR (aortic regurgitation) 3. Hypovolemia/Bleeding 4. Massive PE 5. Right ventricular failure (MI) 6. Cardiac tamponade 7. Left Ventricular (LV) suction event RV size: Decrease LV size: Decrease LV size: No Change LV size: Increase RV size: No change RV size: Increase Left Ventricular Assist Device Team Based Learning group Readiness Assessment Test (gRAT) 1. Which of the following is an INCORRECT method of assessing circulation in an LVAD patient? a. b. c. d. e. f. g. Using an arterial line to obtain mean arterial blood pressure (MAP) Auscultate and palpate the precordium, listening and feeling for a hum or vibration Checking a patient’s radial pulse Checking tissue perfusion (capillary refill, mental status, urine output, skin signs) Using a manual blood pressure cuff with doppler to measure mean arterial blood pressure (MAP) Using a manual blood pressure cuff with doppler to measure systolic and diastolic blood pressure (SBP and DBP) A&E C&F 2. What is an acceptable MAP in a patient with an LVAD? a. c. d. <60 mmHg 60-80 mmHg 80-110mm Hg >110 mmHg 3. Which of the following is an indication for cardiopulmonary resuscitation (CPR) in a patient with an LVAD? a. b. c. e. Absent pulses Loss of consciousness MAP < 60 mm Hg MAP = 0 mm Hg and pump stopped None of the above 4. A 65 yo LVAD patient presents with upper GI bleeding. Why is bleeding common in LVAD patients? a. b. c. d. Oral anticoagulant and anti-platelet use Acquired Von-Willebrand’s Disease Increased risk of AVM due to chronic low pulse pressure Platelet dysfunction All of the above 5. You are monitoring an LVAD patient, who starts to become altered. Mean arterial pressure is measured as 50 mmHg. The patient’s capillary refill is 4 seconds. The controller alarm is flashing “low flow.” The cardiac monitor is shown below. What is your next step management? a. b. d. e. Check for battery power and line connection and contact the patient’s LVAD c company. Check electrolytes (potassium, magnesium) and start amiodarone Synchronize cardioversion at 100 Joules Perform a 12 lead EKG and consult EP cardiologist to do a catheter ablation Defibrillation at 200 Joules 6. Your LVAD patient develops hypotension and the controller alarm flashes “low flow.” (Matching) Put each number in the appropriate box in the table below (more than one number can be in each box). Match the following echo finding with their associated disease entities: 1. 2. 3. 4. 5. 6. 7. Pump not working or pump thrombosis Significant AR (aortic regurgitation) Hypovolemia/Bleeding Massive PE Right ventricular failure (MI) Cardiac tamponade Left Ventricular (LV) suction event LV size: Decrease RV size: Decrease RV size: No change RV size: Increase 3,6,7 3,7 4,5 LV size: No Change LV size: Increase 4,5 1,2 RAT Key: Please insert and attach your RAT Key, please use page breaks to keep gRAT on its own page. 1. Which of the following is an INCORRECT method of assessing circulation in an LVAD patient? Answer: H: Continuous flow LVAD (CF-LVAD) devices are the most widely used LVAD devices.4 Patients, therefore, may have diminished or absent pulses. Similarly, because flow is not pulsatile, measuring systolic and diastolic blood pressures is not applicable. 2. What is an acceptable MAP in a patient with an LVAD? Answer B. 60-80 mmHg According to Feldman,5 patients with a CF-LVAD should have a mean blood pressure less than 80 mm Hg and [greater than 60]. 3. Which of the following is an indication for cardiopulmonary resuscitation (CPR) in a patient with an LVAD? Answer D. MAP = 0 mm Hg and pump stopped is an indication for CPR. Fluid bolus and device optimization should be attempted in patients with a low MAP. Absent pulses are common in patients with continuous flow LVADs. Patients who are unconscious do not necessarily need CPR. Cardiopulmonary resuscitation puts patients at risk for device dislodgment. 4. A 65 yo LVAD patient presents with upper GI bleeding. Why is bleeding common in LVAD patients? Answer E. All of the above: Patients with LVADs take oral anticoagulants and antiplatelet agents. They have acquired Von-Willebrand’s disease from the shear stress of CF-LVADs may cause proteolysis on von Willebrand’s factor.6,7 Patients are also at risk of arteriovenous malformations due to chronic low pulse pressure. 5. You are monitoring an LVAD patient, who starts to become altered. Mean arterial pressure is measured as 50 mmHg. The patient’s capillary refill is 4 seconds. The controller alarm is flashing “low flow.” The cardiac monitor is shown below. What is your next step management? Answer: C: Synchronize cardioversion at 100 Joules. The patient is unstable and therefore not a candidate for IV anti-arrhythmics alone. The patient has a MAP of 50mmHg, so therefore can be cardioverted, rather than defibrillated. 6.Your LVAD patient develops hypotension and the controller alarm flashes “low flow.” (Matching) Put each number in the appropriate box in the table below (more than one number can be in each box). Match the following echo finding with their associated disease entities: RV size: Decrease LV size: Decrease 3,6,7 RV size: No change 3,7 LV size: No Change LV size: Increase RV size: Increase 4,5 4,5 1,2 Left Ventricular Assist Device Team Based Learning Group Application Exercise (GAE) A 50 yr old female with history of DM and ischemic cardiomyopathy status post LVAD (Heartmate II) for bridge to heart transplant two week ago presents after collapsing at her routine follow up appointment, 5 minutes prior to arrival. 1. What is your differential diagnosis? 2. How will you assess her perfusion after you manage her airway and breathing? 3. From your answer to #2, you decide that the LVAD is not working. What are your next steps? 4. You fix the issue in #3, and feel the LVAD is working, but the alarm is going off and the MAP is <60. What are your next steps? 5. The machine is hot and the Echo shows normal RV size but dilate LV. What is the possible cause? 6. How to investigate and manage the diagnosis in #5? 7. What is the definitive therapy for pump failure? 8. What is the definitive therapy for significant Aortic Regurgitation? Left Ventricular Assist Device Team Based Learning Group Application Exercise (GAE): Key Case: A 50 yr old female with history of DM and ischemic cardiomyopathy status post LVAD (Heartmate II) for bridge to heart transplant two week ago presents after collapsing at her routine follow up appointment, 5 minutes prior to arrival. 1. What is your differential diagnosis? Acute stroke, intracranial hemorrhage, cardiac arrest, pump failure or thrombosis, cardiac tamponade, massive PE, dysrhythmia, hypoglycemia, severe active bleeding, pneumothorax, aortic dissection, sepsis, acidosis 2. How will you assess her perfusion after you manage her airway and breathing? -Listen for hum over precordium -Feel vibration over precordium -Doppler MAP -Skin signs -Assess mental status 3. From your answer to #2, you decide that the LVAD is not working. What are your next steps? -Contact LVAD team coordinator -Check batteries -Plug in LVAD in -Check connections -Make sure drive line is connected -Check alarms, what are alarms saying? 4. You fix the issue in #3, and feel the LVAD is working, but the alarm is going off and the MAP is <60. What are your next steps? -Echo, EKG, cardiac monitor, fluid bolus, IV access, labs, ABG -Check which alarms are going off (Is there low flow? Is the machine hot?) 5. The machine is hot and the echo shows a normal RV size but dilated LV. What is the possible cause? -Pump thrombosis, see table 4b in Stainback, et al6 -Pump malfunction of mechanical component -Significant Aortic regurgitation 6. How to investigate and manage the diagnosis in #5? - Consult cardiologist or contact LVAD team coordinator - Compare echo with previous echo - Clinical features associated with pump thrombosis include: intravascular hemolysis (Hemoglobinuria, elevated creatinine, total billirubin and elevated LDH), high power alarm, Hot device - Check prothrombin time (PT)/Partial thromboplastin time (PTT)/International normalized ratio (INR), complete blood count, lactate dehydrogenase, liver function tests, creatinine, urinalysis -Goal INR depends on the device and ranges from 2.0 to 3.5. 7. What is the definitive therapy for pump failure? -Tissue plasminogen activator (TPA) -Heparin 8. What is the definitive therapy for significant Aortic Regurgitation? -Bioprosthetic valve -Heart transplant