* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Myocardial Perfusion SPECT: Current Concepts
Saturated fat and cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Echocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
MEDICINE
REVIEW ARTICLE
Myocardial Perfusion SPECT:
Current Concepts
Oliver Lindner, Herbert Rusche, Michael Schäfers,
Otmar Schober, Wolfgang Burchert
SUMMARY
Introduction: Myocardial perfusion SPECT has made considerable progress in recent years, both
in terms of methodology and of clinical applications. Methods: Selective literature review.
Results: In patients with suspected or known CAD prognostic studies support the use of myocardial
perfusion imaging in stratifying patients by prognosis and management approaches. The number
and severity of perfusion disturbances on scintigraphy relate closely to the frequency of cardiac
death and nonfatal myocardial infarction. The use of a stepwise diagnostic algorithm for CAD
allows individualized stratification by risk and prognosis. In addition, the scintigraphic result can
be integrated into decision making around risk factor management, medical therapy and
revascularization. Discussion: In patients with suspected to advanced coronary artery disease
myocardial perfusion SPECT allows reliable identification of low and high risk patients. Normal
perfusion scans with no perfusion disturbances are in general associated with a low cardiac
event rate.
Dtsch Arztebl 2007; 104(14): A 952–8.
Key words: myocardial perfusion szintigraphy, coronary artery disease, cardiological diagnosis,
SPECT, revascularization
C
ardiovascular diseases are the most common cause of death in Western industrialized
countries. Timely diagnosis of coronary artery disease (CAD) is the decisive factor
influencing the course of the illness and its prognosis. It is, therefore, important to identify
patients with CAD and to initiate effective treatment (risk factor modification, pharmacotherapy, interventional or operative myocardial revascularization) based on prognosisoriented decision processes. Stress electrocardiography (ECG) is the most important initial
component of the diagnostic algorithm for patients suspected of having CAD (1, 2). Depending
on the ECG findings, imaging studies may be performed afterward. The type of imaging
study that is most commonly used is myocardial perfusion scintigraphy (MPS). In
Germany, in the year 2003, MPS was performed 194,084 times and stress ECG was
performed 173,031 times within the framework of care reimbursed by the governmentally
mandated health insurance companies (3).
This article will discuss the current diagnostic and prognostic value of MPS and explain
how its findings can be integrated into the therapeutic decision-making process.
Myocardial perfusion scintigraphy: principles
MPS reveals the effect of arterial stenoses on myocardial perfusion and thereby indicates
the presence of hemodynamically relevant coronary artery stenoses. It employs
radiopharmaceuticals that are taken up by myocardial tissue in an amount depending on the
state of tissue perfusion. If coronary stenosis is present, stress testing reveals less uptake of
the radiopharmaceutical in the myocardial wall supplied by the stenotic vessel than in other,
normally perfused myocardial segments. Testing at rest, in contrast, reveals no regional
differences in tracer uptake, because the stenosis does not impair perfusion at rest. The
related imaging study employs a tomographic technique (as in CT or MRI) and is called
myocardial SPECT ("single photon emission computerized tomography").
MPS is performed either with 201Tl (thallium) or with 99mTc (technetium) tracers
(Sestamibi or Tetrofosmin). The various tracer substances used do not differ fundamentally
Herz- und Diabeteszentrum NRW, Universitätsklinik der Ruhr-Universität Bochum, Institut für Radiologie, Nuklearmedizin und
Molekulare Bildgebung, Bad Oeynhausen: Dr. med. Lindner, Prof. Dr. med. Burchert; Universitätsklinik der Ruhr-Universität
Bochum, Abteilung für Allgemeinmedizin: Prof. Dr. med. Rusche, Westfälische Wilhelms-Universität, Münster,Klinik und Poliklinik
für Nuklearmedizin: Prof. Dr. med. Dr. rer. nat. Schober, Prof. Dr. med. Schäfers
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
1
MEDICINE
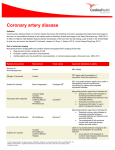
TABLE
The diagnostic accuracy of non-invasive studies for the demonstration of CHD
Studies
(number)
Patients
(number)
Sensitivity
%
Specificity
%
147
24,074
68 (23–100)
77 (17–100)
Ergometric
33
4,480
87 (71–97)
73 (47–100)
Pharmacological
17
2,465
89 (72–93)
75 (28–100)
Stress ECG1 (e2)
Myocardial
scintigraphy2
(12)
Stress echocardiography2 (e3)
Ergometric
33
3,480
86 (71–97)
81 (64–100)
Pharmacological (dobutamine)
37
3,280
82 (54–98)
84 (44–100)
Myocardial perfusion MRI2 (e4)
11
254
80 (65–92)
85 (75–100)
1 According
to the most recent metaanalysis, cf. Refs. (2, 12, 13);
2 Pooled data;
sensitivity and specificity as weighted averages, confidence range in parentheses.
The reference in each case was the demonstration of a >50% stenosis by coronary angiography.
The studies included no correction for referral bias and thus presumably overestimated sensitivity and underestimated specificity,
because an abnormal test often leads to referral for performance of coronary angiography, while a normal test only rarely does (e5).
in their clinical utility (4, 5). The radiation exposure to a patient undergoing MPS with
99mTc perfusion tracers in a single-day protocol is 8.5 mSv (assuming that the patient weighs
70 kg and that the applied amount of radioactivity is 250 MBq for stress testing and
750 MBq for testing at rest); this quantity can be reduced to 4.3 mSv with the use of a 2-day
protocol (70-kg patient, applied radioactivity 250 MBq both for stress testing and for
testing at rest) (6, 7). For comparison, the annual natural radiation exposure in Germany is
2 to 4 mSv, and the effective radiation dose from a chest CT is 6 to 10 mSv (8).
Stress testing
Stress testing in myocardial perfusion can be performed either ergometrically or
pharmacologically. In ergometric testing, the oxygen consumption of the myocardium is
increased, and an increase in perfusion results; this increase is found to be deficient if a 50%
to 75% coronary artery stenosis is present (diminished coronary reserve). In order to
demonstrate hemodynamically relevant stenoses reliably, the patient should be at least
submaximally stressed so that the heart rate equals or exceeds 0.85 × (220 - age in years).
If this is not possible, myocardial perfusion can also be increased directly, i.e.,
independently of the patient's cooperation, with the coronary vasodilator adenosine.
Adenosine produces coronary vasodilatation, which is followed by a reflex increase of the
heart rate by ca. 10% and a slight drop in blood pressure. It has a plasma half-life of less
than two seconds; thus, its effect is short-lived and easily controlled. Alternatively, the
β1-agonist dobutamine can also be used to increase myocardial perfusion. This drug is a
catecholamine derivative and may therefore cause supraventricular and ventricular
arrhythmias. Stress testing with dobutamine is used in patients who cannot be stressed
ergometrically and in whom adenosine is contraindicated (e.g., because of manifest
obstructive pulmonary disease, theophylline use, or second-degree atrioventricular block)
(4). Serious side effects such as high-grade arrhythmias, infarction or death are rare in
ergometric or pharmacological stress tests, with a frequency of ca. 1 in 10,000 patients (9).
With the use of these different procedures, an adequate increase of myocardial perfusion
can be achieved in nearly every patient undergoing testing. Even patients who are in poor
physical condition, obese patients, and those who cannot be mobilized because of concomitant
orthopedic, neurological, or other diseases can be adequately tested with myocardial
scintigraphy, even when they are physically incapable of being stressed to the degree that
would otherwise be required.
Functional analysis – "gated SPECT"
Gated SPECT is an extension of myocardial SPECT using a technique that can be thought
of as analogous to a "flip-book": each heartbeat is divided into 8 intervals on the basis of the
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
2
MEDICINE
DIAGRAM 1
Left: summed stress score (SSS) and summed rest score (SRS) in a high-risk MPS with ischemia in the anterior wall, the cardiac apex, and the
septum. The summed difference score (SDS) is 31 (SSS minus SRS). Right: representative sections.
ECG wave. Each interval is pictorially displayed and analyzed. Gated SPECT thus yields
information not only on overall perfusion, but also on left-ventricular functional parameters
such as end-diastolic and end-systolic volume and left ventricular ejection fraction (LVEF).
These measurements are made during testing at rest and also after stress testing. There is
normally no difference between resting LVEF and post-stress LVEF, because both
measurements are made with a gamma camera while the patient is at rest. If ischemia is
present, however, the post-stress LVEF may be lower than resting LVEF because of
"myocardial stunning": at the time of data acquisition, the myocardium has not yet
recovered from the ischemia that it suffered during stress testing, and ischemic ventricular
dysfunction is still present. Thus, a greater than 5% difference between resting LVEF and
post-stress LVEF provides further evidence of ischemia (10).
Diagnostic accuracy of myocardial scintigraphy
Coronary angiography is usually taken as a standard of reference for the characterization of
imaging techniques for the diagnosis of CAD; thus, the results of functional tests are
generally compared with coronary morphology as revealed by angiography. Stress
echocardiography and myocardial perfusion scintigraphy are established procedures whose
sensitivity and specificity for the diagnosis of CAD are considered to be equivalent (table);
beyond these techniques, there are also newer ones such as dobutamine stress MRI and
myocardial perfusion MRI with adenosine or dipyridamole. The sensitivities and specificities
of the currently available non-invasive techniques, as compared to invasive coronary
angiography, are listed in the table. There have not been any studies to date in which these
techniques were directly compared with one another.
Sensitivity and specificity are not fully adequate parameters to characterize the quality
(usefulness) of a diagnostic test. The nature of patient recruitment ("referral bias") leads to
an overestimation of sensitivity and an underestimation of specificity. The so-called
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
3
MEDICINE
"normalcy rate" is a further parameter characterizing the reliability of MPS in a normal
collective of individuals and thus no longer places it in a head-to-head comparison with
coronary angiography (11). The normalcy rate is defined as the percentage of patients with
a low probability of coronary heart disease (i.e., no more than 10%) whose MPS is normal;
it was found to be 91% (12).
Indications for MPS and other procedures
The German national care guidelines (nationale Versorgungsleitlinie, NVL) for chronic
CAD recommend the use of an ergometric or pharmacological stress test with imaging
(MPS, stress echocardiography, or cardiac MRI) in the following situations (1, 2):
> if chronic CAD is suspected with an intermediate pre-test probability:
– if the ST segments cannot be reliably judged on the resting ECG because of left
ventricular hypertrophy, Wolff-Parkinson-White syndrome, digitalis use, left bundle
branch block, or a pacemaker ECG,
– in patients who cannot be adequately stressed so that relevant findings can be obtained
on a stress ECG (i.e., patients whose heart rate cannot be raised to 85% of the agerelated maximum), or
– if ergometry does not yield conclusive findings.
> in known CAD (in addition to the indications described above):
– if the patient's symptoms and physical findings have changed but the patient cannot
be adequately stressed to yield relevant findings on a stress ECG, or
– as an alternative to a stress ECG in patients who, despite treatment, become
symptomatic again after an asymptomatic interval, and in whom the localization of
ischemia and the functional relevance of a stenosis and/or myocardial vitality is of
clinical importance.
The NVL state that MPS is indicated above all other tests if the patient has an intermediate
pre-test probability of CAD (10% to 90%) as well as a pacemaker ECG or left bundle
branch block. In all of the other situations mentioned, no particular type of imaging study
is preferred over the others (1, 2).
Interpretation of findings and prognosis
If the pre-test probability of CAD is in the intermediate range (10% to 90%), a pathological
finding on an imaging study confirms the suspicion of CAD, while a normal finding largely
excludes functionally relevant CAD. Moreover, nuclear medical tests yield important
prognostic information. Data on the prognostic value of stress echocardiography and MRI
are limited (1).
If non-invasive imaging yields abnormal findings, the German national care guidelines,
like the American guidelines, recommend that diagnostic coronary angiography be performed
(1, 2, 13). In cardiac imaging as elsewhere in medicine, however, the transition from normal
DIAGRAM 2
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
The frequency of cardiac events
depending on the degree of
hypoperfusion, after (14);
SSS, summed stress score;
MPS, myocardial perfusion scintigraphy.
From: Circulation 1999; 98:190, with
the kind permission of Lippincott,
Williams and Wilkins.
4
MEDICINE
to pathological findings is fluid. In the case of myocardial perfusion scintigraphy, the
diagnostic terms "normal," "borderline pathological," and "pathological" were defined in
past years by extensive studies, with cardiac risk as the underlying conceptual basis.
Cardiac risk is said to be low if the cardiac mortality is less than 1% per year (a comparable
risk to that of the general population), and high if it exceeds 3% per year (12, 13).
Quantitative perfusion scores derived from myocardial perfusion scintigraphy can be
used to create a pictorial representation of cardiac risks and prognosis. The left ventricular
myocardium is represented on a circular disk (polar tomogram) (diagram 1). This procedure may be compared to pressing the petals of a flower. The myocardial apex is found in the
center of the polar tomogram, while the basal myocardial segments occupy its periphery.
The upper quarter of the tomogram represents the anterior wall, its right quarter the lateral
wall, its lower quarter the posterior wall, and its left quarter the septum. A score is calculated
by dividing the myocardium into 20 segments, grading the tracer uptake in each segment on
a scale of 0 (normal) to 4 (markedly reduced), and adding up the scores from all segments
(diagram 1). The value obtained during stress testing is called the summed stress score
(SSS), while that obtained during testing at rest is called the summed rest score (SRS). The
SRS is a measure of already infarcted myocardium, while the SSS reflects reduced perfusion
of either reversible (ischemic) or irreversible cause (already infarcted myocardium). The
difference between the two, called the summed difference score (SDS), is thus a measure of
reversible (ischemic) hypoperfusion.
Diagram 2 shows the frequency of cardiac events (cardiac death and nonfatal myocardial
infarction) as a function of the SSS calculated from MPS, as well as the resulting estimation
of risks in 5,183 patients with suspected or known CAD over a period of observation of
ca. 2 years (14). The following may be observed:
> a normal finding (SSS < 4) on stress MPS is associated with a low rate of cardiac
events, i.e., a rate that is comparable to that of the normal population;
> as the SSS increases, the frequency of cardiac events increases;
DIAGRAM 3
Risk stratification with myocardial perfusion scintigraphy (MPS) depending on the pre-test estimation of cardiac risk and the stage of CAD.
Independently of the pre-test risk, MPS with significant hypoperfusion ("high-risk MPS," red diamonds) is associated with a higher
frequency of cardiac events than MPS with mild or no hypoperfusion ("low-risk MPS," blue squares). Patients can be segregated in this
way into high- and low-risk groups. For example, a patient with advanced CAD and a pre-test expected frequency of cardiac events
(cardiac death or nonfatal myocardial infarction) of 4% per year who is then found to have a high-risk MPS can be assigned an event
probability of ca. 5% per year; the same patient, if found to have a low-risk MPS, can be assigned an event probability of 2% per year (11).
From: J Nucl Cardiol 2004; 11: 171–85, with the kind permission of Elsevier.
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
5
MEDICINE
> the stress MPS reveals mild hypoperfusion (borderline findings with 4 SSS < 9),
then nonfatal infarctions will occur more frequently than fatal cardiac events.
A metaanalysis of 39 studies involving a total of 69,655 patients revealed that a normal
MPS (low-risk MPS, SSS < 4) is associated with a rate of cardiac events (cardiac death and
nonfatal infarction) of 0.85% per year, while a pathological MPS (high-risk MPS, SSS 9)
is associated with a rate of cardiac events of 5.9% per year. If one stratifies the currently
available study data by the degree of severity of CAD, and thus by the varying probability
of cardiac events (diagram 3), one finds that:
> MPS is able to distinguish high- from low-risk patients over the entire spectrum of
CAD;
> the rate of cardiac events in persons with a pathological (high-risk) MPS increases
with increasing severity of CAD;
> the frequency of cardiac events in persons with a normal (low-risk) MPS is nearly
always below 2% per year, regardless of the stage of CAD that is present, i.e., even in
patients with three-vessel disease (11, 12, 15).
In summary, the number and extent of disturbances of perfusion that are revealed by
MPS provide a good means of estimating the risk of future cardiac events (2).
If the results of functional analysis (gated SPECT), with LVEF as the most important
parameter, are considered in addition, then still more refined prognostic statements can be
made. The LVEF value used here is the one obtained by post-stress measurement, i.e., ca.
60 minutes after ergometric or pharmacological stress. A longitudinal study with a follow-up
interval of 1.5 years showed that patients with an LVEF of 45% or more had an annual
mortality below 1% regardless of the presence or absence of hypoperfusion, while those
with an LVEF below 45% had a markedly higher mortality. LVEF was found to be the best
predictor of cardiac death, while hypoperfusion was found to be the best predictor of
nonfatal myocardial infarction (16, 17).
Myocardial infarction is mainly due to the rupture of atherosclerotic plaques that, before
rupture, caused less than 50% stenosis of the vessel in which they were located, and were
thus hemodynamically insignificant (18, 19). MPS is generally able to detect only
hemodynamically significant stenoses; thus, one may well ask why a normal MPS is
associated with a low rate of myocardial infarction and a pathological MPS with a higher
rate of myocardial infarction. The answer is that hemodynamically significant stenoses
cannot be considered in isolation but are rather the "tip of the iceberg," i.e., they represent
only one aspect of the overall pathological condition of the cardiovascular system.
Hypoperfusion detected by MPS is an indicator of coronary artery disease. Moreover, even
if angiographically demonstrable coronary artery stenosis is absent, MPS may nevertheless
demonstrate stress-related hypoperfusion on the basis of endothelial dysfunction, providing
a further indication of a diseased coronary arterial system (20, 21). The valid fundamental
principle is as follows: MPS is a safe way to identify patients at risk. The lesion that leads
to infarction cannot, however, be detected with the current non-invasive techniques (12).
Evaluation of findings
On the basis of the concept described above, the findings of MPS can be used for further
diagnostic and therapeutic decision-making. It should be remembered that the mortality
rates for cardiovascular procedures such as percutaneous transluminal catheter angioplasty
(PTCA) or coronary artery bypass grafting (CABG) are 1% (12, 22, 23). The current
state of scientific evidence justifies using the degree of cardiac risk predicted by the MPS
(low, middle, or high) in the following ways as an aid to decision-making in a stratified
diagnostic scheme:
> If the MPS is normal (low-risk), then the rate of cardiac events is less than 1% per year
and is thus comparable both to the cardiac risk of the general population and lower than
the risk of an invasive cardiovascular procedure. Thus, if the MPS is normal, the
recommended clinical intervention is optimal management of all cardiovascular risk
factors that are present. Further diagnostic studies are not required (13).
> If the MPS reveals mild hypoperfusion (intermediate cardiac risk), then the risk of
cardiac death is still under 1%, but the risk of a nonfatal infarction is relatively high. In
this group of patients, the risk of death from a cardiovascular intervention is still higher
than the cardiac mortality, so the proper therapeutic approach is, once again, optimal
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
6
MEDICINE
DIAGRAM 4
Estimation of the risk of cardiac death
after medical treatment or
revascularization in relation to the extent
of myocardial hypoperfusion, measured
as SDS (the "summed difference
score"). If the SDS is higher than 8 (to
10), then revascularization procedures
confer a more favorable prognosis than
medical treatment alone (25).
From: Circulation 2003; 1007: 2900–7,
with the kind permission of Lippincott,
Williams and Wilkins.
medical management with minimization of all risk factors. An analysis of 10,627
patients reveals that this strategy is to be recommended for patients with an SDS up to
8 (diagram 4). If angina pectoris is a prominent complaint, however, a coronary
intervention may be indicated; in such cases, the prognostic aspect (with reference to
death or myocardial infarction) is not the primary concern (25, e1).
> If the MPS reveals moderate or severe hypoperfusion (high cardiac risk), then the risk
of cardiac death is high. In such cases, the MPS is considered unequivocally pathological.
As recommended by the German national guidelines, the patient should undergo
diagnostic coronary angiography with the goal of revascularization. In this situation, the
prognostic utility of revascularization is greater than that of medical treatment
(diagram 4). The same is true if the LVEF is below 45%, even if the associated
hypoperfusion is only mild (14, 16, 25).
Summary
MPS is clearly superior to competing non-invasive techniques with respect to the level of
scientific evidence available from current studies on the prognosis and treatment of
coronary heart disease (2). This explains why MPS has been a well-established technique
in the English-speaking countries for many years. It is widely used as part of a guidelineoriented, stratified diagnostic algorithm after a stress ECG has been performed, or if the
ECG cannot be properly interpreted, whenever the presence of coronary heart disease is
known or suspected. A further advantage of MPS is that myocardial perfusion scintigraphy
with pharmacologically induced myocardial stress can be performed even in patients who
cannot be ergometrically stressed to the extent required for adequate diagnostic information
to be obtained.
Conflict of Interest Statement
Dr. Lindner has received honoraria and/or reimbursement of travel costs from Bristol Myers Squibb, Phillips, and Aventis. He was
temporarily employed by GE Healthcare and collaborated on a multicenter study by GE Healthcare. Prof. Burchert participated in
multicenter studies by GE Healthcare and has received reimbursement of travel costs and lecture honoraria from this company.
He has received reimbursement of travel costs and/or honoraria from Bristol Myers Squibb, Siemens, Phillips, and SanofiSynthelabo. Prof. Rusche, Prof. Schäfers, and Prof. Schober state that they have no conflict of interest as defined by the
Guidelines of the International Committee of Medical Journal Editors.
Manuscript received on 12 October 2005; final version accepted on 18 September 2006.
Translated from the original German by Ethan Taub, M.D.
REFERENCES
For e-references please refer to the additional references listed below.
1. Bundesärztekammer, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften,
Kassenärztliche Bundesvereinigung: Nationale Versorgungs-Leitlinie Chronische KHK (Kurzfassung). Mai
2006; Version 1.1., www.versorgungsleitlinien. de/themen/khk/pdf/nvl_khk_kurz.pdf
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
7
MEDICINE
2. Bundesärztekammer, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften,
Kassenärztliche Bundesvereinigung: Nationale Versorgungs-Leitlinie Chronische KHK (Langfassung).
11. Februar 2006. www.versorgungsleitlinien.de/ themen/khk/pdf/nvl_khk_lang.pdf
3. Bruckenberger E: Herzbericht 2004 mit Transplantationschirurgie; 2005. Selbstverlag, Hannover,
Hitzackerweg 1a.
4. Heller GV: Tracer selection with different stress modalities based on tracer kinetics. J Nucl Cardiol 1996; 3:
S15–21.
5. Kapur A, Latus KA, Davies G, et al.: A comparison of three radionuclide myocardial perfusion tracers in
clinical practice: the ROBUST study. Eur J Nucl Med Mol Imaging 2002; 29: 1608–16.
6. ICRP Publication 62: Radiological protection in biomedical research. Annals of the ICRP Vol. 22/4, Pergamon
Press; 1993.
7. ICRP Publication 80: Radiological protection in biomedical research. Annals of the ICRP Vol 28/3, Pergamon
Press; 1998.
8. Bundesamt für Strahlenschutz: Röntgendiagnostik – schädlich oder nützlich? 2006.
www.bfs.de/www/extfs/bfs/druck/strah lenthemen/STTH_Roentgen.pdf
9. Cerqueira MD: Pharmacologic stress versus maximal-exercise stress for perfusion imaging: which, when,
and why? J Nucl Cardiol 1996; 3: S10–4.
10. Paul AK, Hasegawa S, Yoshioka J et al.: Exercise-induced stunning continues for at least one hour: evaluation with
quantitative gated single-photon emission tomography. Eur J Nucl Med 1999; 26: 410–5.
11. Shaw LJ, Iskandrian AE: Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004; 11:
171–85.
12. Klocke FJ, Baird MG, Lorell BH et al.: ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide
imaging – executive summary: a report of the American College of Cardiology/American Heart Association
Task Force on Practice Guidelines. 2003; American College of Cardiology Web site. www.acc.org/clinical/
guidelines/radio/index.pdf
13. Gibbons RJ, Abrams J, Chatterjee K et al.: ACC/AHA 2002 guideline update for the management of patients
with chronic stable angina – summary article: a report of the American College of Cardiology/American Heart
Association Task Force on practice guidelines (Committee on the Management of Patients With
Chronic Stable Angina). 2003; American College of Cardiology. www.acc.org/clinical/guidelines/stable/
stable_clean.pdf.
14. Hachamovitch R, Berman DS, Shaw LJ et al.: Incremental prognostic value of myocardial perfusion single
photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of
cardiac death and myocardial infarction. Circulation 1998; 97: 535–43.
15. Abdel Fattah A, Kamal AM, Pancholy S et al.: Prognostic implications of normal exercise tomographic thallium
images in patients with angiographic evidence of significant coronary artery disease. Am J Cardiol 1994; 74:
769–71.
16. Sharir T, Germano G, Kavanagh PB et al.: Incremental prognostic value of post-stress left ventricular ejection
fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation
1999; 100: 1035–42.
17. Sharir T, Germano G, Kang X et al.: Prediction of myocardial infarction versus cardiac death by gated myocardial
perfusion SPECT: risk stratification by the amount of stress-induced ischemia and the poststress ejection
fraction. J Nucl Med 2001; 42: 831–7.
18. Falk E, Shah PK, Fuster V: Coronary plaque disruption. Circulation 1995; 92: 657–71.
19. Naghavi M, Libby P, Falk E et al.: From vulnerable plaque to vulnerable patient: a call for new definitions and
risk assessment strategies: Part I. Circulation 2003; 108: 1664–72.
20. Hasdai D, Gibbons RJ, Holmes DR Jr., Higano ST, Lerman A: Coronary endothelial dysfunction in humans is
associated with myocardial perfusion defects. Circulation 1997; 96: 3390–5.
21. Zeiher AM, Krause T, Schachinger V, Minners J, Moser E: Impaired endothelium-dependent vasodilation of
coronary resistance vessels is associated with exercise-induced myocardial ischemia. Circulation 1995; 91:
2345–52.
22. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. The Bypass
Angioplasty Revascularization Investigation (BARI) Investigators. N Engl J Med 1996; 335: 217–25.
23. Pompa JJ, Kuntz RE, Baim DS: Percutaneous coronary and valvular intervention. In: Zipes DP, Libby P, Bonow
RO, Braunwald E, eds. Braunwald's Heart Disease. Philadelphia: Elsevier Saunders; 2005: 1367–98.
24. Hachamovitch R, Berman DS: The use of nuclear cardiology in clinical decision making. Semin Nucl Med
2005; 35: 62–72.
25. Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS: Comparison of the short-term survival benefit
associated with revascularization compared with medical therapy in patients with no prior coronary artery
disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation
2003; 107: 2900–7.
ADDITIONAL REFERENCES
e1. Katritsis DG, Ioannidis JP: Percutaneous coronary intervention versus conservative therapy in nonacute coronary
artery disease: a meta-analysis. Circulation 2005; 111: 2906–12.
e2. Gianrossi R, Detrano R, Mulvihill D et al.: Exercise-induced ST depression in the diagnosis of coronary artery
disease. A meta-analysis. Circulation 1989; 80: 87–98.
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
8
MEDICINE
e3. Cheitlin MD, Armstrong WF, Aurigemma GP et al.: ACC/AHA/ASE 2003 guideline update for the clinical application
of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association
Task Force on Practice Guidelines. 2003; American College of Cardiology www.acc.org/clinical/guide
lines/echo/index_clean.pdf
e4. Wilke NM, Jerosch-Herold M, Zenovich A, Stillman AE: Magnetic resonance first-pass myocardial perfusion
imaging: clinical validation and future applications. J Magn Reson Imaging 1999; 10: 676–5.
e5. Lindner O, Fricke E, Preuss R et al.: Nicht-invasive Diagnostik der KHK bei Diabetes mellitus. Diabetes,
Stoffwechsel und Herz 2006; 15: 33–43.
Corresponding author
Dr. med. Oliver Lindner
Institute for Radiology, Nuclear Medicine, and Molecular Imaging
Heart and Diabetes Center NRW
University Clinic of the Ruhr - University of Bochum
Georgstr. 11
D-32545 Bad Oeynhausen, Germany
[email protected]
Dtsch Arztebl 2007; 104(14): A 952–8 ⏐ www.aerzteblatt.de
9