* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download msb200922-sup
Magnesium transporter wikipedia , lookup
Biosynthesis wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Isotopic labeling wikipedia , lookup
Natural product wikipedia , lookup
Biomarker (medicine) wikipedia , lookup
Specialized pro-resolving mediators wikipedia , lookup
Metabolic network modelling wikipedia , lookup
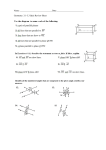
Predicting Metabolic Biomarkers of Human Inborn Errors of Metabolism Supplementary Information Tomer Shlomi1†, Moran N. Cabili2†, Eytan Ruppin2, 3 1 Department of Computer Science, Technion – Israel Institute of Technology, Haifa 32000, Israel 2 School of Computer Science, Tel-Aviv University, Tel-Aviv 69978, Israel 3 School of Medicine, Tel-Aviv University, Tel-Aviv 69978, Israel † These authors contributed equally to this work Table of Content Supplementary Figure 1 An illustrative example of biomarker's extra-cellular concentration change prediction……………………………………………………………………………….. Supplementary Figure 2 Distribution of biomarkers in different biofluids according to HMDB ……………….. Supplementary Figure 3 Illustration of the effect of Tyrosinemia type I, type III and Alkaptonuria on the metabolism and transport of tyrosine…………………………………………………... Supplementary Figure 4 Illustration of the effect of Methylmalonate semialdehyde dehydrogenase deficiency on the metabolism and transport of its known biomarkers…………………………….. Supplementary Table 1 Full names of the metabolites presented in main-text figure 3………………………… Supplementary Table 2 Full names of the metabolites presented in supplementary figure 3…………………… Supplementary Table 3 Full names of the metabolites presented in supplementary figure 4…………………… 2 3 4 5 6 7 8 1 Supplementary Figure 1: An illustrative example of the computed flux distributions underlying the predicted reduction in the extra-cellular concentration of biomarker M6. Circular nodes represent metabolites, solid arrows represent reactions, and dashed lines represent the network boundaries. The disease causing reaction is marked with a red cross. A predicted steady-state flux distribution is colored orange. (a) A flux distribution describing the maximal flux value of V6 in the healthy state. M5 is converted to M6 and 2 some of M6 is secreted from the cell. (b) A flux distribution describing the minimal flux value of V6 in the healthy state. (c) A flux distribution describing the maximal flux value of V6 in the disease state. (d) A flux distribution describing the minimal flux value of V6 in the disease state. Supplementary Figure 2: Number of predicted biomarkers in disorders that can be found in different biofluids according to HMDB (data is available for 137 out of 223 biomarkers predicted in total). According to HMDB the biomarkers are classified to different metabolic sub-classes that are shown in stack. Metabolites that were classified to other metabolic sub-classes or those for which no classification was available are classified as 'other'. 3 Supplementary Figure 3: A sub-network that illustrates the effect of Tyrosinemia type I, type III and Alkaptonuria (OMIM 276700, 276710, 203500, respectively) on the metabolism and transport of tyrosine (tyr). Circular nodes represent metabolites and edges represent biochemical reactions. For simplicity, only abbreviations of metabolite names and enzyme E.C. (Enzyme Commission) numbers are specified (explicit names are given in Supp. Table 2). Metabolites marked in green participate in other reactions that are not presented here, for simplicity. Tyrosinemia type III, Alkaptonuria, and Tyrosinemia type I are caused by dysfunctional HPD, HGD, and FAH, respectively. As shown, tyrosine can be degraded via 5 different pathways. Interestingly though, our method correctly predicts that the extra-cellular concentration of tyrosine would increase in all aforementioned disorders, though a visual inspection of the network topology may incorrectly suggest otherwise (i.e. that the alternative pathways would fully compensate for the dysfunctional enzymes and maintain the same uptake rate of tyrosine in a disease case). 4 Supplementary Figure 4: A sub-network that illustrates the effect of Methylmalonate semialdehyde dehydrogenase deficiency (OMIM 603178) on the metabolism and transport of valine (val), beta-alanine (ala_B), 3-hydroxypropionic acid (3hpp), 3aminoisobutyric acid (3aib) and 3-hydroxyisobutyric acid (3hmp). Circular nodes represent metabolites, full edges represent biochemical reactions and a dashed edge represents a biochemical pathway. Metabolites marked in green participate in other reactions that are not presented here for simplicity. Only abbreviations of metabolite names and enzyme E.C. (Enzyme Commission) numbers are specified (explicit names are given in Supp. Table 3). Methylmalonate semialdehyde dehydrogenase deficiency is caused by a dysfunctional ALDH6A1. In this case, our method fails to predict the elevation of 3hpp and 3hmp as documented in OMIM. An inspection of network topology reveals that these false predictions result from missing membrane transporters for these products, which prevent their secretion and hence indirectly limit the possible uptake of their upstream substrate, valine – leading also to the false prediction of an elevated extra-cellular concentration of valine (val). These newly hypothesized 5 transporters are marked as red edges in the figure (notably though, our method correctly predicts the elevated extra-cellular concentration of 3aib in this case). Short name Full name 2kmb 2-keto-4-methylthiobutyrate dkmpp 2,3-diketo-5-methylthio-1-phosphopentane 5mdru1p 5-Methylthio-5-deoxy-D-ribulose1-phosphate 5mdr1p 5-Methylthio-5-deoxy-D-ribose1-phosphate 5mta 5-Methylthioadenosine ametam S-Adenosylmethioninamine amet S-Adenosyl-L-methionine ahcys S-Adenosyl-L-homocyteine hcys L-Homocysteine ser L-Serine cyst L-Cystathionine cys L-Cysteine met L-Methionine Supplementary Table 1: Full names of the metabolites presented in main-text figure 3. 6 Short name Full name tyr L-Tyrosine 34hpp 3-(4-Hydroxyphenyl)pyruvate akg 2-Oxoglutarate glu L-Glutamate hgentis Homogentisate 4mlacac 4-Maleylacetoacetate 4fumacac 4-Fumarylacetoacetate acac Acetoacetate fum Fumarate tym Tyramine 3ityr 3-Iodo-L-tyrosine i Iodide iod Iodine 34dhphe 3,4-Dihydroxy-L-phenylalanine thbpt Tetrahydrobiopterin thbpt4acam Tetrahydrobiopterin-4a-carbinolamine phe L-Phenylalanine Supplementary Table 2: Full names of the metabolites presented in supplementary figure 3. 7 Short name Full name val L-Valine ala_B beta-Alanine 3hpp 3-Hydroxypropanoate , (syn: 3-Hydroxypropionic acid) 3hpcoa 3-Hydroxypropionyl-CoA msa Malonate semialdehyde 3hmp 3-Hydroxy-2-methylpropanoate, (syn: 3-Hydroxyisobutyric acid ) 2mop 2-Methyl-3-oxopropanoate, (syn: Methylmalonate semialdehyde) accoa Acetyl-CoA ppcoa Propanoyl-CoA 2maacoa 2-Methyl-3-acetoacetyl-CoA 3aib L-3-Amino-isobutanoate , (syn:3-aminoisobutyric acid) Supplementary Table 3: Full names of the metabolites presented in supplementary figure 4. 8