* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Unit12cadiovascularsystem
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
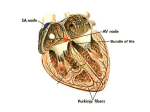
The Cardiovascular System Consists of blood, the heart and blood vessels Blood Blood: A fluid connective tissue Blood makes up about 8% of body weight ( 4-6 liters) (pH 7.4) Hematology : The study of blood Erythropoiesis: RBC formation Hematopoiesis: Process of forming any blood cells Functions: 1. Transportation: Of gases to/from cells and lungs Of nutrients, enzymes, hormones and blood cells all around the body Of wasts from cells to kidneys, lungs and sweat glands Functions: 2. Regulation: ( homeostasis) Of pH through buffer systems Of Temperature by absorbing and distribute heat Of water content of cells by diffusion to/from heart Functions: 3. Protection: Against toxins and invaders with WBCs Against blood loss through clotting Components of blood Plasma: (about 50% total volume) The liquid portion (97% water) Contains various dissolved substances ( gases, nutrients, anti-bodies and fibers) Formed Elements: cells and cell fragments Erythrocytes: Red Blood Cells (RBC) Lack nucleus and mitochondria Circulating lifespan of 120 days Each erythrocyte contains 280 million hemoglobin molecules Erythrocytes: Red Blood Cells (RBC) Destroyed by phagocytic cells in liver, spleen, and bone marrow Cannot reproduce in blood stream Anemia: abnormal low count in RBCs Erythropoiesis: rbc formation Erythrocytes: Red Blood Cells (RBC) Woman usually have 4-5 million erythrocytes per cubic millimeter of blood men have 5-6 million. If this number is considerably higher polycythemia may be the cause. If the number is considerably less, the person has anemia. Erythrocytes Leukocytes: White blood cells (wbc) Contain nucleus and mitochondria Move in ameboid fashion and can leave closed circulatory system (by diapedesis: squeeze between capillaries) Function to combat microbes Have 5000-10000per mm NEUTROPHIL The nucleus is frequently multi-lobed with lobes connected by thin strands of nuclear material. These cells are capable of phagocytizing foreign cells, toxins, and viruses. When taking a Differential WBC Count of normal blood, this type of cell would be the most numerous. NEUTROPHIL If the count exceeds this amount, the cause is usually due to an acute infection such as appendicitis, smallpox or rheumatic fever. If the count is considerably less, it may be due to a viral infection such as influenza, hepatitis, or rubella. Destroy and eat bacteria and dead cells at inflamed site EOSINOPHIL The nucleus often has two lobes connected by a band of nuclear material. (Does it looks like a telephone receiver?) The granules contain digestive enzymes that are particularly effective against parasitic worms in their larval form. EOSINOPHIL These cells also phagocytize antigen antibody These cells account for less than 5% of the WBC's complexes. Primarily combat large invaders, such as worms flukes and decrease allergic reactions BASOPHIL The basophilic granules in this cell are large, stain deep blue to purple, and are often so numerous they mask the nucleus. These granules contain histamines (cause vasodilation) and heparin (anticoagulant). In a Differential WBC Count we rarely see these as they represent less than 1% of all leukocytes the count showed an abnormally high number of these cells, hemolytic anemia or chicken pox may be the cause They intensify inflammation and o allergic reaction by releasing histamine which attracts other WBc( they sound the alarm) BASOPHIL LYMPHOCYTE Its nucleus is very large for the size of the cell and stains dark purple. (Notice that the nucleus almost fills the cell leaving a very thin rim of cytoplasm This is the second most numerous leukocyte, accounting for 25-35% of the cells counted in a Differential WBC Count. the number of these cells exceeds the normal amount, one would suspect infectious mononucleosis or a chronic infection LYMPHOCYTE MONOCYTE This cell is the largest of the leukocytes and is agranular. The nucleus is most often "U" or kidney bean shaped; These cells account for 3-9% of all leukocytes In people with malaria, endocarditis, typhoid fever, and Rocky Mountain spotted fever, monocytes increase in number. MONOCYTE THROMBOCYTES - PLATELETS Each cubic millimeter of blood should contain 250,000 to 500,000 of these. If the number is too high, spontaneous clotting may occur. If the number is too low, clotting may not occur when necessary THROMBOCYTES - PLATELETS Platelets, which are cell fragments, are seen next to the "t's" above. (Many of the other micrographs on this page contain them as well.) Platelets are important for proper blood clotting. Do you know what types of cells are these? Do you know what types of cells are these? Blood Groups and Typing • On the surface of all cell membranes ( including RBCs) are highly specific glycoprotein “flags” which are the basis of blood typing • Agglutinogens: membrane based molecules used for grouping blood into types ( “friends”) 2 types of grouping blood based on type of agglutinogens present • 1. ABO blood grouping : has 2 agglutinogens (A, B) • The blood plasma also contains proteins called agglutinins (enemies) that the blood will react against Blood Typing • % pop Blood type Agglutinogens Agglutinins accepts • 42% A A B A, O • 10% B B A B, O • 4% • • 45% • AB A, B O NONE NONE All universal acceptor A, B Only O universal donor Blood Typing • 2. “Rh” Blood grouping system: • Based on the presences or absence of a single flag ( agglutiongen) • If present = Rh + 85% ++, +• If not = Rh - 15% -• • As a general rule Rh negative group can give safely to Rh positive group, but Rh positive should not be given to Rh negative In the ABO system • The agglutinins are preformed and the first exposure ( transfusion) of the opposing blood type will initiate the clumping reaction • However in the Rh system, the agglutinins are not formed until the first exposure to the “wrong” agglutinogen ( works like immune system)… therefore clumping reaction wont occur until 2nd transfusion Rh factor • If mom is Rh negative and father is heterozygous Rh positive there is a 50% chance the child will be Rh positive • The Childs Rh positive RBC leak into the placenta and the moms circulatory system when the placental tissue breaks down… causing mom to produce Anti-Rh antibodies • The Anti-Rh antibodies pass across the placenta and destroy the RBC of the Rh positive child resulting in brain damage, mental retardation or even death • This is called Erythroblastic fetalis • Solution: Rh negative woman receive an Rh immunoglobulin injection or midway through 1st pregnancy or no later than 48 hrs after giving birth Blood Typing Blood Typing Blood Typing BLOOD DISORDERS Sickle cell anemia An inherited condition which results in some erythrocytes being malformed. The gene for this condition causes the hemoglobin to be incorrectly formed, which in turn causes some erythrocytes to take on a crescent shape. These cells are not able to carry adequate amounts of oxygen to cells Polycythemia condition in which there is a net increase in the total number of red blood cells in the body. The overproduction of red blood cells may be due to a primary process in the bone marrow or it may be a reaction to chronically low oxygen levels or, rarely, a malignancy. Thrombocytopenia Purpura a blood disorder characterized by an abnormal decrease in the number of platelets in the blood. Platelets are cells in the blood that help stop bleeding. A decrease in platelets can result in easy bruising, bleeding gums, and internal bleeding. LEUKEMIA Hemostasis: prevention of blood loss 3 mechanisms: 1. vascular spasm: damage to smooth muscle in blood vessels or platelets, causing a release of chemicals which cause vasoconstriction… reducing blood flow/loss lasing about 30 min 2. Platelet plug formation: If thrombocytes (platelets) come in contact with collagen fibers in a damaged vessels wall… a chemical change occurs The platelets become sticky and cling to each other and to the damaged area forming a plug ( thrombus) or clot If the clot moves it is called an embolus I 3. Coagulaton: A clot is a mesh of protein fibers in which formed elements are trapped Over 30 different hormones and enzymes are involved in coagulation Liquid protein fibers in the blood plasma solidify and form a mesh over the damaged area RBCs and platelets become trapped in the mesh… mean while the fibers shrink, tightening and closing the wound Thrombosis: clotting in an unbroken vessel… if the clot ( thrombus) moves it is called an embolus … if it drifts until it blocks an small vessel, this is called an embolism ( can cause heart attacks, strokes, or death) Leukemia: a malignant disease ( cancer) of blood forming tissue… resulting in excessive numbers of WBCs which crowd out the RBCs Mononucleosis: viral infection attacking lymph tissue Results in lmphocytes which are abnormal , no cure, it just runs its course Heart A hollow 4 chambered muscular organ about the size of a clenched fist and weights about 255 g in females and 310 g in males Located in the thoracic cavity between the lungs 2/3 of the heart is located left of the midline with the apex in contact with the diaphragm Enclosed in a loose fitting serous sac called pericardial sac Functions: Separate the heart from other organs Contains pericardial fluid for lubricaiton Layers of pericardium: outer fibrous , inter serous layer Pericardial cavity: between parietal pericardium and visceral pericardium Layers of heart wall Epicardium: outermost layer Myocardium: cardiac muscle, thickest portion, it contracts Endocardium: thin epithelial lining of the heart chambers Chambers and valves 4 chambers The two upper heart chambers are atria ( atrium) (auricles on outside of the heart) The wall between the two atria is called the interatrial septum The depression in the interatrial septum is called the fossa ovalis, which used to be an opening during fetal development and blood could flow from right atrium to left atrium (can be seen in the right atrium) The two lower chambers are called the ventricles The wall between the 2 ventricles is called the interventricular septum The left ventrical wall is thicker than the right, due to the way the blood circulates in the body Chordae tendinae: cords that connect valves to papillary muscles Papillary muscle: small raised projections of muscle tissue that connect chordae tendinae to endothelium of heart Trabeculae carneae: distinct ridges in walls of ventricles A condition called prolapse involves leaky valves due to stretched chordae tendineae Valves 1. Bicuspid (mitral ) valve: located between left atrium and left ventricle ( most commonly replaced valve) 2. Tricuspid valve: located between right atrium and ventricle 3. Aortic semilunar valve: opens from right ventricle to base of aorta 4. Pulmonary semilunar valve: opens from left ventricle to pulmonary artery Coronary circulatory system The heart has its own circulatory system Most heart problems are due to faulty or blocked coronary circulation… resulting in poor nutrients and oxygen supply to myocardium Ischemia: reduced blood flow, weakens heart Angina: chest ( heart) pain due to ischemia Infaction: death of an area of tissue due to an interupted blood supply Myocardial infarction: heart attack due to infarction and weakened heart , usually caused by an embolus or a thrombus Atherosclerosis: build up of cholesterol or other fatty compounds on the inside of blood vessel wall, decreases or blocks circulation Coronary artery disease: a condition of damaged heart muscle due to one of the above reductions in blood supply. The number 1 cause of death in USA Heart murmers: unusual sounds generally due to valve disorders ( leaky): 1. faulty chordae tendinea 2. disease damaged valves/ cusps Cardiac cycle (blood pressure) The 2 atria contract, pumping blood into the 2 ventricles which are relaxed while being filled. Then the ventricles contract while the relaxed atria are refilled from the vena cava (pulmonary veins) Systole: phase of contraction (top #) Diastole: phase of relaxation ( bottom #) So during ventricular diastole, the tri and bicuspids are open The 2 atria are in systole and the ventricles are filling Then the atrial diastole and ventriclular systole The cuspids close, similunars open, ventricles empty, Atria fill Then brief pause and cycle repeats 8 sec per cycle with about 72 beats per minute Heart Rate Average Heart Rate of some Mammals 400 300 200 200 50 30 100 28 0 376 9 70 40 ca me l ca t co ele w ph an gre yw t ha le hu ma n lio n mo us e Heartbeats per minute can be determined using a Stethoscope Mammals Lub If you listen to your heartbeat, it makes a lub dub sound. The lub is when blood is pushed out of the heart into the body and the dub is the reloading of the heart with more blood ready to push it out to the body Dub The heart is made of cardiac muscle. When the cells receive an electrical impulse they contract - causing a heartbeat. Cardiac muscle is myogenic - it can contract on its own, without needing nerve impulses. Major factors influencing blood pressure 1. cardiac output: heart rate ( neural or hormonal control) 2. Blood volume: regulating water content of blood kidneys regulate blood volume 3. Resistance of Arteries to blood flow Hypotension = low BP Hypertention = high BP The heart is actually a double pump with 2 separate circulatory systems 1. Pulmonary circulation: The short loop pumped by the right ventricle from the heart to the lungs and back to the heart Serves only to bring blood in contact with alveoli resulting in gas exchange It does not meet the needs ( metabolic) of the lung tissue 2. Systemic circulation: the many loops pumped by the left ventricle through aorta, serving the whole heart Circulation Through the heart Aorta---arteries---capillaries---veins---vena cavae—right atrium ---(thru tricuspid valve) to----right ventricle---(thru pulmonary semilunar valve) to---lung capillaries--pulmonary veins---left atrium---thru mitral valve to ----left ventricle---(thru aortic semilunar valve) back to----- aorta (to start again) Conduction system Cells in the heart beat as a unit due to the intercalated disks which weaves the cell endings together The orderly sequence of atrial and ventricular contraction is maintained by an intrinsic (internal) regulating system called a conduction system Conduction system This conduction system consists of specialized muscle tissue which generates and conducts electrical impulses to stimulate the cardiac muscle to contract in a cycle as a unit Consists of the S.A node and the A.V. node Sinoatrial node (SA node) This specialized node is found on the upper inside wall of the right atrium. The SA node is known as the pacemaker of the heart and initiates a heartbeat every 0.85 seconds. This signal travels across the atria causing them to contract and load the ventricles with blood. Ventricles are electrically insulated from atria so they don’t contract yet. Sinoatrial node ( S.A, node or pacemaker) Located in the right atrial wall Initiate cardiac cycle ( sets the pace) by sending impulses to both atria causing them to contract… This impulse also travels to the atrioventricular node Atrio-ventricular node (AV node) The AV node is located on the bottom surface of the right atria and is responsible for initiating the contraction of the ventricles. Electrical impulse passes to ventricles via AV node and the Bundle of His. They pass the impulse to the base of the ventricles (~ 0.1 s delay). The bundle of His is a group of fibres that conduct impulses to Purkyne fibres which carry impulses to left & right ventricles. Ventricles then contract from the bottom upwards. Atrioventricular node (A.V.) Found on the septum (wall) between the right atrium and right ventricle Sends impulses to the ventricles over a bundle of branching conducting fibers called the A.V. bundle ( bundle of his) These fibers keep branching until the smallest make contact with cells in the myocardium Electrocardiograph P = atrial systole QRS = ventricular systole T = ventricular diastole Q wave: absent on EKG. Necrosis (death of an area of the heart muscle produces a Q wave on EKG) used to diagnose heart attack Myocardial infarction is usually related to the left ventricle PR interval: problem in conduction system ( S.A node A.V node) HOW TO READ EKG Determine the heart rate from EKG 1. First find a specific R wave that peaks on a heavy line 2. Next count off 300, 150, 100, 75, 60, 50 for every thick line. Know these numbers , you will use them 3. Where the next R wave falls determines the rate Ventricular fibrillation is an abnormal heart rhythm that is disorganized and irregular. Ventricular tachycardia is a rapid, regular heart rhythm that originates in the lower chambers of the heart. Heart Facts Hold out your hand and make a fist. If you're a kid, your heart is about the same size as your fist, and if you're an adult, it's about the same size as two fists. Your heart beats about 100,000 times in one day and about 35 million times in a year. During an average lifetime, the human heart will beat more than 2.5 billion times. Give a tennis ball a good, hard squeeze. You're using about the same amount of force your heart uses to pump blood out to the body. Even at rest, the muscles of the heart work hard--twice as hard as the leg muscles of a person sprinting. circulation William Harvey (1578-1657 First described blood circulatory system in humans Used fish to figure out the flow of blood Left ventricle holds 2 ounces of blood Heart beats about 70 beats/minute In one hr: 2 oz x 70 beats x 60 min = 84000 oz = 528 pounds of blood Thus concluded blood must be reused Vessels and routes Arteries: blood vessels which carry 1. 2. 3. blood away from the heart Arterial walls consist of 3 layers ( tunicas) around a hollow (lumen) tube Tunica intima: internal lining Tunica media: middle thickest tunica( made of smooth muscle) Tunica externa: tough outer coat that acts as prtection 1 2 3 Arterioles: small arteries Capillaries: microscopic blood vessels, the walls of which consist of only a thin layer of endothelium. Capillaries allow for the exchange of nutrients, gases and waste to take place by diffusion between blood plasma and various tissue cells. Venules: small vessels that receive blood from capillaries and merge into veins Veins: carry blood to the heart, have very low pressure and valves 2 factors that assist venous blood movement 1. Valves: veins have backflow preventing 2. valves If faulty or leaky results in varicose veins Muscle contractions: When muscles which surround the veins ( especially arms and legs) contract they squeeze the veins pushing blood from valve to valve varicose veins Pulse: the alternating expansion and elastic recoil of the walls of an artery ( due to ventricular systole and diastole) Pulse rate: heart rate = 70 to 80 per min Blood pressure: pressure (measured in arteries) exerted by left ventricular systole and remaining during diastole Average B.P. 120/80 The difference between the 2 numbers is a measure of the health of the artery Hepatic Portal Circulation Blood enters liver from 2 sources: 1. The liver is supplied with oxygen rich blood by hepatic artery ( not part of hepatic portal system) 2. Veins drain the stomach, intestines, pancreas etc… and merge into the hepatic portal vein which brings this nutrient rich blood to the liver for processing Blood leaves the liver by way of the hepatic vein and enters the inferior vena cava A prtal system is: Arteries—capillaries—veins—capillaries— veins As opposed to normal: Artery—capillary --veins Fetal circulation Differs from adults because lungs, kidneys and GI tract are not functional Fetal and maternal blood does not mix Key Differences in a fetus 1. Foramen ovale: hole between 2 atria, so blood can bypass the right ventricle and pulmonary circuit ( later closes leaving a scar called the fossa ovalis) 2. Ductus arteriosus: vessel running from pulmonary trunk to aorta, skipping pulmonary circuit. 3. Umbilical arteries: 2 arteries which branch off the internal iliacs carry deoxygenated blood and waste to the placenta 4. Umbilical vein: leaves placenta with oxygenated blood heading toward fetal heart, it bypasses the liver by way of the ductus venosus ( which leads straight into the inferior vena cava) Another modification involves fetal hemoglobin It is slightly more attracted to oxygen than is normal hemoglobin so fetus cant “steal” moms oxygen