* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Electrical Risk Stratification After STEMI
Remote ischemic conditioning wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
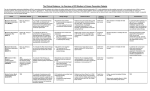
Electrical Risk Stratification After STEMI Peter Cheung, MD, FACC Section of Electrophysiology, Division of Cardiology, Scott & White Clinic Texas A&M Health Science Center Liew, Heart 2010; 96: 1086-94 Define Electrical Risk Stratification • I. Whether patient has a ventricular arrhythmia that is a marker for increased risk of sudden cardiac death (SCD). • II. Whether there is any electrocardiographic risk stratification scheme for a patient with low EF. Electrical Risk Stratification • For all practical purposes, risk stratification is same whether it is STEMI or NSTEMI. • Risk stratification for patient without CAD is outside the scope of this talk. Epidemiology of VA & SCD Incidence of Sudden Cardiac Death Events Incidence General population High-risk subgroups Any prior coronary event EF<30% or heart failure MADIT II Cardiac arrest survivor AVID, CIDS, CASH Arrhythmia risk markers, post MI MADIT I, MUSTT 0 10 20 Percent 30 Myerburg RJ, Kessler KM, Castellanos A. Circulation 1992;85:12-10. 0 150,0000 SCD--HeFT 300,000 Absolute Number Why do we even ask? Major Implantable Cardioverter-Defibrillator Trials for Prevention of Sudden Cardiac Death Trial Year Patients (n) Inclusion Criterion: LVEF Additional Study Features Hazard Ratio* 95% CI p MADIT I 1996 196 < 35% NSVT and EP+ 0.46 (0.26-0.82) p=0.009 MADIT II 2002 1232 < 30% Prior MI 0.69 (0.51-0.93) p=0.016 CABG-Patch 1997 900 < 36% +SAECG and CABG 1.07 (0.81-1.42) p=0.64 DEFINITE 2004 485 < 36% NICM, PVCs or NSVT 0.65 (0.40-1.06) p=0.08 DINAMIT 2004 674 < 35% 6-40 days post-MI and Impaired HRV 1.08 (0.76-1.55) p=0.66 SCD-HeFT 2006 1676 < 35% Prior MI or NICM 0.77 (0.62-0.96) p=0.007 AVID 1997 1016 < 40% Prior cardiac Arrest, or Unstable VT 0.62 (0.43-0.82) p<0.02 CASH† 2000 191 Mean < 45% ±18 at baseline Prior cardiac arrest 0.766 ‡ 1-sided p=0.081 CIDS 2000 659 < 35% Prior cardiac Arrest, Unstable VT, or Syncope 0.82 (0.60-1.1) NS * Hazard ratios for death from any cause in the ICD group compared with the non-ICD group. Includes only ICD and amiodarone patients from CASH. ‡CI Upper Bound 1.112. CI indicates Confidence Interval, EP+ = positive electrophysiologic study, HRV = heart rate variability, LVEF = left ventricular ejection fraction, MI = myocardial infarction, NICM = nonischemic cardiomyopathy, NS = Not statistically significant, NSVT = nonsustained ventricular tachycardia, PVCs = premature ventricular contractions, SAECG = signal-averaged electrocardiogram, VT = ventricular tachycardia. Epstein A, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. J Am Coll Cardiol 2008; 51:e1–62. Table 5. DiMarco. NEJM 2003; 349:1836-1847 Drugs don’t prevent SCD • Antiarrhythmic Drugs worse than Placebo – CAST (Cardiac Arrhythmia Suppression Trial) – MUSTT (Multicenter Unsustained Tachycardia Trial) • ICD better than Antiarrhythmic Drugs – – – – AVID (Antiarrhythmic versus Implantable Defibrillators) CIDS (Canadian Implantable Defibrillator Study) CASH (Cardiac Arrest Study Hamburg) SCD-HeFT (Sudden Cardiac Death in Heart Failure Trial) • Amiodarone no better than Placebo – SCD-HeFT (Sudden Cardiac Death in Heart Failure Trial) CAST CAST Investigators, Aug 1989, NEJM SCD-HeFT Problems with ICD • Very expensive • Complications of infection, vascular injuries, inappropriate ICD shocks Why Electrical Risk Stratification? • Identify patients that you can do something about- ICD • Avoid overtreating – Expensive – Complications associated with ICD • Unfortunately, electrical risk stratification is more or less an academic exercise Electrical Risk Stratification • I. Whether patient has a ventricular arrhythmia that is a marker for increased risk of sudden cardiac death (SCD). • II. Whether there is any electrocardiographic risk stratification scheme for patient with low EF. What type of electrical risk marker? (> 48 hours post-MI) • PVC’s (CAST) • NSVT & (+) EP Study (MADIT, MUSTT) • VT/VF (AVID, CIDS, CASH) What type of electrical risk marker? (> 48 hours post-MI) • PVC’s (CAST) • NSVT & (+) EP Study (MADIT, MUSTT) • VT/VF (AVID, CIDS, CASH) . Pratt C M , Moyé L A Circulation 1995;91:245-247 Copyright © American Heart Association What type of electrical risk marker? (> 48 hours post-MI) • PVC’s (CAST) • NSVT & (+) EP Study (MADIT, MUSTT) • VT/VF (AVID, CIDS, CASH) NSVT & (+) EP Study • MADIT (Multicenter Automatic Defibrillator Implantation Trial)- prior MI (> 3wk), NSVT (> 120bpm), EF ≤ 35%, no revascularization in 3 months • MUSTT (Multicenter Unsustained Tachycardia Trial)- CAD, LVEF ≤ 40%, NSVT, +EPS Multicenter Unsustained Tachycardia Trial- MUSTT • CAD, LVEF ≤ 40%, NSVT, +EPS • No statistically significant difference in the frequency or duration of spontaneous nonsustained ventricular tachycardia was seen between patients with and those without inducible sustained ventricular tachycardia. What type of electrical risk marker? (> 48 hours post-MI) • PVC’s (CAST) • NSVT & (+) EP Study (MADIT, MUSTT) • VT/VF (AVID, CIDS, CASH) Major Implantable Cardioverter-Defibrillator Trials for Prevention of Sudden Cardiac Death Trial Year Patients (n) Inclusion Criterion: LVEF Additional Study Features Hazard Ratio* 95% CI p MADIT I 1996 196 < 35% NSVT and EP+ 0.46 (0.26-0.82) p=0.009 MADIT II 2002 1232 < 30% Prior MI 0.69 (0.51-0.93) p=0.016 CABG-Patch 1997 900 < 36% +SAECG and CABG 1.07 (0.81-1.42) p=0.64 DEFINITE 2004 485 < 36% NICM, PVCs or NSVT 0.65 (0.40-1.06) p=0.08 DINAMIT 2004 674 < 35% 6-40 days post-MI and Impaired HRV 1.08 (0.76-1.55) p=0.66 SCD-HeFT 2006 1676 < 35% Prior MI or NICM 0.77 (0.62-0.96) p=0.007 AVID 1997 1016 < 40% Prior cardiac Arrest, or Unstable VT 0.62 (0.43-0.82) p<0.02 CASH† 2000 191 Mean < 45% ±18 at baseline Prior cardiac arrest 0.766 ‡ 1-sided p=0.081 CIDS 2000 659 < 35% Prior cardiac Arrest, Unstable VT, or Syncope 0.82 (0.60-1.1) NS * Hazard ratios for death from any cause in the ICD group compared with the non-ICD group. Includes only ICD and amiodarone patients from CASH. ‡CI Upper Bound 1.112. CI indicates Confidence Interval, EP+ = positive electrophysiologic study, HRV = heart rate variability, LVEF = left ventricular ejection fraction, MI = myocardial infarction, NICM = nonischemic cardiomyopathy, NS = Not statistically significant, NSVT = nonsustained ventricular tachycardia, PVCs = premature ventricular contractions, SAECG = signal-averaged electrocardiogram, VT = ventricular tachycardia. Epstein A, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. J Am Coll Cardiol 2008; 51:e1–62. Table 5. Electrical Risk Stratification • I. Whether patient has a ventricular arrhythmia that is a marker for increased risk of sudden cardiac death (SCD). • II. Whether there is any electrocardiographic risk stratification scheme for patient with low EF. EKG risk markers ? • • • • QRS duration- conflicting data Fragmented QRS- undetermined QT dispersion- undetermined Early repolarization- undetermined Risk Stratification Tests • • • • • Signal Average ECG Holter T wave alternan Electrophysiology Study None Signal-Averaged ECG • • • • • Ventricular Late Potentials (VLPs) Potential substrate to ventricular arrhythmia Seen in 25-50% after AMI Sensitivity 15-75% Prognostic value seems much diminished in patients who underwent revascularization. Conventional Holter • PVCs • NSVT • Low sensitivity and specificity Heart rate variability • • • • SD of RR intervals Measures of cardiac autonomic tone HRV decreases with AMI Decreased HRV associated with increased mortality- Multicenter Postinfarction Study (MPS) • Revascularization seems to improve HRV Heart Rate Turbulence • Fluctuations in sinus rhythm following PVC • REFINE Study (Noninvasive Risk Assessment Early After a Myocardial Infarction)- (+) Study especially performing at 10-14 weeks. • ISAR-Risk Study (Improved Stratification of Autonomic Regulation for risk prediction in post-infarction patients with preserved left ventricular function)- (+) Microvolt T-Wave Alternans (MTWA) MASTER (Microvolt T Wave Alternans Testing for Risk Stratification of Post-Myocardial Infarction Patients) Trial- CAD, EF < 30%, (-) patients have less event. ABCD (Alternans Before Cardioverter Defibrillator) Trial- 1 year PPV 9%, NPV 95%. Patients not immediately post-MI. Whether revascularization may affect MTWA is not studied. EP Study • MADIT (Multicenter Automatic Defibrillator Implantation Trial)- prior MI (> 3wk), NSVT (> 120bpm), EF ≤ 35%, no revascularization in 3 months • MUSTT (Multicenter Unsustained Tachycardia Trial) What clinical roles do electrical risk stratification play? • Not much. • Noninvasive electrophysological testing may be helpful but guidelines do not support ICD use based on it. • Guidelines support invasive EP study to risk stratify patients with NSVT and EF between 35-40%. • Guidelines support risk stratification by nonelectrophysiological means. Dichotomy of Approach • Most clinical trials trend toward broader use of ICD – AVID- history of SCD – MADIT 1- NSVT, + EPS, EF ≤ 35% – MUSTT- NSVT, + EPS, EF ≤ 40% – MADIT 2- EF ≤ 30% – SCD-HeFT- EF ≤ 35% • Electrical Risk Stratification means selective (reduced) use of ICD Major Implantable Cardioverter-Defibrillator Trials for Prevention of Sudden Cardiac Death Trial Year Patients (n) Inclusion Criterion: LVEF Additional Study Features Hazard Ratio* 95% CI p MADIT I 1996 196 < 35% NSVT and EP+ 0.46 (0.26-0.82) p=0.009 MADIT II 2002 1232 < 30% Prior MI 0.69 (0.51-0.93) p=0.016 CABG-Patch 1997 900 < 36% +SAECG and CABG 1.07 (0.81-1.42) p=0.64 DEFINITE 2004 485 < 36% NICM, PVCs or NSVT 0.65 (0.40-1.06) p=0.08 DINAMIT 2004 674 < 35% 6-40 days post-MI and Impaired HRV 1.08 (0.76-1.55) p=0.66 SCD-HeFT 2006 1676 < 35% Prior MI or NICM 0.77 (0.62-0.96) p=0.007 AVID 1997 1016 < 40% Prior cardiac Arrest, or Unstable VT 0.62 (0.43-0.82) p<0.02 CASH† 2000 191 Mean < 45% ±18 at baseline Prior cardiac arrest 0.766 ‡ 1-sided p=0.081 CIDS 2000 659 < 35% Prior cardiac Arrest, Unstable VT, or Syncope 0.82 (0.60-1.1) NS * Hazard ratios for death from any cause in the ICD group compared with the non-ICD group. Includes only ICD and amiodarone patients from CASH. ‡CI Upper Bound 1.112. CI indicates Confidence Interval, EP+ = positive electrophysiologic study, HRV = heart rate variability, LVEF = left ventricular ejection fraction, MI = myocardial infarction, NICM = nonischemic cardiomyopathy, NS = Not statistically significant, NSVT = nonsustained ventricular tachycardia, PVCs = premature ventricular contractions, SAECG = signal-averaged electrocardiogram, VT = ventricular tachycardia. Epstein A, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. J Am Coll Cardiol 2008; 51:e1–62. Table 5. Epidemiology of VA & SCD Incidence of Sudden Cardiac Death Events Incidence General population High-risk subgroups Any prior coronary event EF<30% or heart failure MADIT II Cardiac arrest survivor AVID, CIDS, CASH Arrhythmia risk markers, post MI MADIT I, MUSTT 0 10 20 Percent 30 0 150,0000 SCD--HeFT 300,000 Absolute Number Reused with permission from Myerburg RJ, Kessler KM, Castellanos A. Circulation 1992;85:12-10. ICD I IIa IIb IIbIII III I IIa IIb III “is indicated in patients who are survivors of cardiac arrest due to VF or hemodynamically unstable sustained VT after evaluation to define the cause of the event and to exclude any completely reversible causes.” “is indicated in patients with structural heart disease and spontaneous sustained VT, whether hemodynamically stable or unstable.” I IIa IIb III “is indicated in patients with syncope of undetermined origin with clinically relevant, hemodynamically significant sustained VT or VF induced at EP study. “ All primary SCD prevention ICD recommendations apply only to patients who are receiving optimal medical therapy and have reasonable expectation of survival with good functional capacity for more than 1 year. ICD I IIa IIb IIbIII III “is indicated in patients with LVEF ≤ 35% due to prior MI who are at least 40 days post-MI and are in NYHA functional Class II or III.” I IIa IIb III I IIa IIb IIbIII III I IIa IIb III “is indicated in patients with nonischemic DCM who have an LVEF ≤ 35% and who are in NYHA functional Class II or III.” “is indicated in patients with LV dysfunction due to prior MI who are at least 40 days post-MI, have an LVEF ≤ 30%, and are in NYHA functional Class I.” “is indicated in patients with nonsustained VT due to prior MI, LVEF ≤ 40%, and inducible VF or sustained VT at EP study. “ All primary SCD prevention ICD recommendations apply only to patients who are receiving optimal medical therapy and have reasonable expectation of survival with good functional capacity for more than 1 year. ICD I IIaIIbIII ICD implantation is reasonable for patients with unexplained syncope, significant LV dysfunction, and nonischemic DCM. I IIaIIbIII I IIaIIbIII ICD implantation is reasonable for patients with sustained VT and normal or near-normal ventricular function. ICD implantation is reasonable for patients with HCM who have 1 or more major† risk factors for SCD. I IIaIIbIII ICD implantation is reasonable for the prevention of SCD in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) who have 1 or more risk factors for SCD. I IIaIIbIII ICD implantation is reasonable to reduce SCD in patients with long-QT syndrome who are experiencing syncope and/or VT while receiving beta blockers. All primary SCD prevention ICD recommendations apply only to patients who are receiving optimal medical therapy and have reasonable expectation of survival with good functional capacity for more than 1 year. † See Section 3.2.4, “Hypertrophic Cardiomyopathy,” in the full-text guidelines for definition of major risk factors. Defibrillator in Acute Myocardial Infarction (DINAMIT) Trial • 674 patients < 40 days post-MI with LVEF ≤ 35% and decreased heart rate variability • Randomized to ICD therapy (n=332) or no ICD therapy (n=342) • Arrhythmic death ↓ in ICD group, but ↑ in nonarrhythmic death (6.1% per year vs. 3.5% per year, HR 1.75 (95% CI 1.11 to 2.76; p=0.016) • No difference in total mortality Hohnloser SH, Kuck KH, Dorian P, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med 2004;351:2481-8. MI < 40days, EF ≤ 35%, decreased heart rate variability Hohnloser SH, Kuck KH, Dorian P, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med 2004;351:2481-8. Hohnloser SH, Kuck KH, Dorian P, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med 2004;351:2481-8. Defibrillator Implantation Early After Myocardial Infarction (IRIS) MI < 40days, EF ≤ 40% (± NSVT) NEJM 2009: 361:1427-36 IRIS NEJM 2009: 361:1427-36 Summary • With the exception of EP Study, current guidelines neglect use of electrophysiological stratification and relies mostly on EF and NYHA. • Some non-invasive electrophysiological tests may identify patients who are at lower risk of SCD. Further studies are needed. • Revascularization may reverse some electrophysiological risk markers. • Beware of risk stratification too early after myocardial infarction. Intervention too early after an MI does not seem to be beneficial. Suggested Reading Liew, R. Prediction of sudden arrhythmic death following acute myocardial infarction. Heart 2010; 96:1086-1094. ACC/AHA/ESC 2006 Executive Summary. Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. ACC/AHA/HRS 2008 Executive Summary. Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities.