* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Setting the Heart`s Tempo
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
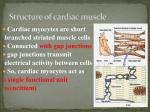
Setting the Heart’s Tempo Heart, or cardiac, muscle differs from other types of muscle. Like skeletal muscle, cardiac muscle appears striated (grooved or ridged) when viewed under a microscope. But unlike skeletal muscle, cardiac muscle displays a branching pattern. The greatest difference stems from the ability of this muscle to contract without being stimulated by external nerves. Muscle with this ability, called myogenic muscle, explains why the heart will continue to beat, at least for a short time, when removed from the body. The heart’s tempo or beat rate is set by the sinoatrial (SA) node. This bundle of specialized nerves and muscles is located where the venae cavae enter the right atrium. The SA node acts as a pacemaker, setting a rhythm of about 70 beats per min for the heart. Nerve impulses are carried from the pacemaker to other muscle cells by modified muscle tissue. Originating in the atria, the contractions travel to a second node, the atrioventricular (AV) node. The AV node serves as a conductor, passing nerve impulses via two large nerve fibres, called Purkinje fibres, through the septum toward the ventricles. The Purkinje fibres run along the septum that separates the right and left ventricles, carrying impulses from the AV node to the bottom tip of the heart. From here, these branching fibres carry impulses up along the outer walls of the ventricles back toward the atria. A wave of cardiac contraction follows the nerve pathway. Both right and left atria contract prior to the contraction of the right and left ventricles. One of the greatest challenges for surgeons performing open-heart surgery is to make incisions at the appropriate location. A scalpel placed in the wrong spot could cut fibres that conduct nerve impulses. Heart rate is influenced by autonomic nerves. Two regulatory nervous systems—the sympathetic and parasympathetic nervous systems—conduct impulses from the brain to the SA node. Stimulated during times of stress, the sympathetic nerves increase heart rate. This increases blood flow to tissues, enabling the body to meet increased energy demands. Conditions in which the heart rate exceeds 100 beats per min are referred to as tachycardia. Tachycardia can result from exercise or from the consumption of such drugs as caffeine or nicotine. During times of relaxation, the parasympathetic nerves are stimulated to slow the heart rate. Diagnosing Heart Conditions Doctors can use electrocardiographs, which map electrical fields within the heart, to make tracings to diagnose certain heart problems. Electrodes placed on the body surface are connected to a recording device. The electrical impulses are displayed on a graph called an electrocardiogram (ECG). Changes in electrical current reveal normal or abnormal events of the cardiac cycle. The first wave, referred to as the P wave, monitors atrial contraction. The larger spike, referred to as the QRS wave, records ventricular contraction. A final T wave signals that the ventricles have recovered. A patch of dead heart tissue, for example, will not conduct impulses and produces abnormal line tracings. By comparing the tracings, doctors are able to locate the area of the heart that is damaged. Define the following words: Myogenic Muscle, SA node, Av Node, Purkinje fibers, Sympathetic nervous system, Parasympathetic nervous system, septum, Pulmonary circulatory system, systemic circulatory system, atria, ventricles, Atrioventricular valves, semilunar valves, Aorta, coronary arteries,