* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 21 – hip and back pain in adults Should know differentials
Adoptive cell transfer wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
Osteochondritis dissecans wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Myasthenia gravis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
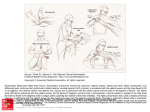
Lecture 21 – hip and back pain in adults Should know differentials of hip and back pain anterior: osteoarthritis, psoas syndrome, patellafemoral syndrome lateral: IT band syndrome, greater trochanter bursitis, meralgia paresthetica, “dead butt syndrome” posterior: piriformis syndrome, spondyloysis, spondylolisthesis Hip pain: sciatic nerve can cause hip and back pain from piriformis syndrome: sacralplexus directly beneath or through the pirimormis muscle. Also lateral femoral cutaneous nerve can cause meralgia paresthetica: nerve entrapment as it passes through inguinal ligament Anterior Hip Pain 1. Psoas Syndrome “snapping hip”/iliopsoas a. Origin: L1.L4 joints iliacus at ingunia and inserts on lesser trochanter b. MOA: hip flexion, tendon bursa becomes inflamed in dancers gymnast complaining of anterior pain/ groin pain. 2. Patellofemoral syndrome a. MAO: most common knee pain, due to overuse, tight hamstrings, weak hip abductors (g.medius,minimus muscles) b. Worsens while squatting, walking up stairs, sitting and standing after long periods of time Lateral Hip Pain 1. IT band a. MAO: overuse syndrome common in runners b. OBERS: abduct, extend hip and the knee wont dip down c. In between the tensor fascia latae and glut. Maximus d. O: lateral iliac crest inserts on the lateral tubercle of the tibia 2. Greater troachanter bursitis a. “Hip pain” points laterally to hip b. MAO: exaggerated movement of G.medius tendon/ tensor fascia over used by flexing of hip c. Presentation: can radiate, lateral hip pain, point tenderness, seen in older people and gymnast. 3. Meralgia Paresthetica a. MAO: mononeuropathy of lateral femoral cutaneous nerve due to excess weight/stress. Can get entrapped near the inguinal ligament because it travels through the fascia latae so movement between thigh and pelvis can stretch the nerve causing entrapment. b. Test: tinnels test over inginual ligament or deep palpation to ASIS. 4. Dead Butt syndrome: gluteus medius tendonitis a. Origin: external ilium and Inserts on greater trochanter b. Symptoms: weakness of the g. medius/ with tight iliopsoas and weak abdominals c. Test: Trendelenberg sign: hip goes down on one side, pain in abduction/rotation. They have wobbly gait, point tenderness of Trochanter and positive test. Posterior Hip Pain a. Symptoms in sedentary patients with sciatic pain in butt down the leg. Worse with exercise and pain is reproduce din adductions/IR. Helps with external rotation and abduction. b. O/I: anterolateral sacrum, greater trochanter c. Treat: piriformis counterstain Spondylolysis Vs Spondylolisthesis Spondylosis is weakness of stress fracture in on of the bony bridges that connects upper and lower facet joints (usually L5) where spondylolisthesis is the sliding of vertebrae (L5-S1). Both are seen in young athletes with continuous hyperextension (gymnast) but also in post menopausal, older men. You can see middle line tenderness. With the spondylolistheses the x-ray will have a step off a neurological issues can occur via impingement. Lecture 22 – crystal arthropathies Treatment for Gout Pathophysiology: underexcretors (genetic) or overproducers (genetic, or environment) Physical findings: spontaneous onset, chills, fever, malaise, podgra, coronary artery disease, topi Diagnostics: negatively birefrngent crystals. Increase serum uric acid above 6.5 mg/dL. Urinary with low uric acid points to underexcretor. Short term = NSAIDS, ice, colchicine, steroid (prednisone) Long term = allopurinol, febuxostat Diagnosis for Gout with aspiration and synovial fluid culture. Would see negative birefringement syndrome Rheumatory Arthritis Diagnose RA via: rheumatory factor and anti-CCP in a blood culture PM&R: Exercise to match the ability and fitness level, heat or ice to make it feel better. Diagnose polymyalgia rheumatica by treating with steroids and should go away in 2 days. o Make sure you taper down the steroids and slowly start with 10 mg. Dermatomyositis – Pathophysiology DM: T cells will build up in between the muscles and steroid treatment will not work. In labs we will see these T cells between the muscles and make sure you look for malignancies. Clinical Findings: shoulder/hip black female*, pain in large muscles, malaise, fatigue, weight loss. Higher in blacks and higher in males. Affects symmetrical muscles* Prednisone wont work in these patients. Helotrophic rash, polkilderma, gattron papules, sparing of periorbital folds Diagnosis: diagnosis it via muscle biopsy but so we don’t have to do that we can see an elevated creatine kinase. Watched for cardiac, pulmonary and GI muscle problems (because affecting muscles!) Polymyalgia rhematica Pathophysiology: does not affect the muscles. Increased ESR, anti CCP/R (T cells and increased IL-6) Clinical findings: shoulder/hip, older in age (71), worse in the morning, are to get up from the chair, very fatigued, bad range of motions, tender. Quickly start to steroids and watch for vasculitis and steroid side affected. (Giant cell arthritis Lecture 23 – rheumatic disorders. JIA – juvenile idiopathic arthritis: IL-6, IL-1,TNF alpha Type Age Gender Diagnosis Complications Joints affected Systemic JIA 2-4 y/o 1:1 25% severe destructive joint disease Polyarticular arthritis in small to medium joints follows fever Oligioarticular 1-5 y/o Girls 4:1 Fevers for at least 2 weeks with rash hepatosplenomegaly, lymphadenopathy, serositis. Negative RF/ rarely positive ANA 70% ANA+ (higher risk of uveitis) Knee>ankle big joints Persistent or Extended Polyarticular 2-5 (ANA+) or early teenage (RF+) Girls Uveitis or I ridocyclitis (cataracts, synechiae, glaucoma leads to blindness) Blindness, osteoporosis RF (-): <10 ANA+ RF(+)/ Anti CCP: >10 rapid severe onset RF-: knees, wrist ankles RF+: hands feet Enthesitis Psoariatic 9-12 y/0 Males 9:1 Arthritis and (2) sacroiliac pain, HLAb27*, symptomatic uveitis (pain), positive FH Chronic arthritis and psoriasis or Arthritis and 1* FH of psoriasis plus dactylitis or fingernail abnormal HLA b-27* Lower limbs and spine, any number of joints. Axial involvement Arthritis is after psoriasis Peripheral and or axial arthritis asymmetric small and medium joints. Complications: joint destruction and uveitis/glaucoma make sure you monitor these throughout. Also monitor for spondyloarthrpathies Diagnostic Criteria*: joint effusion plus two of the following pain, warmth, erythema, limited ROM. Presence has to be at least one joint at least six weeks and onset before 16. For joint pain history is key! Pain, age and precipitating factors Treatment: stop synovitis to prevent joint destruction and blindness (not pain relief. 1 st line is NSAIds, Glucocorticoids then DMARDS methotrexate (IL inhibitor, TNF alpha and IL-6 inhibitor) JIA vs Septic Joint? Pain when you touch septic joint/wont be able to stand. Know by symptoms/joint aspiration. JIA and septic arthritis all have warm, acute pain and severely painful ROM. In JIA we will see a bilateral arthritis in comparison to septic. In RA biopsy we will see infiltrates of blood vessels, inflammatory cells, and lymphocytes where in septic arthritis we will see these but it will also grow on culture Lupus (SLE) – rash (butterfly/mallor/photosensitive), systemic symptoms. Need to ask heart block for maternal history! Watch for renal problems and med toxicity. Kids will have more hematologic, fever and cutaneous signs. Diagnose with anti-dsDNA (most specific), ANA 100% +, anti-smith is 30% Pathophysiology = autoimmune (immune complexes)/autoimmune dysfunction. The immune complexes bind to the mast cells African American woman* (non-white people know this). Cause immune complexes via histamine and mast cells Juvenile Dermatomyositis Characteristics: heliotropic rash (with nasolabial sparing *lupus*), Gattrons papules (dorsum of hand, knees), Calcinosis of muscle, nail bed changes Diagnosis: Skin (Gattrons/helptrophic) plus 2 of progressive symmetrical proximal weakness or increase serum muscle enzymes (CPK*,LDK,AST,ALT) complications: calcinosis, cellulitis, pulmonary via treatment, liver failure, GI pleed from muscles. Septic Arthritis vs Toxic Synovitis Septic: refusal to bear weight 95% of the time*, high fever, elevated ESR/CRP/WBC, red hot swollen tender joint. Hip is flexed abducted and externally rotated. Draw blood culture Toxic: pain is limited ROM of the hip Henock shlomlin perpura –abdominal pain, rash, musculoskeletal pain MSK findings: arthritis/arthralgia, oligoarticular, usually lower extremity/large joints, no periarticular swelling/tenderness, no effusion, redness, warmth Complications = GI initial problems because intussception and we can screen via ultrasound which later goes into renal disease so we need to monitor the blood pressure and urinary analysis (creatine kinase) Lecture 24/25 – immune mediated musculoskeletal disorders Rheumatory Arthritis Diagnosis: rheumatoid factors (immune complex test for autoantibody to self IgM binding to self IgG FC receptor), anti-CCP(most specific), ESR, CRP, ANA. Swann Neck (flexed DIP/hyperextended PIP), symmetrical, progress to large joints, acute synovitis Genetics: autoantibody binding to self-IgG FC receptor possibly genetic (HLA-DR4 and CTLA4 attacks the class two to make a pannus). TNF alpha/IL-1 bring more cells to the area to make the vessels leaky! CD4+cells play major role in B cell activation to make autoantibody and to activate Macs for more cytokines (Th17) Environmental: smoking can cause in influx of cells as well (TNFalpha, IL-1)) Pathophysiology Early RA: Initiation: in lymph node, macs make cytokines RF made in normal antibody making process. Breaking down the tolerance of immune system (of the T and B cells/tolerance fails from antigen presentation, deletion, receptor specificity, or differentiation to suppressive T lymphocytes). Propagation: immune complex enters and makes macs to make more cytokines, histamine release, B cell stimulation to make antibodies, tissue damage and pannus forms. This creates a type III hypersensitive reactions. Complement activation and recruitment of immune cells. There can be a problem with complement but also with phagocytosis (frustrated) so bad cleaning up of all the debris. Tissue damage: by cytokines making synovial fibroblast, OC and ROS. Autoantigens are from a clearance problem of apoptotic cells CTLA4 usually kills bad B cells so if it is mutated it will cause the B cell to persist TNFalpha, IL-1, IL-17 are most common cytokines. T cell CD4+ plays major roll in B cell activation to make autoantibody and for Macs to make cytokines Th17 major T cell with destruction and formation of inflammatory cytokines Reiter syndrome/Reactive Arthritis: conjunctivitis, urethritis, arthritis. pathophysiology: from molecular mimicry of HLA-B27 (Class 1). The body now begins attacking itself. Binds to other self and has to be initial insult and makes antibodies against it so it will begin to attack self. Needs infection first (chlamydia, salmonella, Yersinia) . Reactive arthritis: sausage fingers, coexisting articular infection. Asymmetrical peripheral large joints (weight bearing). 1-4 weeks after initial infection. The T regs rail at doing their jobosteoclast 1. X-ray is none diagnostic. Inflammatory joint fluid without identifiable organism. You will see conjunctivitis, UTI and skin infections! The links have to be close together. Anklyosing Sponyloitis: HLA-B27+, age less than 40 in males* (adolescent boys and young men), When we x-ray we look for sacroiliac joints Cardinal features: sacroilititis inflammation of SI joints, spondylitis inflammation of the spine, enthesitis inflammation of tendon insertion sites, uveitis inflammation of the eye . Systemic Lupus Erythematosus: no pearls on it but affects renal, CNS, vascular (Raynaud’s), cutaneous, pulmonary (pleuritic), cardiac (Libman Sacks endocarditis* sterile vegetation’s on the valve leaflet on echo onset murmur) La findings are titers of dsDNA antibodies. Need 4 of the 11 to have Lupus. susceptibility: C4 deficiency, HLA-DR3-2, defective immune complex clearance, drugs (temporarily induced). The autoantibody production is similar to RA. Immune complex clearance and apoptosis with C4 is similar problems. B cells become hyperactive and continuously secrete auto-antibody and T regs aren’t shutting down the auto immune response and cause production of pro inflammatory cytokines cellular markers: LE cells on the peripheral UV light, gender, infections, drugs, abnormal immune response, autoantibodies: DNA proteins (ANA/histones), type 3 hypersensitivity (watch kidneys), damaged systems attacks entire body. loss of tolerance to nuclear antigens (sle11, sel1b, sle1c), dysregulation (Far, TLR7) of immune system, disease FCG receptors, adhesion macs (allows cells to come in) treatment: NSAIDS, steroid, IV/oral steroids, hydroxychlorquine*, cyclophosphamide) Scleroderma: chronic systemic disorder by thickening of skin and has variable internal organ involvement with vasculitis and fibrosis of these organs. CREST: C-Calcinosis cutis R-Raynauds: spasm of BV to cold/stress E-Esophageal dysmotility S-Sclerodactylyl: thickening tightening of skin on the fingers T-Telagenietasias: dialation of capillaries causing red GI: esophageal dysmotility, reflux and watermelon stomach* Diagnosis is clinical based! marks on surface of skin Renal Crisis: malignant hypertensions/rapidly progressive acute renal failure (males, AA) Lab: ANA, Scl-1 anti tropisomerase I (most specific) anti centromere antibodies)’ Sjogren’s Syndrome: slowly progressive autoimmune disorder caused by lymphocytic infiltration of exocrine glands (primary SICCA and parotid enlargement). Has more dry eye and mouth without the other symptoms. Associated with HLA-B*8DRB1 (IFN alpha). You can have scleroderma with sjorgens but not vice versa. IFNalpha problems Clinical: Sicca (dry eyes/mouth), middle age females, extra glandular (arthralgia’s, Raynaud’s (vascular), GI (pancreatitis), lymphoma (higher risk) Labs: labial biopsy focal lymphocytic infiltration, abnormal tear flow shcirmers test, anti-Ro/SSA/SSB* and AntiLA/S Jacobasus lecture (26/27) MCL sprain/tear Testing in knee with 30 degrees of flexion and add valgus stress Mechanism: hyperextension and pushed valgus stress MCL injures can be treated with a brace. 3 grades to the injury. LCL sprain/tear testing with the knee in 30 degrees of flexion, you add varus stress, and you test by doing a figure 4 Mechanism: ACL tear: occurs during noncontact deceleration event that produces a valgus twisting injury. Meniscus tears occur with 50-75% of ACL tears. Extraarticular knee pain: prepatellar bursitis (anterior to the patella, no infectious aspirate/steroid injections and nsaids), Osgood-Schlatter (tibial tuberosity, young boys affects who kneecap moves requires immboilization), Bakers cyst (posterior, associated with meniscal tear)), cellulitis, skin infections Pes ansare bursa = medial side of knee. Distal to joint line. Protecting 3 tendons (Sartorius:femoral nerves, gracilis:obturator nerve, semitendinosus: tibial branch of sciatic nerve). It is a common cause of knee pain in older females/runners because the tendon insertion along the proximal tibial gest pulled out. There are rehab programs to do. Inframedial joint line plane. They can do exercises to help strengthen these muscles. Hemarthrosis = intra-articular swelling, poke a needle in there and suck on some blood. Could be ACL tear* (most are this) L tear, Tibial plateau fracture*, PCL, meniscal tear, intraarticular fractures, tear of joint capsule Osteochondrosus deficans : (complications) focal injury to bone and overlaying cartilage cause by a disruption of the blood supply Symptoms = adolescents and is extremely rare 15-30 people per 100,000. Micro fractures Signs = XRAYs show the size and location of the lesion on the femur Treatment = crutches, splinting or cast for a short period of time. If the lesion is separated or to large you go to surgery. Osteoarticular transformer (results encouraging, cell viability incomplete but maintained over time plugs, graft you need fresh chondrocytes Knee dislocation: most dislocation will have ACL, PCL, posterolateral corner and medial knee structures (MCL and posterior oblique ligament), medial/lateral meniscus, articular cartilage. Position of the tibia relative to femur gives us classifications. 1. 2. Anterior dislocation Posterior: anterior/posterior force (dashboard injury/high injury fall flexed knee) 3. Medial/lateral/rotatory *high incidence of popliteal artery injury and maybe the genicular artery, posterior tibial recurrent artery, sural artery. *posterior articular branches of tibial and obturator nerves for a posterior dislocation *anterior branches of femoral, common peroneal* and saphenous nerve *Common fibular nerve (winds around fibular head which can be injured during dislocation) * sciatic nerve splits into the tibial and common peroneal above the knee. Tibia nerve supplies the posterior side and common peroneal supplies anterior side (10-40%) can be injured with varus Lock-knee: meniscus tear. Meniscus only has blood supply to the periphery. Differential with posterior knee pain. Meniscus. Probably needs surgical repair. Meniscal tears and they cant bend because the meniscus is stuck. Extension located is a posterior tear of the meniscus. Cant bend it because of the severe pain and it gets stuck from that meniscus. posterior tear of meniscus: locked in extension Indications for knee arthroplasty 1. limited walking 2. attempted physical therapy, tried NSAIDS, injection, walker 3. limitations on daily activities of daily living 4. Acceptable medical risk Risk factors for tears 1. Age 2. Weight 3. Previous injury 4. Muscle imbalance in hamstrings and quads. The hamstrings decrease the ACL load by ruding the quadriceps induced anterior tibia translation 5. Limb alignment 6. Notch width: is less an women than it is in men. The ACL width correlates with the notch so the smaller the notch the thinner the ACL Don’t operate if no meniscus tear, no cartilage injury, low activity level prior to injury. Development of osteoarthritis as later complication of ACL deficient knees Lecture 28 – osteoarthritis Treatment (in order) * Reduction of Joint loading*: weight reduction, decrease in stressful activities, learning to work smarter, using devices to help Exercise, physical therapy (strength, aerobic, range of motions, agility, neck and back strength) Drug therapy: acetaminophen (stay under 3000), tramadol, NSAIDS (can cause ulceration/renal compromise), opioids Intraarticular therapies: corticosteroids, hyaluronic acid (Synvisc, Hyalgan) Aspirate knee* : sterile, gram stain negative, no inflammatory cells On x-ray* joint mice, joint narrowing in the medial compartment with subchondral sclerosis and osteophytes fingers: DIP and PIP, gleno-humeral joints, base of thumb (spared wrist elbow and ankle) Medial compartment will cause varus (bow leg) deformity Lateral compartment will cause valgus (knock knee) deformity Osteoarthritis: joint failure which is pathologic hyaline articular cartilage loss with increasing thickness and sclerosis of subchondral bony, osteophytes, stretching of articular capsule, mild synovitis, weakness of muscles bridging the joints, muscle degeneration. (type to collagen) Where is it? Knees, hips, C spine, L spine, first MTP joint, DIP/PIP, base of thumb wrist, elbow and ankle are spared. Heberdens nodes, bouchards node which develop gradually. Lecture 29 Disease Gender, Pathophysiology Diagnosis/Symptoms/Complications Age, Race LCPD Male 4:1, 3- Idiopathic osteonecrosis of proximal femoral Stage 2: Crest sign (fracture of necrotic 10 yo, epiphysis at secondary ossification center due subchondral trabeculae), and Gage sign (rat bite Caucasian to pressure changes in the capsule. Inc. at femoral head) pressure decreased blood flow to ischemia. Stage 3: Coxa magna due to premature physeal At sg 2 revascularization from periphery and arrest and hypertrophy of epiphyseal cartilage. as BF inc. areas are digested via granulation Symptoms: pain is achy, gradual, without trauma, tissue (cystic areas of bone). At sg 3 retender in hip and IR/ABd is restricted and painful, ossification begins at epiphysis, and antalgic gait. Galeazzi test (knees) distortion of femoral head may occur. Sg. 4 is Imaging: Bone scan will detect earlier remodeling resolution and new bone SCFE Male 1.5:1, 11-16 yo, AA Slipped capital femoral epiphysis, when forces applied to the femoral head exceed the strength of the epiphysis causing slippage. Ray reveals posterior displacement of femoral head. Can be bilateral. Hip, medial thigh, knee pain, acute/insidious onset (more pain associated) Diagnosis: radiology: instability of proximal femoral growth plate. Causes widening of hypertrophic zone up to 80% Classification: preslip, acute, acute on chronic, chronic (most common, not joint effusion). Treat with screw in hip. Transient Synovitis Male 4:1, 310 yo, Pain and lip most often seen after post infection, allergic reaction, post trauma. Has fever and ROM is limited Xray shows widening of joint space. MRI used to confirm diagnosis. Treat with limited activity, NSAIDS. Can progress to LCPD in 1-2% of cases. Can do ultrasound Lecture 30/31 Knee Anatomy and Key coronal view of MRI of the Knee Six main ligaments/cartilaginous structures (ACL/PCL/MCL/LCL/Lateral and medical meniscus). The menisci stabilize against rotation forces. The muscles of the knee are the vastus lateralis/medialis/intermedius, rectus femoris, biceps femoris, semitendinosus, semimembranosus, Sartorius, gracilis, IT bad, popilteus, and gastrocnemius. Popliteal fossa and popliteal artery gives off 5 genicular arteries (superior/inferior paired, middle). Collateral circulation to the knee are lateral femoral circumflex and anterior tibial arteries. The genicular arteries cannot compensate if a popliteal artery is ruptured. The tibial nerve joints the popliteal artery in the fossa but is not tethered to the knee. The peroneal nerve passes around the proximal fibula just distal to fibular head. Femoral head and neck injuries. Complication of femoral neck fracture = AVN because of the strong fibrous hip capsule there is a high rate of nonunion and avascular necrosis. Femoral head fractures are associated with posterior hip dislocations. Due to blood supply and strong fibrous hip capsule there is a high rate of a non union and AVN The major artery is the medial femoral circumflex artery to the femoral head that turns into its terminal branch the lateral epiphyseal artery Posterior hip dislocation can injure sciatic nerve. If the dislocation was anterior it would damage the femoral canal. Can be associated with posterior wall acetebaular fractures as well. Pelvic fracture complications hemorrhage (blood loss) occurs in 75% of pelvic fracture patients, urogenital and muscular skeletal pain Sacral Fractures: Divided into 3 zones. Zone 1: Vertical alar fractures. Osteoporotic stress fractures usually. The sacral ala up to the lateral border of neural foreman 5.6% of neural deficits (L5 root) Zone 2: Through the neural foramen has a 28.4% of neural deficits Zone 3: Central point of the sacrum and the canal, it’s a 56.7% of neural deficits. In the lumbar sacral plexus and neurological surgery Insufficiency fractures: 5% of all sacral fractures and is common in osteoporosis patients (elderly females). Tibial stress fractures occur because of fatigue fractures. The repetitive loading exceeds the bones capacity to remodel. Muscles of pelvis and hip Flexion: iliopsoas (Major/Minor Psoas, Iliacus) Extension: Glut max Abduction: glut med/min Adduction: add brevis, longus, magnus, pectineus, gracillis Ext rotation: in & ext obturator, quadratus femoris, sup/inf gemelli Int rotation: glut med & min Femoral Shaft fracture: vascular injury to femoral artery tether at adductor hiatus Most Common Avulsion Sites 1. Ischium: hamstring/adductor muscles 2. Anterior Superior Iliac Spine: Sartorius 3. Anterior inferior iliac spine: rectus femoris 4. Iliac crest: abdominals 5. Lesser trochanter: iliopsoas 6. Greater trochanter: Gluteus medius, gluteus minimus Salter harris classifications Type I Slipped: involves epiphyseal plate (only epiphyseal plate SCFE) Type II Above : involves epiphyseal, fracture of metaphysis Most common Type III Lower: fracture of epiphyseal plate and epiphysis itself Type IV Through : epiphyseal plate, fracture of metaphysis and epiphysis. Needs to be taken care of immediately V Rammed: involves epiphyseal plate Lecture 32/33 Developmental Dysplasia of the Hip: Increased ligamentous laxity of the hip capsule due to hormonal, mechanical and genetic factors Breech Position in 25% of the children Risks/Etiology: Crowding phenomenon, Congenital muscular torticollis, metatarsus adducts Neonate Testing: if there is clicking it’s a positive test o Barlow Tests: Barlow Barbarian. Dislocating the hip by adduction and applying gentle posterior force to hip o Ortolani Test: “Ortho-Ortolani”, reducing the hip by abduction and applying gentle anterior force to posterior thigh. Infant o Hip abduction test: baby on back up to 90 degrees. Under 60 is concerned and under 50 is diagnostic o Galeazzi Sign. Place the knees up and look at the height of the knees. o Asymmetry of thigh and gluteal folds: Asymmetry of thigh/gluteal folds. Diagnostic Testing o <4-6 months: Do ultrasounds as diagnostic testing and look at alpha angle o >4-6 months Xray to look for shenton line. Clinical findings: in toeing and limping (number 1 misdiagnosed DDH), waddling gain, leg length discrepancy, excessive lumbar lordosis Treatment o <6 mo: immobilization in Pavlik Harness start at 4 wks and do for 6. If no reduction after 3 weeks go to Spica o >6 mo-2 yo: Spica cast done in general anesthesia. Use CT/MRI to check o Surgery: If closed reduction fails. <2 y/o do open reduction no osteotomy. If >2 yo: do open reduction and osteomoty. Complications: Avascular necrosis Congential Disorders of Lower Extremity Disorder Age Symptoms/Testing Treatment Internal Femoral Torsion >2/yo W sitting, patella pointed inwards, internal Observation Femoral Anteversion rotation. In Toeing Test: Hip rotation degree angle lay on abdomen and IR >70 degrees/limited external (10-20) Internal Tibial Torsion < 2 yo Patella’s say forward. Resolve Test: Thigh foot angle measure inward value. Will spontaneously have a negative angle. In Toeing Genu Varum (Bowlegs) Physiological: crowding. Same as ITT, no intoeing Physiological: fixes Blount’s Dz: abnormal growth of medial aspect of itself proximal tibial physis. Sloping, peaking, widening, Physiological: fragmentation. African Americans, adolescents depending on age, *Xray to differentiate. Blunts has asymmetric, stage and nature. abrupt sharp angulation and off angle Osteomoty (op) Genu Valgum (knock 3-5 Physiological Resolution btwn 5knees) yo Rare causes: infection tumor, renal, 8 yo. Surgery if bad osteodystrophy, cerebral palsy* Ankle/Foot Disorder Metatarsal Adductor Calcaneovalgus foot Talipes Equinovarus Club foot Symptoms/Testing Convex lateral foot concave medial foot. DDH test (2%) Forefoot is adducted, midfoot and hindfoot are normal. In toeing Testing: finger V test, xray increased angle btwn 1-2 MT Hyperdosiflexion, forefoot abduction, heel valgus Xray differentiate from congenital vertical talus (rockerbottom) C: Cavus (planter flexion) (FF) A: Adduction of forefoot/midfoot on hindfoot (FF) V: Varus of hindfoot (HF) E: Equnus of hindfoot (HF) Multifactorial, family history Congential: 75%, breech, AP/lateral 30 deg plantar flexion Treatment Depends on rigidity. To neutral: stretch, opposite shoes Cannot to neutral: cast Failure Surgery Reassurance, stretching, rare serial casting Nonsurgical: casting changed 1-2 weeks and achieved by 3 months. Followed by bracing Surgery is easy if needed (failure by 3 mo) Congenital Vertical Talus Rocker bottom foot 40% neuroMSK/ 60% unknown Talar head prominent at med border of midfoot, forefoot and midfoot are dorsiflexed *Trisomy 18 Edward Syndrome (overlapping fingers) Tarsal Coalitions 2+ bones in mid/hindfoot are joined. Decreased joint motion, pain, flat foot, ankle sprains Talonavicular (3-5 y), Calcanonavicular (8-12y), Talocalcaneal (12-15 y). CT Scan! Absence of arch. Medial longitudinal arch laxity. While sitting arch is present when standing its gone. (protonation) Neuromuscular! Elevation of longitudinal arch Pes Planus Pes Cavus Serial manipulation/casting after birth Surgery at 6-12 mo Casting then orthosis postoperatively Non-operative: shoe inserts, casting Surgical: arthritis Resolution by 6 mo or have rest of life. Use shoe inserts stretch