* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download To know
Hypothyroidism wikipedia , lookup
Hypoglycemia wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Graves' disease wikipedia , lookup
Metabolic syndrome wikipedia , lookup
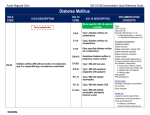
Epigenetics of diabetes Type 2 wikipedia , lookup
Diabetes mellitus wikipedia , lookup
Gestational diabetes wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Diabetes management wikipedia , lookup
Diabetic ketoacidosis wikipedia , lookup
Diabetes mellitus type 2 wikipedia , lookup
MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 1. DIABETES MELLITUS AND PREGNANCY. THE PREGNANCY FOR THE DIABETIC PATIENTS. FEATURES IN THE TREATMENT OF DIABETES MELLITUS TREATMENT IN PREGNANT WOMEN. IFNMU 2010 Actually Diabetes mellitus in pregnant women may be pregestational, where the diabetes mellitus (type 1 or type 2) was diagnosed before pregnancy, or gestational, which refers to diabetes mellitus diagnosed during pregnancy. Gestational diabetes accounts for 88 percent of diabetes mellitus in pregnancy, type 2 diabetes mellitus comprises 8 percent, and type 1diabetes mellitus makes up the remaining 4 percent. Complications are minimal in infants of mothers with gestational diabetes. In contrast, hyperglycemia-induced teratogenicity occurs almost exclusively in pregestational diabetes. The most difficult pregnancies for the mother and fetus occur in diabetic women with renal, cardiac, or retinal disease. Study aim To know: 1. To know terms and definition of gestational diabetes mellitus. 2. To know how to determine the diagnosis of gestational diabetes mellitus. 3. To know how to determine the criteria for either low risk or high risk development of gestational diabetes mellitus. 4. To know classification of fetal complications for maternal diabetes mellitus. 5. To know about maternal risks in diabetic pregnancies. 6. To know fetal complications of maternal pregestational diabetes mellitus. 7. To know causes of fetal illnesses and death. 8. To know contraindication to pregnancy for patients with diabetes mellitus. 1. 2. 3. 4. 5. 6. To be able: To be able to prevalence of pregestational diabetes in pregnant women. To be able to interpreted diagnostic criteria of gestational diabetes mellitus. To be able to define pregnant women with the high risk of development of diabetes mellitus. To determine a plan of treatment for pregnant patients with diabetes mellitus. To be able to determine a plan of fetopathy monitoring. To conduct the correction of insulin therapy during births and postpartum. Base knowledges, abilities, skills, necessary are studying themes. Discipline Path. Physiology Gynaecology Paediatrics To know To be able Features of exchange processes are in the organism of woman in different periods of To estimate the state of compensation diabetes mellitus. pregnancy. Role of carbohydrate changes. State the diagnostic criteria for the gestational diabetes mellitus. The pregnant have requirements to control of level of blood glucose. To know the complications of mother with diabetes mellitus and her child. To conduct the correction of glucose in the blood, control for sight, ECG and body mass index in the pregnant women with diabetes mellitus To be able to conduct a woman with diabetes mellitus in births. Influence of pregnancy is on mental and physical development of child. To know about causes of fetal illnesses and death. To be able to determine a plan of fetopathy monitoring. Assessment questions: 1. Define gestational diabetes mellitus (GDM). 2. Describe the metabolic changes associated with the development of GDM. 3. List one potential risk of GDM on the fetus and one on the mother. 4. State the diagnostic criteria for the individual with GDM. 5. Propose the algorithm of diagnosing of GDM. 6. List one component of medical nutrition therapy for the individual with GDM. 7. State the criteria for initiating insulin as treatment for the individual GDM. 8. State two recommendations for post-partum care for GDM. 9. Clinical features of Diabetes Mellitus in pregnant women. 10. Features of the course of Diabetes Mellitus in pregnancy. 11. Treatment of Diabetes Mellitus in pregnant women in different stages of the disease. 12. Features in the treatment of Diabetes Mellitus treatment in pregnant women. 13. Build the scheme of treatment for pregnant women with diabetes mellitus. Self-assessment examination: # 1. Which of the following statements is not true regarding gestational diabetes mellitus (GDM): A. GDM affects up to 14% of pregnancies B. Symptoms of GDM include increased thirst and frequent urination C. GDM is typically found in the third trimester D. If undetected, GDM can harm the mother and fetus # 2. Patient J. is a 24 year old woman. Her health care provider just confirmed she is 14 weeks pregnant. This is her first pregnancy. She has a family history of diabetes and is overweight. What is her risk assessment? A. Low risk status. No need to test blood glucose levels B. Average risk status and should be screened at 24-28 weeks C. High risk status and should be screened at 24-28 weeks D. High risk status and should be screened at this visit E. High risk status and should be screened at this visit and at 24-28 weeks # 3. Which of the following is a fetal complication associated with GDM? A. The infant will have hyperglycemia at birth B. Pre-eclampsia C. Macrosomia D. Polyhydraminos # 4. Based on the following oral glucose tolerance test (GTT) results, which individual with the following test results would be diagnosed with GDM? A. Fasting: 4,9 mmol/L, 1 hour: 10,3 mmol/L, 2 hour: 8,6 mmol/L, 3 hour: 6,4 mmol/L B. Fasting: 5,2 mmol/L, 1 hour: 9,9 mmol/L, 2 hour: 8,6 mmol/L, 3 hour: 7,7 mmol/L C. Fasting: 4,6 mmol/L, 1 hour: 8,6 mmol/L, 2 hour: 6,2 mmol/L, 3 hour: 4,7 mmol/L D. Fasting: 4,8 mmol/L, 1 hour: 10,8 mmol/L, 2 hour: 9,4 mmol/L, 3 hour: 7,7 mmol/L E. Fasting: 3,6 mmol/L, 1 hour: 9,9 mmol/L, 2 hour: 6,9 mmol/L, 3 hour: 5,9 mmol/L # 5. In which situation should urine ketones be tested? A. When nauseated and vomiting B. 2 hours after every meal C. When fasting blood glucose levels are less than 3,9 mmol/L D. All of the above # 6. All of the following statements are true regarding insulin except: A. Insulin needs are higher in the third trimester than in the first B. Insulin needs are based solely on the fetal weight C. Women with GDM requiring insulin should be educated on signs and symptoms of hypoglycemia D. Insulin therapy is recommended when the meal plan and activity alone are unable to adequately control blood glucose levels # 7. Post-partum counseling should include: A. Elimination of all carbohydrates from the meal plan to facilitate weight loss B. Avoidance of all oral contraceptive because they elevate blood glucose levels C. Encouraging breastfeeding only for obese women to help them lose weight D. Follow up with blood glucose testing at 6-week checkup E. All of the above # 8. What kind of complications for diabetes mellitus in women is pregnancy contraindicated? A. Background retinopathy B. Maculopathy C. Proliferative retinopathy D. Neuropathic form of diabetic foot E. Diabetic neuropathy # 9. Principles of treatment for pregnant women with diabetes mellitus are include: A. Diet and insulin therapy B. Oral antidiabetic drugs C. Combinations of insulin therapy with oral antidiabetic drugs D. Only insulin therapy E. Diet # 10. What are preconditions must be preceded conception at women with diabetes mellitus? A. Good and protracted compensation of diabetes mellitus B. Good compensation of diabetes mellitus is on the day of conception C. Only absence of glucosuria D. Permanent indexes of metabolism are within the limits of norm E. Not to use carbohydrates Case # 1. A 30 year old woman booked into the clinic at 17 weeks gestation. She was 165 cm tall and weighed 55,8 kg. Uterine ultrasound confirmed the gestational age and was otherwise unremarkable. She complained of vaginal thrush and on routine testing had “++” glycosuria. There was no polydipsia or polyuria. She had a past medical history of an operation for hiatus hernia at the age of 9 months. There was no relevant family history. The thrush was treated. At 28 weeks gestation, she presented to again with pre-term labor. She was noted to have marked polyhydramnios (an excess of amniotic fluid). She considered the polyhydramnios to be due to gestational diabetes mellitus and performed a 75 g glucose tolerance test: Time (min) Serum glucose concentration (mmol/L) 0 6,6 30 14,0 60 15,4 90 8,1 120 7,7 Question 1: Were correct in diagnosing gestational diabetes mellitus? Question 2: If not, how may the glucose tolerance test be interpreted? Question 3: How would you have treated the patient at the time of the presentation at 28 weeks gestation? Case # 2. Patient T., 28 year old with type 1 diabetes mellitus of 5 years duration was seen in the clinic. Daily doses of insulin - 46 IU. She’s pregnant 16 weeks. During flu nausea, vomit, somnolence. The sick in the evening gave up a meal, did’t get the duty dose of insulin, and unconsciousness a morning. Objectively: sick without consciousness, a skin is dry. Strong smell of acetone from a mouth. Temperature - 36.6°, pulse – 100 beats per minute, weak; blood pressure (BP) is 90/50 mmHg. Lab studies: The reaction of the urine to acetone is positive (+++). The glucose in blood - 23 mmol/L. Question 1: Substantiate diagnosis. Question 2: What therapy is needed first of all? Standards of answers to the self- assessment examination. Theme # 1. Diabetes Mellitus and pregnancy. The pregnancy for the diabetic patients. Features in the treatment of Diabetes Mellitus treatment in pregnant women. 1. 2. 3. 4. 5. Tests C. E. C. B. D. 6. C. 7. E. 8. C. 9. A. 10. A. Case # 1. Answer 1: Diagnosis of gestational diabetes mellitus is correct. Answer 2: The oral glucose tolerance test interpreted - gestational diabetes mellitus. Answer 3: Insulin therapy. Case # 2. Answer 1: Type 1 diabetes mellitus, moderate form, the state of decompensation. Diabetic ketoacidotic coma. Pregnancy 16 weeks. Answer 2: Intensive insulin therapy. Rehydration and electrolyte balance recovery. Detection and treatment of concomitant diseases. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 7. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. SUPPLIMENTARY REFERENCES: 1. The Diabetes Control and Complications Trial Research Group: Effect of pregnancy on microvascular complications in the Diabetes Control and Complications Trial. Diabetes Care 2000, 23: 1084–1091. 2. Loukovaara S., Immonen I., Teramo K.A., Kaaja R.R. Progression of retinopathy during pregnancy in type 1 diabetic women treated with insulin lispro // Diabetes Care. – 2003. - 26:1193–1198. 3. Larsen M., Colmorn L., Bonnelycke M., et al. Retinal artery and vein diameters during pregnancy in diabetic women / Invest Ophthalmol Vis Sci. – 2005. - 46: 709–713. 4. Diabetic Retinopathy. Preferred Practice Patterns [pamphlet]. San Francisco, C.A.: The American Academy of Ophthalmology; 2003. 5. American Diabetes Association, “Gestational Diabetes Mellitus,” Clinical Practice Recommendations 2004: Diabetes Care, Jan. 2004; Volume 27, Supplement 1. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 2. DIABETES MELLITUS IN CHILDREN. FEATURES IN THE COURSE OF DIABETES MELLITUS IN CHILDREN. MAURIAC SYNDROME AND NOBEKURA SYNDROME. IFNMU 2010 Actually Diabetes mellitus is typically perceived as a disorder of older adults; however, diabetes occurs in 1 out of 600 children under 18 years of age, and the incidence appears to be increasing. Unless children with diabetes mellitus are diagnosed promptly and treated appropriately, they are at serious risk for acute and long-term complications. Mauriac syndrome, also known as diabetic dwarfism, is a complication of diabetes mellitus that causes enlarged liver, short stature and delayed puberty in children. The cause of the disorder is believed to be related to low levels of insulin, inadequate diet and diabetes mellitus that has been poorly controlled over a long period of time. It occurs most often in children, teens or young adults with type 1 diabetes mellitus. Study aim To know: 1. To know terms and definition of Diabetes Mellitus in children. 2. To know about peculiarity in development of Diabetes Mellitus in children. 3. To know definition of Mauriac syndrome and Nobekura syndrome. 4. To know causes of Mauriac syndrome and Nobekura syndrome. 1. 2. 3. 4. 5. To be able: To be able to prevalence of Mauric’s syndrome in children. To be able to interpreted diagnostic criteria of type 1 and type 2 Diabetes Mellitus in children. To be able to define children with the high risk of development of type 2 Diabetes Mellitus. To determine a plan of treatment for children with type 1 Diabetes Mellitus. To be able to determine a plan of glicemic control and lipid profile in children with type 2 Diabetes Mellitus. Base knowledges, abilities, skills, necessary are studying themes. Discipline Path. Physiology Children diseases Pharmacology To know Mechanism of interaction between hormones, pathogenesis of Diabetes Mellitus in children. To be able To examine glucose in blood and urine and acetone in urine. Carbohydrate, lipid and protein metabolism in the children body. To diagnose type, state, and stage of difficulty of Diabetes Mellitus in children. Structure of visual analyzer clinical symptoms of Diabetes Mellitus in children. Differential diagnosis and treatment of Diabetes Mellitus in children. To choose an adequate and appropriate type of treatment of Diabetes Mellitus in children. Assessment questions: 1. Definition of term “Diabetes Mellitus” in children. 2. Epidemiological aspects of type 1 and type 2 Diabetes Mellitus in children. 3. The role of virus infection in Diabetes Mellitus in children development. 4. The role of autoimmune process and other damage factors of the pancreas in Diabetes Mellitus in children development. 5. Pathogenesis of type 1 and type 2 Diabetes Mellitus in children. 6. Stages of severity of Diabetes Mellitus in children, diagnostic criteria of each stage. 7. The main signs and symptoms of Diabetes Mellitus in children and pathogenesis of them. 8. Pathogenetic mechanisms of development of chronic complications of Diabetes Mellitus in children. 9. Definition of Mauriac syndrome and Nobekura syndrome. 10. Etiology and pathogenesis of Mauriac syndrome and Nobekura syndrome. 11. The main principles of Diabetes Mellitus in children therapy. 12. Treatment of chronic complications of Diabetes Mellitus in children. Self-assessment examination: # 1. Determining which type of diabetes mellitus a child has may be difficult because: A. The signs and symptoms of each type may be similar B. Recognition of the signs and symptoms is difficult C. No exact lab test exists that can differentiate between them D. Children are not reliable in reporting the signs and symptoms # 2. Initially, insulin dosages in children are determined primarily by: A. The child’s age B. The child’s weight C. The physician’s preferences D. How high the blood glucose was during the evening E. The level of ketone bodies and child’s weight # 3. A child of ten years with diabetes mellitus of age could probably be expected to: A. Be totally responsible for the management of the condition B. Be able to check the blood sugar and record it accurately C. Give insulin injections in an independent manner D. Prepare appropriate meals # 4. The recent increase in type 2 diabetes mellitus in children is thought to be a response to which of the following? A. Diets high in fats and carbohydrates, combined with a sedentary lifestyle B. A hereditary predilection for this type of diabetes mellitus C. Ungrounded fears about diabetes mellitus D. Better detection and diagnostic methods # 5. In a child with diabetes mellitus, if the morning fasting blood sugar is consistently elevated, which insulin should be adjusted? A. The a.m. short-acting insulin B. The a.m. intermediate (rapid) acting insulin C. The p.m. short-acting insulin D. The p.m. intermediate (rapid) acting insulin # 6. In beginning education for the child and family who have just received a diagnosis of diabetes mellitus, the educator should first determine: A. The age of the affected child B. The family history of diabetes C. The child’s past medical history D. What the child and family already know about diabetes mellitus # 7. The mother of a 14 year old girl complains that her daughter’s blood sugar values are frequently elevated. She accuses the child of cheating on her diet plan. The best response would be to: A. Discuss possible insulin resistance during puberty B. Agree with the mother that her suspicions are probably true C. Check the blood glucose yourself to see if it is elevated D. Lecture the child on the importance of being honest about what she has eaten # 8. The child with diabetes mellitus who is involved in athletic activities should observe which of the following recommendations? A. Not to exercise when the insulin is peaking B. To give additional insulin before exercise to meet the body’s metabolic demands C. To check the blood sugar level one hour after exercising D. To have a snack before or during strenuous exercise to prevent hypoglycemia # 9. A 18 years old man is diagnosed with diabetes mellitus. Which of the following findings would point most convincingly to type 1 rather than type 2 diabetes? A. He is not obese B. Severe polydipsia and polyuria preceded the diagnosis C. Ketoacidosis was present at the time of diagnosis D. The serum C-peptide level was normal at the time of diagnosis E. Glucose levels rose above 32 mmol/L before treatment was started # 10. A 21 years old female is diagnosed with diabetes mellitus. Type 1 diabetes mellitus is usually associated with which one of the following? A. Onset in middle age B. Obesity C. Insulin resistance D. Requirement for insulin therapy E. Absence of autoimmune manifestations # 11. In a boy of 5 years, after measles vaccination a temperature of the body is 37,8 0C, a big thirst, polydipsia, polyuria. Weakness is increasing during 6 hours from the beginning of the disease, noisy breathing, sleepy. Your preliminary diagnosis: A. Type 1 diabetes mellitus B. Postvaccination syndrome C. Typical postvaccination reaction D. Postvaccination allergy E. Non of this variant # 12. A 9 year old boy had acute respiratory viral infection. After it there appeared polydipsia, polyuria, weakness, nausea. Examination revealed the following symptoms: mental confusion, dry skin, soft eyeballs, Kussmaul's respiration, acetone smell from the mouth, muffled heart sounds, soft and painless abdomen. Blood sugar was 19 mmol/L. What acute condition is it? A. Ketoacidotic coma B. Hepatic coma C. Cerebral coma D. Acute renal insufficiency E. Hyperosmolar coma Case # 1. A male, 19 years old with type 1 diabetic mellitus. In past history of multiple admissions to intensive therapy unit (ITU) with diabetic ketoacidosis (DKA) in a period of 3 years was admitted to ITU with DKA. On his examination protuberant abdomen with hepatomegaly, normal BMI and growth impairment were seen. His sexual development was normal. He had background diabetic retinopathy. Labaratory: НвА1C 10.9%. His renal function was normal. Liver function test showed ALP, ALT and total bilirubin raise in 1.5 times. Your preliminary diagnosis. Standards of answers to the self- assessment examination. Theme # 2. Diabetes mellitus in children. Features in the course of Diabetes Mellitus in children. Mauriac syndrome and Nobekura syndrome. 1. 2. 3. 4. 5. 6. A. E. B. A. D. D. 7. B. 8. D. 9. C. 10. D. 11. A. 12. A. Case # 1. Type 1 Diabetes Mellitus. Mauriac syndrome. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 7. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. SUPPLIMENTARY REFERENCES: Manual of Endocrinology and Metabolism edited by Norman Lavin. Lippincott Williams & Wilkins. 2009. – 837 p. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 3. METABOLIC SYNDROME IFNMU 2010 Actually The contemporary definition of the Metabolic Syndrome refers to a cluster of metabolic abnormalities related to a state of insulin resistance which is often associated with a high-risk overweight/obesity phenotype. Because such cluster increases the risk of coronary heart disease (CHD) and type 2 diabetes mellitus, numerous consensus groups have attempted to provide recommendations to identify in clinical practice patients with these atherogenic/diabetogenic metabolic abnormalities. Study aim To understand the various theories of Metabolic Syndrome development and research studies that support these theories. To know about the etiology, pathogenesis and clinical presentation of Metabolic Syndrome. To know: 1. To know about definition of Metabolic Syndrome (Syndrome X, Insulin Resistance Syndrome). 2. To know about pathogenesis of insulin resistance. 3. To determine the diagnosis of Metabolic Syndrome and build the scheme of clinical and laboratory diagnostic. To be able: 1. To find out the clinical and laboratory criteria of the Metabolic Syndrome. 2. To be able to conduct differential diagnostics between of the Metabolic Syndrome and cardio metabolic syndrome. 3. To be able build the scheme principle of treatment of Insulin Resistance Syndrome. Base knowledges, abilities, skills, necessary are studying themes. Discipline Path. Physiology Internal medicine Pharmacology 1. 2. 3. 4. 5. 6. 7. 8. 9. To know To be able Mechanism of interaction between To explain the action of antagonists of insulin, violation, at cellular level insulin resistance and compensate (defect of receptors) and postreceptor hyperglycemia; levels. Mechanisms of development of atherosclerosis. Causes of development of cardio vascular To explain the role of risk factors for diseases and hypertension. development of metabolic syndrome. Pharmacology effects of oral antidiabetic To conduct the correction of drugs, antihypertension medicine and dyslipidemia, hypertension and other lipidmodifications therapy. metabolic changes. Assessment questions: Definition of Metabolic Syndrome (MS). The role of insulin resistance and hyperinsulinemia in pathogenesis of MS. The diagnostic criteria of MS. Build the scheme of pathogenesis of MS. Name three laboratory values that indicate possible MS. Define insulin resistance (IR). Discuss the two most serious consequences of developing MS. Describe two major lifestyle changes that can help treat and prevent MS. Treatment approaches to MS. Self-assessment examination: # 1. Insulin resistance is: A. Fear of changing from oral medications to insulin injections B. Abnormal difficulty body cells have in using insulin C. Abnormal difficulty beta cells have in making insulin D. The difficulty kidneys have in secreting insulin # 2. Insulin resistance can be caused by: A. Excessive thirst (polydipsia) B. Excessive urination (polyuria) C. Excess visceral fat D. Excessive sweating # 3. Weight loss for people with metabolic syndrome: A. Cannot be recommended if the person has heart or kidney disease B. Can reduce insulin resistance C. Is generally dangerous to the person's general health D. Is the least important lifestyle change # 4. A high level of blood cholesterol: A. Protects people with type 2 diabetes mellitus from kidney damage B. Lowers the risk of cardiovascular disease C. Is not a problem unless people also have hypertension D. Is a type of dyslipidemia # 5. In people with type 2 diabetes mellitus, hypertension: A. Doubles the risk of developing cardiovascular disease B. Occurs rarely C. Increases the risk of neuropathy but not of cardiovascular disease D. Cannot be controlled # 6. People with metabolic syndrome need to: A. Use protein as their main source of calories B. Reduce proteins to less than 10% of total calories C. Choose bacon, steak, sausage, and ground beef as potent protein sources D. Get their protein from poultry, fish, cheese, and soy products # 7. Hyperinsulinemia is: A. Decreased sensitivity to the action of insulin B. Elevated levels of plasma insulin C. Elevated blood glucose levels D. Elevated blood glucose levels and levels of plasma insulin E. Insulin resistance # 8. Metabolic syndrome is a cluster of problems including impaired fasting glucose, dyslipidemia, and: A. Hyperadrenalism B. Hypercapnia C. Hyperthyroidism D. Hypertension E. Hypercortisolemia # 9. The patient Q., 53 years old during random checkup has the fasting level glycemia – 8,2 mmol/L, the glucosuria – 1,5 g/L. Body height -172 cm, body weight - 106 kg. Body mass index – 35,8 kg/m2. Define initial tactics of treatment: A. Insulin B. Biguanides C. Diet with carbohydrate restriction D. Sulfonylureas of 1 generation E. Sulfonylureas of 2 generation # 10. The patient W., 66 years old, the diabetes mellitus is revealed random during checkup. It was not treated. Objectively: body height - 170 cm, weight -112 kg. Body mass index – 38,8 kg/m2. Ps - 76 /minutes, regular. The blood pressure - 160/90 mm Hg. The fasting level of glycemia – 8,2 mmol/L. What is primary tactics of treatment: A. Diet recommendations B. Prescribe Repaglinide C. Prescribe Metformin D. Prescribe Glibenklamide E. Prescribe Insulin # 11. Which of the following is associated with the use of prescription omega-3 fatty acids for dyslipidemia? A. Bleeding B. Hypervitaminosis C. Reduction in LDL (low density) cholesterol D. Reduction in triglycerides # 12. Which of the following statements about the use of lipid-modifying drug therapy is correct? A. Empiric dosage reductions should be made for all agents in the elderly solely on the basis of age B. Empiric dosage reductions should be made for selected agents in the elderly solely on the basis of age C. Empiric dosage reductions should be made for selected agents on the basis of renal insufficiency in patients of all ages D. Empiric dosage reductions should be made for selected agents on the basis of renal insufficiency only in the elderly # 13. Which combination of metabolic syndrome criteria can be used to estimate future risk of chronic heart disease (CHD), cardiovascular mortality, and all-cause mortality in women? A. Triglyceride level and waist circumference B. HDL (high density) level and waist circumference C. Triglyceride and HDL (high density) levels D. HDL (high density) level and blood pressure E. Triglyceride level and blood pressure # 14. The body shape most closely associated with metabolic syndrome is: A. Gynecoid (pear shaped) B. Ovoid (egg shaped) C. Android (apple shaped) D. Droid (star shaped) # 15. Which pair of serious health problems are the most common results of metabolic syndrome? A. Colon cancer and stroke B. Coronary heart disease and type 2 diabetes mellitus C. Pulmonary hypertension and portal hypertension D. Breast cancer and prostatic cancer Standards of answers to the self- assessment examination. Theme # 3. Metabolic syndrome. 1. 2. 3. 4. 5. 6. 7. B. C. B. D. A. D. B. 8. D. 9. C. 10. A. 11. D. 12. C. 13. B. 14. A. 15. B. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 7. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. SUPPLIMENTARY REFERENCES: 1. Grundy S.M., Brewer H.B., Jr., Cleeman J.I., Smith S.C., Jr., Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433-438. 2. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497. 3. Lakka H.M., Laaksonen D.E., Lakka T.A., et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002; 288:2709-2716. 4. Laaksonen D.E., Lakka H.M., Niskanen L.K., Kaplan G.A., Salonen J.T., Lakka T.A. Metabolic syndrome and development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am. J. Epidemiol. 2002;.156:1070-1077. 5. Mc.Cormack J. New approaches to treat insulin resistance. In Symposium: Targeting Insulin Resistance and Defective Insulin Secretion. Presented at the 18th International Diabetes Federation Congress; August 24-29, 2003; Paris, France. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” THEME # 4. THE SURGICAL TREATMENT FOR DIABETIC PATIENTS. IFNMU 2010 Actually There is a permanent increase of amount of patients with diabetes mellitus, frequent development of complications, which quite often are completed lethally, require implementation of surgical interferences. Therefore knowledge of mechanisms of development of features of clinical picture of disease, pathogenic therapy of the exigent states, will provide the rational passing to treatment of patients with diabetes mellitus and concomitant surgical pathology. Study aim To know: 1. To know pathogenesis in development of surgical complications in patients with diabetes mellitus 2. To know to receive the planned surgical treatment of patients with diabetes mellitus 3. To know about methods of anaesthetizing, which apply at small and large operations for patients with diabetes mellitus To be able: 1. To be able to conduct differential diagnostics of surgical complications of diabetes mellitus with nosology of other etiology 2. To be able to execute complex therapy for patients with diabetes mellitus and surgical pathology 3. To be able to choose the methods of anaesthetizing for every patient 4. To be able to warn possible complications at implementation of surgical interferences for patients with diabetes mellitus Base knowledges, abilities, skills, necessary are studying themes. Discipline Path. Physiology Surgery Fist aid and anaestheology To know To know about pathological mechanisms of development surgical complications in patients with diabetes mellitus. To know about pathophysiological mechanisms of tissues regeneration in patients with diabetes mellitus. To find out the pathological links of mechanism with the purpose of setting of pathogenic treatment. To know new methods of treatment of surgical pathology in patients with diabetes mellitus. To conduct differential diagnostics of surgical complications of diabetes mellitus with similar nosologies of other etiology. To choose the method of surgical interference. To know principles of anaesthetizing for patients with diabetes mellitus and surgical pathology. To know principles of complex therapy of the exigent states are at diabetes mellitus. To be able To conduct surgical preparation of patient with diabetes mellitus. To provide the correction during an operation and after that. Assessment questions: 1. To know about surgical complications of diabetes mellitus and tell about the pathological mechanisms of their development. 2. To conduct differential diagnostics of veritable “sharp stomach” and diabetic pseudoperitonitis. 3. To describe the features of flowing of sharp festering-inflammatory diseases on a background diabetes mellitus. 4. To describe the role of violations of the immune system for patients with diabetes mellitus and concomitant hyperthyroidism and features of surgical preparation of such patients. 5. To tell for violation of stasis of blood for patients with diabetes mellitus and concomitant surgical pathology. 6. To describe the clinical picture of diabetic gangrene and diabetic osteoartropathy. To know methods of their diagnostics and treatment. 7. To build the scheme of surgical preparation of patient with diabetes mellitus. 8. To transfer contraindication to implementation of surgical interferences for a patient with diabetes mellitus. 9. To describe facilities of complex medicinal therapy, which apply for the correction of the broken metabolism during surgical treatment. 10. To tell about influence on the carbohydrate exchange of accumulated drugs of different pharmacological groups. 11. To transfer possibilities of complication, which arise up for patients with diabetes mellitus after surgical preparation, and measures, for their warning. Self-assessment examination: # 1. At suspicion on diabetic pseudoperitonitis which from the indicated examination will you do fist of all? A. Determination of glycemia B. Determination of glucosuria C. Determination of ketone body in urine D. Determination of activity of alpha amylase E. Determination of leukocytosis # 2. Patient 21 years of age, suffering from diabetes mellitus for 2 years. Compensation of diabetes mellitus is not satisfactory. Complains that turned blue feet, chilliness in both legs. Objective review: foot cold to the touch, bluishred color on the little finger of both feet ulcer with pus. Ripple in the dorsal arteries of the foot is good. Substantiate diagnosis: A. Diabetes mellitus type 1, neurotrophic ulcers B. Diabetes mellitus type 1, diabetic microangiopathy and macroangiopathy low extremites C. Diabetes mellitus type 1, diabetic ishemic angiopathy low extremites, diabetic gangrene D. Diabetes mellitus type 1, acute diabetic foot ulcers # 3. How to treat diabetic blister? A. Immediately cut, cut the epidermis and put a bandage poluspirtnuyu B. Immediately cut, cut the epidermis and put a bandage with an antiseptic solution C. Immediately cut, cut the epidermis and put dry aseptic bandage D. Remove the syringe contents puhirya and put dry aseptic bandage E. Do not shoot blister, put a gauze bandage on it and recommend shoes that do not sting blister # 4. Which listed symptoms distinguish diabetic ketoacidosis with clinic "acute abdomen" from present "acute abdomen"? A. Availability acetonuria B. Vomiting precedes pain C. Indeterminate localization pain D. Reducing pain in result of intensive therapy diabetic ketoacidosis E. Impetuous development symptoms # 5. Abdominal pain with ketoacidosis predetermined: A. Enhanced peristalsis of small intestine B. Loosening of peristalsis of the colon C. Violation egestion function of the pancreas D. Increasing the stomach E. Paresis of the ileum Clinical cases Case 1. Male 23 years old, suffers from type 1 diabetes mellitus. During the party with friends did not impose insulin. On the second day began to disturb nausea, vomiting, a bulging belly. Feebleness. Caused by the ambulance. The patient reported that he suffers from diabetes. Emergency doctor decided to hospitalize the patient to the duty surgical department with a diagnosis of acute pancreatitis. What is substantiate diagnosis in patient? Case 2. In the surgical department of hospitalized patients 46 years old and diagnosed with exacerbation of chronic cholecystitis. From history we know that the patient suffers from diabetes mellitus type 2. Treatment by maninil a dose of 20 mg per day. Diets are not followed. Glycemia, usually within 15-17 mmol / L. The last week did not take maninil and significantly violated diet. Objective review: contact, slightly inhibited, accelerated respiration, noisy, sharp smell of acetone in the air. Pulse - 142 beats/ min. In order to prepare for the surgery the patient is assigned: 10% glucose solution 500.0 ml of sodium chloride 0.8% to 500,0 ml. Insulin 32 IU. Do you think that if this therapy requires correction? Case 3. Patient 50 years preparing for operations in connection with calculous cholecystitis. 5 years suffering from diabetes mellitus, treated maninil 3 tables / day. Fasting blood glucose - 5,5 mmol / L. Glycosuria abstent. What treatment should be nominated? Case 4. Type 2 diabetic patients suffering carbunculosis. Could this serve as indications for insulin therapy? Standards of answers to the self- assessment examination. Theme # 4. The surgical treatment for diabetic patients. 1. 2. 3. 4. 5. Answers the tests: C. C. E. A. E. Answers the clinical cases: CASE 1. Diabetic psevdoperitonit. CASE 2. The patient needs intensive care because of her diabetic ketoacidosis. CASE 3. Insulin therapy. CASE 4. Insulin therapy. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 7. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. 1. 2. 3. 4. 5. SUPPLIMENTARY REFERENCES: Novella S.P., Inzucchi S.E., Goldstein J.M. The frequency of undiagnosed diabetes and impaired glucose tolerance in patients with idiopathic sensory neuropathy. Muscle Nerve. - 2001;24:1229-31. McCrimmon R. The mechanisms that underlie glucose sensing during hypoglycaemia in diabetes. Diabet Med. May 2008;25(5):513-22. Clinical Endocrinology and Diabetes: An Illustrated Color Text by Sheru L. Chew, David Leslie. Churchill Livingstone, 2006. – 120 p. Diabetic Medicine Philip Wright Blackwell Publishing Ltd. Oxford, UK, 2007. А. Veves, J.M. Giurini, F.W. LoGerfo (ebs). The diabetic foot (second edn). Humana Press. Totowa, New Jersey, 2006, 696 p. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 5. DIFFERENTIAL DIAGNOSIS OF KETONURIA. IFNMU 2010 Actually Mortality rates for DKA are between 1 and 10%. Shock or coma on admission indicates a worse prognosis. Main causes of death are circulatory collapse, hypokalemia, and infection. Among children with cerebral edema, 57% recover completely, 21% survive with neurologic sequelae, and 21% die. The knowledge of etiological factors that contribute to the development ketoacidosis states pathogenetic mechanisms that cause metabolic disturbances in the patient with diabetes mellitus, diagnostic features and basic elements of immediate treatment of diabetic coma to save the life of the patient and prevent complications. 1. 2. 3. 4. Study aim To know: The causes and mechanisms of decompensation of diabetes mellitus; Early signs ketoatsydotychnyh states; Principles of timely diagnosis and emergency care; Prevention of diabetic coma. To be able: 1. Explain the possible causes of decompensation; 2. To the differential diagnosis of the complications of the disease; 3. Assign adequate medical therapy. Base knowledges, abilities, skills, necessary are studying themes. Discipline To know To be able - The main pathogenetic mechanisms of diabetes mellitus; - The main etiological factors leading to decompensation of the disease; - Biosynthesis, secretion, mechanism of action of insulin. - Detect abnormal levels of ketone bodies; - To correct violations of metabolism. Resuscitation and anesthesiology Urgent measures to prevent diabetic coma. Perform correction of acid-alkaline balance and damaged metabolism. Pharmacology Pharmacodynamic and pharmacokinetic features of drugs that eliminate the state ketoacidosis. Apply the medication to the impact of abnormal levels of disease. Path. Physiology Assessment questions: 1. To define the notion of ketosis, ketoacidosis and ketoacidic coma. 2. Visit the cause of decompensation of diabetes mellitus. 3. An algorithm to compute intermediate care at ketoacidosis condition. 4. Tell about the possible complications damaged metabolism and list the measures to prevent them. 5. Perform differential diagnosis hyperglycemic state with ketonuria. 6. Explain the mechanism of these symptoms ketoacidosis as: Kussmaul's breathing, "acute abdomen", etc. 7. List the early signs of diabetic ketoacidosis. 8. Describe the main laboratory parameters, confirming ketoacidosis. 9. Terming the basic principles of management of patients with decompensated diabetes mellitus and concomitant surgical pathology. 10. Tell about the tactics of elderly patients with ketosis and pathology of the cardiovascular system. Self-assessment examination: # 1. When suspected diabetic psevdoperytonit with which these surveys will you do first? A. determining glycemia; B. determine glycosuria; C. determination of ketonuria; D. determine the activity of alpha-amylase; E. determine the presence of leukocytosis # 2. The manifestations of hypoglycemia associated with the level of glycemia: A. if glycemicemia is 4 mmol / L; B. if glycemicemia - 3 mmol / L; C. not related; D. yes, but with a period of days; E. yes, but the nature of the physical work # 3. Which of these measures is necessary to hold in the case of hypoglycemia? A. insulin therapy; B. 40% glucose solution; C. 10% glucose solution; D. 5% fructose solution # 4. Healing diabetic ketoacidosis applying: A. insulin short action; B. introduction solution with kalii from the very beginning of treatment; C. input soalt solutions; D. the introduction of 40% glucose solution; E. introduction of 10% glucose solution # 5. Episodic hypoglycemia characteristic of these diseases: A. insulinoma; B. pheohromotsytoma; C. Itsenko-Cushing's syndrome; D. diffuse toxic goiter; E. diabetes insipitus # 6. Development ketoacidic coma and promote these factors: A. reducing unnecessary dose of insulin; B. physical and mental injury; C. short-term reduction of caloric food; D. alcohol; E. abuse of simple carbohydrates # 7. In decompensated diabetes mellitus, high lever blood sugar characteristic symptoms: A. no drought; B. a great thirst; C. severe famine; D. dry skin; E. wet skin # 8. Which of the listed measures to bring to ketoacidic coma should be started at the prehospital stage: A. rehydration; B. insulin therapy; C. prevention of iatrogenic hypoglycemia; D. restoration of acid-base status; E. prevention of infectious complications # 9. "Ketone bodies" defined in reaction to: A. ortotoluyidyn; B. glucose oxidase C. nitrosynim tetrazolin D. nitroprusyd sodium E. acetic acid # 10. Pain in the abdomen due to ketoacidosis: A. increased peristalsis of the large intestine; B. violation of excretory function of the pancreas; C. expansion of the stomach; D. fever intestine CASE 1. The patient U., 28 years old, during 5 years treated diabetes mellitus, takes insulin in daily dose 38 IU. He was hospitalized with signs of ketoacidosis. What the scheme of insulin therapy is indicated for patient with ketoacidotic state? CASE 2. The patient E., 24 years, is suffering from diabetes mellitus type 1 during 3 years. Several days ago she canceled the insulin. Patient lost consciousness in the evening. She is hospitalized. Objectevly: the skin is dry. Kussmaul's respiration, the odor of acetone from the mouth, tongue is dry, with fur of brown colour. Pulse 120 /minutes, the arterial pressure 80/45 mmHg. The abdomen does not react to the palpation. The liver is + 3 cm. The reaction of urine to acetone is positive, the glucose of blood - 28 mmol/L. What is the preliminary diagnosis? CASE 3. A girl 9 years old has been suffering from diabetes mellitus for 3 years. The patient has fallen ill with acute respiratory infection. Her state became worse during the last two days, the temperature reached 38 0 C, the thirst and the frequency of urination increased. General weakness enlarged. Nausea and vomiting appeared. General condition is grave. Consciousness is dizzy. Rubeosis. The tungue is dry. Heart tones are rythmic, accelerated. What is your diagnosis? Standards of answers to the self- assessment examination. Theme # 5. Differential diagnosis of ketonuria. Answers of the tests: 1. 2. 3. 4. 5. C. B. B. C. A. 6. A. 7. B. 8. B. 9. E. 10. D. Answers of the cases: CASE 1. The scheme of insulin therapy is short or ultrashort action insulin (intensifyed). CASE 2. The preliminary diagnosis is diabetic ketoacidotic coma. CASE 3. Type 1 Diabetes mellitus, stage of decompensation. Diabetic ketoacidosis. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 7. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. SUPPLIMENTARY REFERENCES 1. Gunnerson K.J., Saul M., He S., Kellum J.A. Lactate versus non-lactate metabolic acidosis: a retrospective outcome evaluation of critically ill patients // Crit. Care. – 2006. -10(1). – P.R22. 2. Manual of Endocrinology and Metabolism edited by Norman Lavin. Lippincott Williams & Wilkins. 2009. – 837 p. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 6. INSULINOMA. EARLY DIAGNOSIS, CLINICAL PRESENTATION, TREATMENT. IFNMU 2010 Actually Insulinomas are rare neuroendocrine tumours with an incidence estimated at 1 to 4 new cases per million persons per year. Insulinoma is one of the most common types of tumour arising from the islets of Langerhans cells (pancreatic endocrine tumours). Estimates of malignancy (metastases) range from 5% to 30%. Over 99% of insulinomas originate in the pancreas, with rare cases from ectopic pancreatic tissue. About 5% of cases are associated with tumours of the parathyroid glands and the pituitary (Multiple endocrine neoplasia type 1) and are more likely to be multiple and malignant. Study aim To know: 1. Causes of hypoglycemia; 2. Sings and symptoms of hypoglycemic states; 3. Principles of diagnosis hypoglycemic states; 4. Principles of treatment of patients with hypoglycemia. To be able: 1. To identify of causes in anamnesis of hypoglycemic states; 2. To identify pathology of pancreas and other organs, which led to a hypoglycemic state; 3. Provide differentiated treatment to such patients. Base knowledges, abilities, skills, necessary are studying themes. Discipline Oncology Histology Anatomical Pathology To know - Key performance indicators of oncological employment; - Principles of cancer care. -Histological variants of insulinomas and other pancreatic endocrine tumors. - Histological forms of insulinomas; - Histological variants of pancreatic cells. To be able - Conduct early diagnostic of insulinoma; - Choose the right of treatment tactics. - Microscopy of preparations. - Macroexamination of endocrine pancreatic tumors; - Microscopic study of pancreatic tumors. Assessment questions: 1. Definition of terms “hyperinsulinemia” and “insulinoma”. 2. Etiology and pathogenesis of pancreatic hypoglycemia. 3. Stages of hypoglycaemia development. 4. Pathological anatomy of insulinomas. 5. Classification of endocrine pancreatic tumors. 6. Classification of hypoglycemic states. 7. Classification of primary hyperinsulinemia (hypoglycemic diseases). 8. Diagnosis of hypoglycemic states. 9. The main signs and symptoms of hypoglycemia and pathogenesis of them. 10. Clinical characteristics of the hyperinsulinemia. 11. Differential diagnosis of endocrine hypoglicemia. 12. Principle of treatment of hypoglycemic states. Self-assessment examination: Case 1. A 32 year old male had episodic confusion and blackouts progressing over 2 years. Lab tests demonstrated true hypoglycemia at time of episodes. Two admissions at a local hospital for 72 hour fast showed hypoglycemia without definite hyperinsulinemia. CT scan of the pancreas was normal. Arterial calcium stimulation did not localize an insulin secreting mass. A trial of diazoxide did not improve his symptoms. On a repeat 72 hour fast, admission blood glucose was 3,2 mmol/L, insulin - 4.6 uU/mL (normal 5-25 uU/mL), C-peptide - 1.4 ng/mL (normal 1,6-3,6 ng/mL), proinsulin - 86.0 pmol/L (normal 0,35-4,50 pmol/L), negative sulfonylurea screen, with mild confusion present. After 1 hour, glucose was 4,1 mmol/L, insulin - 5.9 uU/mL, C-peptide - 1.5 ng/mL, proinsulin - 103.7 pmol/L, with severe neuroglycopenic symptoms. What is your diagnosis? Case 2. The patient 27 years old, complains on regular morning headache, which is present when he awakes. Patient has type 1 Diabetes Mellitus and takes 82 units of insulin/day. What is your previous diagnosis? Case 3. The patient, 42 years old, has Diabetes Mellitus for 12 years, takes 62 unites of insulin daily, complains on early-morning headache. Fast serum glucose level is 13,2 mmol/l. What is your diagnosis and treatment? Case 4. A 59 years old woman had experienced intermittent fatigue, diaphoresis, and tremors for 6 weeks. The signs and symptoms characteristically occurred several hours after a meal and would abate as soon as the patient ate. Two episodes of syncope prompted her to seek medical attention. Because of her medical history, insulinoma was suspected. Blood analysis revealed a serum glucose level of 1,7 mmol/L (normal, 3.3-6.6 mmol/L) and corresponding serum insulin level of 62 pmol/L (normal 5-25 pmol/L). Proinsulin level at that time was 0.78 ng/mL (normal <0.2 ng/mL). What is your previous diagnosis? Case 5. A 62 years old female patient defines hypoglycemic attacks for 1.5 years. In physical examination the body mass index (BMI) was 24 kg/m2, initial glucose level was 2,72 mmol/L, plasma insulin level was 17 μIU/ml (5–25 μIU/ml), C-peptide level was 12.9 ng/ml (1.6–3.6 ng/ml). Prolonged supervised fast test was applied and at the sixth hour of the test hypoglycemic symptoms were occurred. The CT scan showed no pathology. In the EUS scanning at the pancreas uncinate process, there was a hypoechoic 11 mm nodular lesion. It was in homogenous echo and well shaped. It was toughed as neuroendocrine tumor. She was examined for multiple endocrine neoplasia. Magnetic resonance imaging (MRI) of hypophysis, hypophysial hormonal analysis and intact parathormone levels were normal. What is the best principle of treatment? Case 6. A 43 years old female patient defines hypoglycemic attacks for two years. In physical examination the body mass index (BMI) was 27 kg/m2, initial glucose level was 3,0 mmol/L, plasma insulin level was 16 μIU/ml (5–25 μIU/ml), C-peptide level was 2.7 ng/ml (1.6–3.6 ng/ml). Prolonged supervised fast test was applied and at the sixteenth hour of the test hypoglycemic symptoms were occurred. Simultaneously taken blood samples showed the glucose 2,3 mmol/L, plasma insulin 12.7 μIU/ml, insulin/glucose ratio was 0,52. What should be your next diagnostic step? Standards of answers to the self- assessment examination. Theme # 6. Insulinoma. Early diagnosis, clinical presentation, treatment. Case 1. In this case, a proinsulinoma resulted in severe hypoglycemia in an otherwise healthy, young patient. Case 2. Hypoglycemic status. (You have to investigate blood glucose level at 3 o’clock in the morning and if the level is low decrease the dose of insulin.) Case 3. Somogyi phenomenon. Treatment: gradual reduction of insulin dose. Case 4. This led to a diagnosis of insulinoma. Case 5. The best principle of treatment is the surgical operation. Case 6. The next diagnostic tests are CT scan and magnetic resonance imaging (MRI) of hypophysis, hypophysial hormonal analysis and intact parathormone levels. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 7. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. 1. 2. 3. 4. 5. SUPPLIMENTARY REFERENCES: Cryer P.E. Glucose homeostasis and hypoglycemia. In: Kronenberg H.M., Shlomo M., Polonsky K.S., Larsen P.R., eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia, Pa: Saunders Elsevier; 2008:chap 33. Dhumbe V.M., Amarapurkar A.D., Rege J.D. et al. Insulinoma- a case report. Indian Journal Pathology Microbiology 2004; 47: 540-1. Fajans S.S., Vinik A.I.: Diagnosis and treatment of insulinoma. In Diagnosis and Management of Endocrine Related Tumors. Fanten R.J., Manni A., Eds. Boston, Martinus Nijhoff, 1984, p. 235. Starke A., Saddig C., Kirch B., Tschahargane C., Goretzki P.: Islet hyperplasia in adults: challenge to preoperatively diagnose non-insulinoma pancreatogenic hypoglycemia syndrome. World J. Surg. 30:670-679, 2006. Yao M.M., Reynertson R.H. Insulinoma: a case report and review of the clinical features and diagnosis. Gundersen Lutheran Medical Journal 2005; 3: 73-6. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 7. ATYPICAL FORMS OF HYPOTHYROIDISM. DIFFERENTIAL DIAGNOSIS, CLINICAL PRESENTATION. IFNMU 2010 Actually Hypothyroidism is defined as the insufficient production of thyroid hormone. Secondary hypothyroidism as a result of dysfunction of hypothalamic and pituitary hormone secretion are much less common but should be suspected in a patient with a history suggestive of Sheehan syndrome or with symptoms or signs of a tumor in the region of the sella. Ninety-five percent of cases of hypothyroidism are caused by primary thyroid gland failure, resulting in insufficient thyroid hormone production. The most common cause of hypothyroidism is lymphocytic (Hashimoto) thyroiditis, in which cytotoxic antibodies are produced, which leads to thyroid atrophy and fibrosis. The next most common cause is surgical or radioactive iodine treatment for hyperthyroidism, or Graves disease. Worldwide, iodine deficiency is the most common cause of goiter (enlarged thyroid) hypothyroidism. Most hypothyroid patients present with vague and nonspecific symptoms. 1. 2. 3. 4. Study aim To know: The place of hypothyroidism in the structure of endocrinology diseases; To the differential diagnosis of hypothyroidism with other diseases; The etiology, pathogenesis of hypothyroidism; The modern methods of treatment of hypothyroidism. To be able: Clinical and pathogeneses substantiation of hypothyroidism, laboratory and instrumental methods; Principle of palpation of thyroid gland; Timely to diagnostic atypical forms of hypothyroidism. Base knowledges, abilities, skills, necessary are studying themes. Discipline Physiology Pathology Physiology Functional Diagnostics To know Physiological role of thyroid hormones Changes in the amount of thyroid hormones, their causes Diagnostic methods of patients with hypothyroidism To be able Determination (laboratory diagnostic) of thyroid hormones Definition of metabolism in humans with hypothyroidism Dates interpretation of thyroid ultrasound, determine the concentration of thyroid hormones in the blood Assessment questions: 1. 2. 3. 4. 5. 6. Definition of atypical forms of hypothyroidism. Classification of hypothyroidism. Causes of atypical forms of hypothyroidism. Primary, secondary hypothyroidism: etiology and pathogenesis. Changes of the skin and subcutaneous adipose tissue in patients with hypothyroidism. Changes of cardiovascular system, nervous system and gastrointestinal tract in patients with hypothyroidism. 7. Clinical peculiarities of congenital hypothyroidism. 8. Syndrome of galactorhea - amenorhea. 9. Laboratory and instrumental signs of atypical forms of hypothyroidism. 10. Differential diagnosis of atypical forms of hypothyroidism. 11. Principle of treatment of atypical forms of hypothyroidism. Self-assessment examination: # 1. An individual with cirrhosis who has decreased production of thyroid-binding globulin (TBG) yet clinically is euthyroid would most likely have which one of the listed sets of laboratory values? A. B. C. D. E. Serum T4 Normal Decreased Normal Decreased Decreased Serum T3 Normal Normal Decreased Normal Decreased Serum TSH Normal Normal Normal Decreased Normal # 2. An 8-month-old infant is being evaluated for growth and mental retardation. Physical examination reveals a small infant with dry, rough skin; a protuberant abdomen; periorbital edema; a flattened, broad nose; and a large, protuberant tongue. Which one of the listed disorders is the most likely cause of this infant’s signs and symptoms? A. Graves’ disease B. Cretinism C. Toxic multinodular goiter D. Toxic adenoma E. Struma ovarii # 3. A perimenopausal woman presents with increasing swallowing difficulty and fatigue. Physical examination reveals that her thyroid is enlarged (palpable goiter). Laboratory examination of her serum reveals T4 of 4.9 mg/dL, free T4 of 2.5 ng/dL, and TSH of 5.5 mIU/mL. No thyroidstimulating immunoglobulins are identified in the serum, but antimicrosomal antibodies are present. Which one of the listed histologic findings, if present in a thyroid biopsy from this individual, would be most consistent with a diagnosis of Hashimoto’s thyroiditis? A. Lymphocytic infiltrate without follicle formation B. Intense lymphoplasmacytic infiltrate with lymphoid follicles and scattered oxyphilic cells C. Hyperplasia of follicular cells with scalloping of colloid at the margin of follicles D. Granulomatous inflammation with multinucleated giant cells surrounding fragments of colloid E. Dense fibrosis within the thyroid gland extending into adjacent soft tissue # 4. Histologic sections of a follicular carcinoma of the thyroid would characteristically reveal: A. An amyloid stroma intermixed with neoplastic C cells B. Blood vessel and capsular invasion by malignant thyroid follicles C. Diagnostic nuclear changes including “Orphan Annie eyes,” nuclear grooves, and intranuclear inclusions D. Papillary fronds with fibrovascular cores and psammoma bodies E. Undifferentiated anaplastic cells with occasional giant cells # 5. A 37 years old man presents with a single, firm mass within the thyroid gland. This patient’s father developed a tumor of the thyroid gland when he was 32 years of age. Histologic examination of the mass in this 37 years old male reveals organoid nests of tumor cells separated by broad bands of stroma, as seen in the photomicrograph below. The stroma stains positively with Congo red stain and demonstrates yellowgreen birefringence.The most likely diagnosis of this lesion is: A. Follicular carcinoma B. Papillary carcinoma C. Squamous cell carcinoma D. Medullary carcinoma E. Anaplastic carcinoma # 6. A 42 years old woman presents to your office for her annual physical. On examination, you note neck fullness. When you palpate her thyroid, it is enlarged, smooth, rubbery, and nontender. The patient is asymptomatic. You send her for thyroid function testing: her T4, free T4, and T3 are normal, but her TSH is slightly elevated. Which of the following is the most likely diagnosis? A. Iodine deficiency B. Thyroid cancer C. Hashimoto thyroiditis D. Graves disease E. Multinodular goiter # 7. Which of the following laboratory tests could be performed to confirm your diagnosis of the patient in Question 6? A. Repeat thyroid function tests B. Thyroid ultrasound C. Nuclear thyroid scan D. Antithyroid antibody tests E. Complete blood count with differential # 8. A 19 years old gymnast active in national competition is brought to your office by her mother because the daughter’s menses have ceased for the last 3 months. Prior to this, she was always regular. She denies excess dieting, although she does work out with her team 3 hours daily. Her physical examination is normal except for her body mass index (BMI) of 20 kg/m2. Which of the following laboratory tests should be ordered first? A. Thyroid function tests B. Complete blood count C. Luteinizing hormone (LH)/follicle-stimulating hormone (FSH) D. Prolactin E. Beta-hCG # 9. A 35 years old woman who was diagnosed with hypothyroidism 4 weeks ago presents to your office complaining of persistent feelings of fatigue and sluggishness. After confirming your diagnosis with a measurement of the TSH, you started her on levothyroxine 50 μg daily. She has been reading about her diagnosis on the Internet and wants to try desiccated thyroid extract instead of the medicine you gave her. On examination, she weighs 95 kg, her heart rate is 64 bpm at rest, and her blood pressure is normal. Which of the following is the best next step? A. Tell her that this delay in resolution of symptoms is normal and schedule a follow-up visit with her in 2 months B. Change her medication, as requested, to thyroid extract and titrate C. Increase her dose of levothyroxine and have her come back in 4 weeks D. Tell her to start a multivitamin with iron to take with her levothyroxine Case 1. A 38 years old woman presents to your office for evaluation of menstrual irregularity. She states that her periods started when she was 12 years old, and they have been fairly regular ever since, coming once every 28 to 30 days. She has had three previous uncomplicated pregnancies and deliveries. However, approximately 9 months ago, her cycles seemed to lengthen, and for the last 3 months she has not had a period at all. She stopped breast-feeding 3 years ago, but over the last 3 months she noticed that she could express a small amount of milky fluid from her breasts. She had a bilateral tubal ligation after her last pregnancy, and she has no other medical or surgical history. She takes no medications except multivitamins. Over the last year or so, she thinks she has gained about 10 kg, and she feels as if she has no energy despite adequate sleep. She has noticed some mild thinning of her hair and slightly more coarse skin texture. She denies headaches or visual changes. Her physical examination, including pelvic and breast examinations, are normal. She is not obese or hirsute. You elicit slight whitish nipple discharge. Her pregnancy test is negative. What is the most likely diagnosis? What is the most likely etiology for the condition? Case 2. The patient, 35 years old, 3 month ago has subtotal thyroidectomy. She complaints on fatigue, somnolence, constipation, edema on the face, changing of the voice. During examination was found: skin pale, thick and cold, face enlarged, pulse – 58/minute, blood pressure is decreased. What is the most likely diagnosis? What is the most likely the plan of examination? Standards of answers to the self- assessment examination. Theme # 7. Atypical forms of hypothyroidism. Differential diagnosis, clinical presentation. 1. 2. 3. 4. B. B. B. B. 5. 6. 7. 8. 9. D. C. D. E. C. Case 1. Most likely diagnosis: Oligomenorrhea and galactorrhea due to hypothyroidism. Most likely etiology: In this patient with symptoms of weight gain, fatigue, thinning hair, and galactorrhea in the setting of previously normal menses, hypothyroidism is the most likely diagnosis. Case 2. Most likely diagnosis: Primary, postoperative hypothyroidism. Most likely of plan of examination: Level of thyroid hormones T4, T3, TSH and fat metabolism cholesterol. REFERENCES PRINCIPAL REFERENCES Lectures. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. 1. 2. 3. 4. SUPPLIMENTARY REFERENCES: Cooper D.S.: Clinical practice. Subclinical hypothyroidism. N. Engl. J. Med. 2001; 345:260–265. Dillman W.H.: The thyroid. In Goldman L., Bennett J.C. (eds): Cecil Textbook of Medicine, 21st ed. Philadelphia, WB Saunders, 2000, p.p. 1231–1250. Santiago-Fernandez P., Torres-Barahona R., Muela-Martinez J.A., et al. Intelligence quotient and iodine intake: a cross-sectional study in children. J. Clin. Endocrinol. Metab. Aug 2004; 89(8): 3851-7. Romanchishen A.F., Lakovlev P.N. Special surgical treatment of patients with nodular tumors of the thyroid gland against the background of diffuse toxic goiter. Vestn. Khir. Im. I. I. Grek. 2005; 164(1): 21-4. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 8. TOXIC ADENOMA. EARLY DIAGNOSIS, CLINICAL PRESENTATION, TREATMENT. IFNMU 2010 Actually Hyperthyroidism has no uniform etiology. Of three patients, only two fit the picture of the syndrome described first by Graves and later, in more detail, by Basedow. The third patient's hyperthyroidism is caused by a toxic thyroid adenoma. Toxic adenoma accounted for 9.5 % of a series of 680 thyrotoxic patients. Comparison of the 65 cases of toxic adenoma with the 615 cases of Graves disease revealed that the former group presented a milder clinical picture, without overt toxicity in about 40 % of the cases. Approximately 1 in 10, to 1 in 20 solitary nodules present with hyperthyroidism. This varies from country to country, being more common in Europe than in the USA. The problem is 5 times more common in women than men. The proportion of cases of thyroid toxic adenoma with hyperthyroidism was 33% in males, but only 17% in females. 1. 2. 3. 4. 5. 6. Study aim To know: Risk factors for thyroid adenoma; Early detection of disease; Learn the complications of thyrotoxicosis, including thyroid storm; Understand the evaluation of a patient with a thyroid nodule; Histological of thyroid adenoma; Principle of treatment of toxic thyroid adenoma. 1. 2. 3. 4. To be able: Show a history of risk factors of thyroid adenoma; Be able to discuss the causes of hyperthyroidism, including Graves disease and toxic nodule; To identification of thyroid pathology; Differentiated to provide to treatment the patients with thyroid adenoma. Base knowledges, abilities, skills, necessary are studying themes. Discipline Oncology Histology Human pathology To know To be able Key indicators of service of patients with To conduct early diagnosis of toxic thyroid adenoma; thyroid adenoma; Principles of cancer care. Right-to guide patient treatment. Histological variants of toxic thyroid To study preparation (puncture, adenoma. biopsy), microscopy. Groups of thyroid neoplasms; Macroexamination of thyroid Histological forms of toxic tumors; thyroid adenoma. Microscopic study of thyroid tumors. Assessment questions: 1. To define a toxic thyroid adenoma. 2. Etiology and pathogenesis of toxic thyroid adenoma. 3. Histological picture of toxic thyroid adenoma. 4. The clinical presentation of toxic thyroid adenoma. 5. Laboratory diagnostic of toxic thyroid adenoma. 6. Instrumental diagnostic of toxic thyroid adenoma. 7. Diagnosis and differential diagnosis of toxic thyroid adenoma. 8. Prediction of this disease. 9. Principle of treatment of toxic thyroid adenoma. Self-assessment examination: # 1. A 58 years old woman is noted to have Graves disease, and has a nodule toxic goiter. Which of the following is the best therapy? A. Long-term propranolol B. Lifelong oral propylthiouracil (PTU) C. Radioactive iodine ablation D. Surgical thyroidectomy # 2. Which of the following distinguishes hyperthyroidism from thyroid storm? A. Tachycardia to heart rate 120 bpm B. Weight loss C. Fever and delirium D. Large goiter # 3. A 44 years old woman is noted to be nervous and has heat intolerance. Her thyroid gland is diffusely enlarged, nontender, with an audible bruit. Her TSH level is very low. Which of the following is the most likely etiology? A. Lymphocytic thyroiditis B. Hashimoto thyroiditis C. Graves disease D. Multinodular toxic goiter # 4. Graves’ disease is characterized clinically by finding: A. Central obesity, “moon” face, and abdominal striae B. Hyperthyroidism, exophthalmus, and pretibial myxedema C. Polyuria, polydipsia, and hyponatremia D. Polyuria, polydipsia, and polyphagia E. Progressive lethargy, cold intolerance, and myxedema # 5. The term goiter refers to Any enlargement of the thyroid regardless of the etiology Any involution of the thyroid regardless of the etiology Enlargement of the thyroid secondary to Graves’ disease Enlargement of the thyroid secondary to the ingestion of goitrogens Involution of the thyroid secondary to Hashimoto’s thyroiditis Case 1. A 37 years old previously healthy woman presents to your clinic for unintentional weight loss. Over the past 3 months, she has lost approximately 8 kg without changing her diet or activity level. Otherwise, she feels great. She has an excellent appetite, no gastrointestinal complaints except for occasional loose stools, a good energy level, and no complaints of fatigue. She denies heat or cold intolerance. On examination, her heart rate is 108 bpm, blood pressure 142/82 mm Hg, and she is afebrile. When she looks at you, she seems to stare, and her eyes are somewhat protuberant. You note a large, smooth, nontender thyroid gland, a 2/6 systolic ejection murmur on cardiac examination, and her skin is warm and dry. There is a fine resting tremor. What is the most likely diagnosis? How could you confirm the diagnosis? What are the options for treatment? Standards of answers to the self- assessment examination. Theme # 8. 1. 2. 3. 4. 5. D. C. C. B. A. Case 1. Most likely diagnosis: Thyrotoxicosis/Graves disease. Confirming the diagnosis: A low serum thyroid-stimulating hormone (TSH) level and an increased free thyroxine (T4) level with this clinical presentation would be confirmatory of hyperthyroidism. However, other tests that would define the etiology would be thyroid-stimulating immunoglobulins or diffusely elevated uptake of radioactive iodine on thyroid scan. Treatment options: Antithyroid drugs, radioactive iodine ablation, or less commonly, surgical ablation of the thyroid. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Singer P.A. Thyroiditis. In: Lavin N., ed. Manual of Endocrinology and Metabolism. Boston, M.A: Little Brown; 2002:386-395. 5. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 6. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. SUPPLIMENTARY REFERENCES 1. American Association of Clinical Endocrinologists. Medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocrine Pract. 2002;8:457-469. 2. Belfiore A., Sava L., Runello F., Tomaselli L., Vigneri R. 1983 Solitary autonomously functioning thyroid nodules and iodine deficiency. J Clin Endocrinol Metab. 56:283–287. 3. Davies D.F., Larsen T.F. Thyrotoxicosis. In: Wilson J.D., Foster D.W., Kronenberg H.M., et al., eds. Williams Textbook of Endocrinology. 9th ed. Philadelphia, PA: WB Saunders; 2003: 372-421. 4. Hay I.D., Morris J.C. 1996 Toxic adenoma and toxic multinodular goiter. In: Braverman L.E., Utiger R.D., eds. Werner and Ingbar’s the thyroid. Philadelphia: Lippincott-Raven; 566–572. 5. McDermott M.T. Thyroid emergencies. In: Endocrine Secrets. Philadelphia, P.A: Hanley and Belfus; 2002: 302-305. 6. MacFarlane I. 2000 Thyroid disease. Pharm. J. 265; 240-244. 7. Wiener J.D. 1987 Plummer’s disease: localized thyroid autonomy. J. Endocrinol. Invest. 10:207–224. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 9. ADRENO-GENITAL SYNDROME. EARLY DIAGNOSIS, CLINICAL PRESENTATION, TREATMENT. IFNMU 2010 Actually Adreno - genital syndrome is a group of disorders caused by adrenocortical hyperplasia or malignant tumors, resulting in abnormal secretion of adrenocortical hormones and characterized by masculinization of women, feminization of men, or precocious sexual development in children. About 1 in 10,000 to 18,000 children are born with congenital adrenal hyperplasia. A newborn screening test is available for the most common form of congenital adrenal hyperplasia and can be done on heelstick blood (as part of the routine screenings done on newborns). Study aim To know: 1. Control mechanism at the level of sex hormones hypothalamus-pituitary-adrenal-ovarian; 2. Menstrual regulation; 3. The differential diagnosis with other pathological conditions - clinical, laboratory and instrumental research. To be able: 1. Collect gynecological anamnesis; 2. Diagnostic of organ damage. Base knowledges, abilities, skills, necessary are studying themes. To know Mechanism of regulation of sex hormones. Mechanism of regulation of hormone Path. Physiology disorders. Synthesis of sex hormones. Biochemistry Gynecological and endocrinology aspects Obstetric and Gynaecology of pathology. Neiroendocrinology syndromes. Endocrinology To be able Discipline Physiology Diagnostic tests set. Diagnostic tests set. Assessment questions: 1. Anatomical and physiological features of the reproductive system. 2. Hormones of the reproductive system. 3. Premature male sexual development. 4. Hormone producing tumors of testis. 5. Main principles of hormone regulation with regard to the reproductive system. 6. Assess methods of reproductive status. Diagnostic methods. 7. Classification of adreno - genital syndrome. 8. Laboratory diagnostic of all forms adreno - genital syndrome. 9. Principle of treatment of other forms of adreno-genital syndrome. 10. Classification of hermaphroditism. 11. Stein-Leventhal syndrome. 12. Virilization. 13. Hormone producing tumors of ovaries. 14. Clinical signs of delayed puberty. 15. Signs of hypogonadism depends on age. 16. Clinical features of hy pergonadotropic hypogonadism in girls. 17. Clinical features of secondary hypogonadism in girls: clinical signs, diagnosis. Self-assessment examination: # 1. Which of the following results would be diagnostic of this patient's condition? A. Decreased serum ACTH B. Decreased serum aldosterone C. Increased serum DHEA D. Increased serum 17-OH-progesterone E. Increased urinary 17-ketosteroids # 2. If a young woman had 11-hydroxylase deficiency, which of the following presentations would be most likely? A. Adrenal insufficiency B. Elevated 11-deoxycortisol C. Hyperkalemia and hypotension D. Increased aldosterone E. Normal menses and hair growth # 3. Overproduction of androgens is evidenced by: A. Low level of 17-KS in urine B. Hirsutism C. Gigantism D. Cretinism E. Mental retardation # 4. Temporary lack of pubertal development due to the following conditions, except: A. Isolated gonadotropin deficiency B. Malnutrition C. Emotional stress D. Excessive physical stress E. Untreated endocrinopathies # 5. What statement is not correct relatively to the polycystic ovary syndrome? A. Alopecia is common B. Polycystic ovary syndrome presents with elevated androgen levels C. Patients with polycystic ovary syndrome have amenorrhea D. Hirsutism is common E. Obesity is often found # 6. Choose the drug, which will not cause gynecomastia A. Isoniazid B. Cimetidine C. Hexestrolum D. Metformin E. Digitoxin # 7. Differential diagnosis of ambiguous genitalia includes the following measures, except: A. Bone age x ray B. Physical examination C. Contrast urography D. Chromosomal evaluation E. Stimulation or suppression tests Case 1. An 8 year old male child presented with fever. On routine examination it was observed that there was bilateral cryptorchidism and presence of pubic hair corresponding to SMR stage 3. The scrotum was well developed and the penis was small (with no prepuce) with an urethral opening at its tip. There was generalized hyper-pigmentation and presence of acne. These findings prompted investigation for ambiguous genitalia. Abdominal CT scan revealed presence of uterus and its adenexa and bilateral adrenal enlargement. Karotyping revealed 46-XX genotype. The serum 17-hydroxyprogesterone (17-OHP) level was 2.8 ng/mL (normal: 0.2-0.5 ng/mL) and urinary 17-ketosteroids was 18 mg/d (normal: 1-4 mg/d). The clinical findings and investigations suggested the diagnosis of a female pseudohermaphrodite. What is the preliminary diagnosis? Case 2. A mother brings her 2-week-old daughter to the emergency department because of protracted vomiting. She states her baby has been vomiting for the last few days and was not tolerating any milk, or water. The baby had been "very fussy" but had not been feverish. The course of her pregnancy was uneventful and she was vaginally delivered without any complications. On examination, the baby appears ilI, but well developed. Her blood pressure is 50/30 mm Hg, pulse is 176/min, and respiratory rate is 35/min. Her oral mucosa look dry and she is not tearing much. Her anterior fontanelle appears sunken, and mild tenting can be elicited in her skin. An enlarged clitoris and partial fusion of the labial folds is noted. Serum electrolytes are significant for sodium of 123 mEq/L, chloride of 92 mEq/L, and bicarbonate of 27 mEq/L. Which of the following is most likely diagnosis? Case 3. An 11 days old infant with abnormal genitalia and failure to thrive since birth was referred to hospital. On the 3rd day the infant had blood-stained purulent discharge from the abnormal genital opening. She was vomiting 2-3 time a day and having 4-5 loose stools/ day containing no blood or mucus. On examination she weighed 2,5 kg was ashen grey in color, marasmic and degydrated. The pulse was of feeble volume, the rate – 144/min. Abdomen, heart, chest, nervous system were normal. Local examination showed increased pigmentation around the genitalic. The clitoris was enlarged to 2,5 cm. The labila majora had horizontal folds. What is the preliminary diagnosis? Case 4. A 22 years old male presented with palpable painless hardness mass lesions over bilateral testes for two weeks. He had no history of trauma or other systemic disease. General physical examination was normal. Laboratory studies, including complete blood count, routine urinalysis, blood coagulation studies, blood biochemistry tests, carcinoembryonic antigen (CEA), and α-fetoprotein (AFP) tests were normal. Endocrine evaluation revealed normal thyroid function tests and values of testosterone, estradiol, folliclestimulating hormone, luteinizing hormone, cortisol, and prolactin were normal in limits. The ACTH level – 61,3 pg/mL (normal range: 9.0~52.0 pg/mL) was found to be elevated. The semen analysis showed azoospermia. Chromosomal analysis was normal as 46,XY. The scrotal ultrasonography (US) revealed normal size of both testes and several round to oval hypoechoic lesions, 8 mm ~ 1.7 cm in diameter, in bilateral mediastinum testes. They were sharply delineated from the normal parenchyma and had no acoustic attenuation or enhancement. On magnetic resonance (MR) imaging, the lesions were isointense or hypointense on T1-weighted and hypointense on T2-weighted MR images as compared with normal testicular parenchyma. Which of the following is most likely diagnosis? Standards of answers to the self- assessment examination. Theme # 9. D. B. B. A. A. D. A. Case 1. Congenital adrenal hyperplasia resulting in adreno-genital syndrome. Case 2. Congenital adrenal hyperplasia. Case 3. Adreno-genital syndrome. Salt-losing form of C21-hydroxylase deficiency. Case 4. Adrenal Nodular Hyperplasia with so Called Testicular Tumor of Adreno-genital syndrome. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. SUPPLIMENTARY REFERENCES 1. Fetal Adrenal Development. In Williams Obstetrics, 20th ed. Stamford, CT: Appleton & Lange, 1997. 2. Fetal Treatment. In Medical Genetics, ed. Lynn B. Jorde, et al. St. Louis: Mosby, 1995. 3. Hay Jr., William W., et al., eds. Current Pediatric Diagnosis and Treatment. Stamford, CT: Appleton & Lange, 1997. 4. Richard A.A., Shawn M.M., Philip A.I., et al. Clinical and pathological features associated with the testicular tumor of the adrenogenital syndrome. J. Urol. 2007; 177: 546-549 Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 10. METABOLIC OSTEOPATHIES ASSOCIATED WITH ENDOCRINOPATHIES. IFNMU 2010 Actually Osteoporosis, a condition characterized by decreased bone strength, is prevalent among postmenopausal women but also occurs in men and women with underlying conditions or major risk factors associated with bone demineralization. Its chief clinical manifestations are vertebral and hip fractures, although fractures can occur at any skeletal site. Osteoporosis affects 10 million individuals in the United States, but only a small proportion are diagnosed and treated. Endocrinous osteoporosis constitutes the largest group among the secondary osteoporosis. This problem has been thoroughly studied in Ukraine at the Gerontology Institute (prof. V. V. Povoroznjuk et al., 2001), under the Academy of Medical Sciences of Ukraine and V. P. Komyssarenko Institute of Endocrinology and Metabolic Processes under the Academy of Medical Sciences of Ukraine (prof. V. А. Oleinyk et al., 2000). Study aim 1. 2. 3. 4. 5. 6. To know: Factors that influence the functional status of bone tissue; The main risk factors for osteoporosis; Classification of osteoporosis; Clinical picture of osteoporosis; Diagnostic criteria of osteoporosis; Principles of prevention and treatment of osteoporosis. To be able: 1. Reveal a history of risk factors of osteoporosis; 2. Diagnostic criteria of osteoporosis using X-ray, morphometric, histochemical, densitometric, biochemical methods; 3. Appoint a permanent and preventive treatment of osteoporosis. Base knowledges, abilities, skills, necessary are studying themes. Discipline Physiology Path. Physiology Radiology Biochemistry Endocrinology To know Calcium homeostasis in the human body Disturbance of calcium homeostasis in the human body X-ray of the bones and densitometry Biochemical markers of bone metabolism Risk factors for osteoporosis To be able Identify of pathological disturbance in the bones. Rate data obtained Identify risk factors of osteoporosis in anamnesis Assessment questions: 1. The most important first messengers for Dental Biochemistry include parathyroid hormone, calcitonin, insulin, and glucagon. 2. Define calcium balance. 3. Anatomy and physiology of a bone tissue. 4. The function of main cells of a bone tissue – osteoclasts, osteoblasts, osteocytes. 5. Hormonal regulation of bone remodeling. 6. Classification of endocrine osteoporosis. 7. Describe the properties and mechanism of action of parathyroid hormone (PTH) including G-protein function. 8. Review the composition of bone, and know what bone mineral is? 9. What are the two main functions of parathyroid hormone in kidney? 10. Describe the metabolic activation of vitamin D. 11. What are the actions of vitamin D? 12. What is osteomalacia? Hyperparathyroidism? Pseudohypoparathyroidism? 13. What is osteoporosis? 14. Describe physiological ways to establish and maintain maximum bone density. 15. What foods are good sources of dietary calcium? 16. Make a scheme of development of osteoporosis in case of the main endocrine diseases. 17. Clinics of osteoporosis. 18. Diagnostics and differential diagnostics of osteoporosis. 19. Prophylaxis and treatment of osteoporosis. Self-assessment examination: # 1. Which of the following patients is most likely to be a candidate for bone mineral density screening? A. A 65-year-old, thin, white woman who smokes and is 15 years postmenopausal B. A 40-year-old white woman who exercises daily and still menstruates C. A healthy 75-year-old white man who is sedentary D. A 60-year-old overweight African American woman E. A 35-year-old asthmatic woman who took prednisone 40 mg/d for a 2-week course 1 week ago #2. During which of the following periods in a woman’s life is the most bone mass accumulated? A. Ages 15 to 25 B. Ages 25 to 35 C. Ages 35 to 45 D. Ages 45 to 55 # 3. A 60 years old woman presents with the results of her DEXA scan. She has a T score of −1.5 SD at the hip and −2.5 at the spine. Which of the following is the most accurate interpretation of these results? A. She has osteoporosis at the spine and osteopenia at the hip B. She has osteoporosis in both areas C. This is a normal examination D. She has osteoporosis of the hip and osteopenia at the spine E. You need to know the Z score # 4. You see a 70-year-old woman in your office for a routine checkup, and you order a DEXA scan for bone mineral density screening. The T score returns as −2.5 standard deviations SD in the spine and −2.6 in the hip. Which of the following statements is most accurate? A. This patient has osteopenia B. Estrogen replacement therapy should be started with an anticipated rebuilding of bone mass to nearnormal within 1 year C. Swimming will help build bone mass D. Bisphosphonates would reduce the risk of hip fracture by 50% # 5. Which one of the listed signs or symptoms is more characteristic of hypocalcemia than of hypercalcemia? A. Calcium stones in the urine B. Metastatic calcification C. Peptic ulcers D. Psychiatric changes E. Tetany # 6. A 62-year-old asymptomatic woman is noted to have multiple myeloma and an elevated calcium level, but no bone lesions or end-organ damage. Which of the following therapies is useful for immediate treatment of the hypercalcemia? A. Bisphosphonates B. Erythropoietin C. Dexamethasone plus thalidomide D. Interferon-a E. Observe without treatment since she is asymptomatic Case 1. A 75 years old white woman presents to the emergency room with right wrist pain after a fall at home. She tripped and fell while preparing dinner, and she says that she tried to stop her fall with her outstretched right hand. She heard a “snap” and felt immediate pain. Her medical history is remarkable only for three normal pregnancies, menopause at age 50 years, and hypertension that is well controlled with diuretics. She has a 50-pack per year history of smoking. Her weight is 85 kg and her height is 174 cm. Her examination is remarkable for normal vital signs; a swollen, deformed right distal forearm and wrist, with limited mobility because of pain; and good radial pulses and capillary refill in the right fingernail beds. An X-ray confirms a fracture of the right radial head, and the radiologist notes osteopenia. 1. What risk factor for fracture is this woman likely to have? 2. What are the causes of this condition? 3. What can her physician offer her to prevent future fractures? Standards of answers to the self- assessment examination. Theme # 10. 1. 2. 3. 4. 5. 6. A. A. A. D. E. A. Case 1. 1. Risk factor for fracture: Osteoporosis. 2. Causes of this condition: Decreased bone strength as a consequence of demineralization and increased bone turnover as a result of decreased levels of sex steroids (estrogen and testosterone), medications, other hormonal conditions, or diseases of decreased calcium absorption. 3. Preventive measures: Several medications are available to increase bone density, which may decrease the risk of future fractures. Also, her physician would want to work with her to prevent future falls by limiting unnecessary medications that may cause instability, making changes in the home environment, and evaluating her gait, visual acuity, and peripheral sensory system. The patient should be advised to quit smoking. REFERENCES PRINCIPAL REFERENCES 1. Lectures. 2. Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. 3. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. 4. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. 5. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. SUPPLIMENTARY REFERENCES 1. Diagnosis and treatment of osteoporosis. Bloomington (MN): Institute for Clinical Systems Improvement (ICSI); 2008 Sep. 67 p. 2. Heaney R.P. Advances in therapy for osteoporosis. Clin. Med. Res. Apr. 2003;1(2):93-99. 3. Wasnich R.D., Bagger Y.Z., Hosking D.J., et al. Changes in bone density and turnover after alendronate or estrogen withdrawal. Menopause. Nov-Dec 2004;11((6 Pt 1)):622-630. Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y. MINISTRY OF HEALTH, UKRAINE IVANO-FRANKIVSK NATIONAL MEDICAL UNIVERSITY CHAIR OF ENDOCRINOLOGY METHODOLOGICAL PROTOCOLS BY POST-AUDITORIUM INDIVIDUAL WORK OF ENDOCRINOLOGY FOR FOURTH - YEAR STUDENTS OF FACULTY OF PREPARATION OF FOREIGN CITIZENS WITH THE SPECIALITY “MEDICINE” Theme # 11. IFNMU 2010 Actually Study aim To know: To be able: Base knowledges, abilities, skills, necessary are studying themes. Discipline To know Path. Physiology Internal medicine Pharmacology Assessment questions: Self-assessment examination: # 1. Standards of answers to the self- assessment examination. Theme # 11. B. C. B. D. A. D. B. D. C. A. D. C. B. A. B. REFERENCES PRINCIPAL REFERENCES Lectures. To be able Endocrinology. Textbook/ Study Guide for the Practical Classes. Ed. by prof. Petro M. Bodnar: Vinnytsya: NOVA KNYHA Publishers, 2008. – 496 pp.: Art. Endocrinology Studie Guide for the Practical Classes Ed. by prof. Petro M. Bodnar, academician APS of Ukraine Sergey D. Maksymenko. Kiev, 2007, 102 p. Basic & Clinical Endocrinology. Seventh edition. Edited by Francis S. Greenspan, David G. Gardner. – Mc Grew – Hill Companies, USA, 2004. – 976 p. Oxford handbook of endocrinology and diabetes. Edited by Helen E. Turner, John A.H. Wass. Oxford, University press. 2006. – 1005 p. Harrison′s Endocrinology.Editor J. Larry Jameson. Mc Grew – Hill, USA, 2006. – 563 p. International Textbook of Diabetes Mellitus Edited by R.A. Defronzo, E. Ferrannini, H. Keen, P. Zimmet. John Wiley & Sons, Ltd. England, 2004. – vol. 1 – 1100 p., vol. 2 – 1913 p. SUPPLIMENTARY REFERENCES: Prepared by MD, PhD, Associate of professor Kostitska I.O. Adopted at the Chair Sitting №…… , …… . … . 2010 y.