* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ANTIMICROBIAL DRUGS
Drug design wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug discovery wikipedia , lookup
Ciprofloxacin wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Levofloxacin wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Antibiotics wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
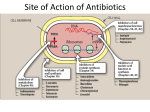
β-Lactam antibiotics Antimicrobial Drugs As a class, they are one of the most frequently used as well as misused drugs. Drugs in this class differ from all others in that they are designed to inhibit/kill the infecting organism and to have no/minimal effect on the recipient. This type of therapy is generally called chemotherapy. Chemotherapy is a treatment of systemic infections with specific drugs that selectively suppress the infecting microorganism without significantly affecting the host. Due to analogy between the malignant cell and the pathogenic microbes, treatment of neoplastic diseases with drugs is also called ‘chemotherapy’. General Considerations Antibiotics These are substances produced by microorganisms, which selectively suppress the growth of or kill other microorganisms at very low concentrations. Chemotherapeutic agent Initially this term was restricted to synthetic compounds, but now since many antibiotics and their analogues have been synthesized, this criterion has become irrelevant; Antimicrobial agent (AMA) includes synthetic as well as naturally obtained drugs that attenuate microorganisms. PROBLEMS THAT ARISE WITH THE USE OF AMAs Toxicity Hypersensitivity reactions Drug resistance (Natural / Acquired resistance ) Superinfection Nutritional deficiencies Masking of an infection Beta-Lactam Antibiotics These are antibiotics having a β-lactam ring. Penicillins Cephalosporins Monobactams Carbapenems PENICILLINS All β-lactam antibiotics inhibit the synthesis of bacterial cell wall→ bacterial lysis occurs → bactericidal action Rapid cell wall synthesis occurs when the organisms are actively multiplying; βlactam antibiotics are more lethal in this phase. High sensitivity to the gram-positive (Gr+) bacteria. Penicillins Natural penicillins Semisynthetic penicillins Natural penicillins Benzylpenicillin (penicillin G, the original penicillin found in 1928), Procaine benzylpenicillin (procaine penicillin) Benzathine benzylpenicillin (benzathine penicillin) Phenoxymethylpenicillin (penicillin V) intravenous use intramuscular use the same antibacterial activity as benzylpenicillin but act for a longer period of time oral use Antibacterial spectrum Narrow spectrum antibiotics; activity is limited primarily to GR+ bacteria, few GR- ones and anaerobes. Cocci: Streptococci, pneumococci, etc. Staph. Aureus - now absolutely resistant Gram negative cocci: Neisseria gonorrhoeae Gram-positive bacilli: Corynebacterium diphtheriae, all Clostridia (tetani and others), Listeria Spirochetes (Treponema pallidum, Leptospira, and others) Bacterial resistance The primary mechanism of acquired resistance is production of penicillinase. Penicillinase -it is a narrow spectrum β-lactamase which opens the β-lactam ring and inactivates penicillin. Some bacteria become penicillin tolerant and not penicillin destroying due to acquired low affinity. The methicillin-resistant Staph. aureus (MRSA) have acquired a PBP which has very low affinity for β-lactam antibiotics. SEMISYNTHETIC PENICILLINS CLASSIFICATION Penicillinase-resistant penicillins (β-lactamase-resistant) Methicillin Nafcillin Oxacillin Cloxacillin Dicloxacillin. Aminopenicillins (broad spectrum penicillins): Ampicillin Amoxicillin Bacampicillin Carboxypenicillins: β-lactamase inhibitors : Carbenicillin Clavulanic acid Ticarcillin Sulbactam Ureidopenicillins: Tazobactam Piperacillin Mezlocillin PENICILLINASE-RESISTANT PENICILLINS Methicillin, Cloxacillin, Dicloxacillin They have side chains that protect the β-lactam ring from attack by penicillinase. However, this also partially protects the bacteria from the β-lactam ring. Their only indication is infections caused by penicillinase producing Staphylococci, for which they are the drugs of choice. MRSA (methicillin resistant Staph. Aureus) have emerged in many areas. These are insensitive to all penicillins and to other βlactams as well as to erythromycin, aminoglycosides, tetracyclines, etc. Broad spectrum penicillins Ampicillin, Amoxicillin None is resistant to penicillinase or to other βlactamases. These semisynthetic penicillins are active against a variety of : Gr- bacilli- H. influenzae, E. coli, Proteus, Salmonella, Shigella and Helicobacter pylori Gr+- as natural penicillins Carboxypenicillins Carbenicillin,Ticarcillin The special feature of this group is its activity against Pseudomonas aeruginosa. P. aeruginosa has association with serious illnesses – especially nosocomial infections such as ventilator-associated pneumonia and various sepsis syndromes. The indications for carbenicillin are—serious infections caused by Pseudomonas, e.g. burns, urinary tract infection, septicaemia. Ureidopenicillins Piperacillin, Mezlocillin This antipseudomonal penicillins is about 8 times more active than carbenicillin. It is frequently employed for treating serious pseudomonal infections in neutropenic/immunocompromised or burn patients. Uses 1. Streptococcal infections like bronchitis, sinusitis, pharyngitis, otitis media, scarlet fever, rheumatic fever, urinary tract infections, 2. Pneumococcal infections for empirical therapy of pneumococcal (lobar) pneumonia and meningitis 3. Meningococcal infections are still mostly responsive; meningitis and other infections may be treated with intravenous injection of high doses. 4. Gonorrhoea 5. Syphilis- T. pallidum has not shown any resistance and penicillin is the drug of choice. 6. Diphtheria (Antitoxin therapy is of prime importance). 7. Tetanus and gas gangrene (Antitoxin and other measures are more important; adjuvant value.) 8. Penicillin is the drug of choice for rare infections like anthrax, actinomycosis, rat bite fever and those caused by Listeria monocytogenes, Pasteurella multocida. Adverse effects Penicillin is one of the most nontoxic antibiotics. Hypersensitivity/ anaphylaxis Allergy Diarrhoea BETA-LACTAMASE INHIBITORS Clavulanic acid, sulbactam,tazobactam β-lactamases are a family of enzymes produced by many gram-positive and gram-negative bacteria that inactivate β-lactam antibiotics by opening the βlactam ring. AUGMENTIN: Amoxicillin + clavulanic acid UNASYN: Ampicillin + sulbactam Piperacillin + tazobactam CEPHALOSPORINS All cephalosporins are bactericidal and have the same mechanism of action as penicillin, i.e. inhibition of bacterial cell wall synthesis. They are divided into 5 generations. This division has a chronological sequence of development, but more importantly, takes into consideration the overall antibacterial spectrum as well as potency. CEPHALOSPORINS 1st Generation Parenteral Cefazolin 2nd Generation Parenteral Cefuroxime Cefoxitin Oral Cephalexin Cefadroxil Oral Cefaclor Cefuroxime axetil Cefprozil 3rd Generation Cefixime, Ceftriaxone, Ceftazidime, Cefoperazone, Cefotaxime 4th Generation (Pseudomonas) Cefepime Cefpirome 5th Generation Ceftaroline Ceftolozane Generations 1st Gen- high activity against Gr+ bacteria. 2nd Gen-These are more active against Gr- organisms,. They are weaker than the 1st generation against Gr+bacteria. Don’t inhibit P. aeruginosa 3rd Gen – high activity against Gr-. Inhibit Pseudomonas. 4th Gen- high activity against Gr-. against Gr+bacteria (weaker than the 1st generation) High activity against Pseudomonas aeruginosa Is indicated for the treatment of serious and resistant hospital-acquired infections including septicaemias, lower respiratory tract infections, etc. 5th Gen- powerful antipseudomonal characteristics and appears to be less susceptible to development of resistance. The first cephalosporin with antimicrobial activity against MRSA. Uses They cover a wide range of Gr+ and Gr- (but not MRSA) → one of the most commonly used antibiotics. 1. As alternatives to penicillins (1st gen ). 2. Respiratory, urinary and soft tissue infections caused by Gr organisms(2nd gen) 3. Penicillinase producing staphylococcal infections (3-5th gen). 4. Septicaemias 5. Surgical prophylaxis 6. Meningitis 7. Gonorrhoea 8. Hospital acquired infections, especially respiratory and other infections in intensive care units, resistant to commonly used antibiotics (3rd or 4th gen) 9. Prophylaxis and treatment of infections in neutropenic patients(3rd gen). Adverse effects Diarrhoea Hypersensitivity reactions Nephrotoxicity Neutropenia and thrombocytopenia Pain after i.m. injection Thrombophlebitis of injected vein MONOBACTAMS Aztreonam Spectrum: Only against aerobic Gr- bacteria (e.g., Neisseria, Pseudomonas ) Reserve drug The main indications of aztreonam are hospital- nosocomial infections originating from urinary, biliary, gastrointestinal and female genital tracts. Adverse effects: skin rash CARBAPENEMS Imipenem, Meropenem Spectrum: Gr+,Gr-, anaerobes Inhibit Pseudomonas Reserve drug for the treatment of serious nosocomial respiratory, urinary, abdominal, pelvic, skin and soft tissue infections ADR: hypersensitivity reactions TETRACYCLINES Tetracyclines inhibite practically all types of pathogenic microorganisms → name ‘broadspectrum antibiotic’. Classification: - natural (tetracycline); - semisynthetic (doxycycline). In world practice for the systemic action is used primarily doxycycline. Mechanism of action: inhibition of bacterial protein synthesis by interfering with ribosomes of bacteria Action: bacteriostatic Activity: as drugs with a broad spectrum of antimicrobial activity, but in the process of their long-term use, many bacteria have acquired resistance to them. Gr+ flora: Streptococcus pneumoniae, but resistant to tetracycline, many strains of S. pyogenes, and nosocomial strains of staphylococci and most enterococci. Gr - flora: the meningococcus and M. catarrhalis; many gonococci are resistant. Tetracyclines are also active against Listeria monocytogenes, H. influenzae, Yersinia (including Yersinia pestis), Campylobacter (including H. pylori), Brucella, bartonellas, vibrios (including cholera), agents of inguinal granuloma, anthrax, tularemia, spirochetes, Leptospira, Borrelia (including the causative agents of Lyme disease), Rickettsia (including pathogens I spotted fever of the Rocky mountains. and of typhus), chlamydia, Mycoplasma (including the causative agents of atypical pneumonia), actinomyces, Clostridium (except C. difficile), fuzobakterii, P. acnes, Entamoeba histolytica. Most strains of E. coli, Salmonella, Shigella, Klebsiella, Enterobacter bacteroids sustainable. Specific adverse reactions: tooth/ bones damage(because of the affinity to Ca2+ and formation of complexes, which leads to demineralization of bone tissue). Adverse effects: Teeth and bones Tetracyclines are deposited in developing teeth and bones → brown discolouration, ill-formed teeth which are more susceptible to caries. Tetracyclines given between 3 months and 6 years of age affect the crown of permanent anterior dentition. Suppression of bone growth + deformities +reduction in height Tetracyclines should not be used during pregnancy, lactation and in children. Irritative effects (epigastric pain, nausea,vomiting and diarrhoea) Hepatotoxicity Phototoxicity Uses Tetracyclines are the first choice drugs: Venereal diseases: Chlamydial nonspecific urethritis/endocervicitis Lymphogranuloma venereum Granuloma inguinale. Atypical pneumonia Cholera Brucellosis Plague: Tetracyclines are highly effective in both bubonic and pneumonic plague. They are preferred for blind/mass treatment of suspected cases during an epidemic. Relapsing fever: due to Borrelia Rickettsial infections: typhus, rocky mountain spotted fever, Q fever, etc. respond dramatically. Anthrax AMPHENICOLS Chloramphenicol Mechanism of action: inhibition of bacterial protein synthesis by interfering with ribosomes of bacteria Action: bacteriostatic Activity: broad spectrum of antimicrobial activity, but in the process of long use, many bacteria have become resistant. The level of resistance to it in economically developed countries is quite good, because for a long time strictly limited to the application. Among Gr+ flora most sensitive to the drug pneumococcus, (stable penicillin-resistant strains), H. influenzae (including ampicillinresistant strains), E. coli, Salmonella, Shigella, diphtheria, anthrax, brucellosis, plague. Enterococci are not sensitive. From G - flora most sensitive meningococci. The drug has a high activity against spore-forming and asporogenous anaerobes, including B. fragilis. Uses: In all developed countries, their use is strictly limited, mainly meningitis or some other life-threatening infections (e.g., salmonellosis, rickettsial), resistant to other drugs. SIDE EFFECTS: aplastic anemia, bone marrow depression and other disorders of hematopoiesis, pancytopenia, “gray baby syndrome”. Gray baby syndrome The baby stopped feeding, vomited, became hypotonic and hypothermic, abdomen distended, respiration became irregular; cyanosis (gray body) developed in many, followed by cardiovascular collapse and death. It occurs because of inability of the newborn to adequately metabolize and excrete chloramphenicol. Chloramphenicol blocks electron transport in the liver, myocardium and skeletal muscle, resulting in the above symptoms. MACROLIDE ANTIBIOTICS Macrolides and azalides - first place in the application and importance in serious nosocomial infections. Azithromycin is the most widely used antibiotic in the world. Classification - with 14 – membered ring: erythromycin, clarithromycin, roxithromycin; - with 15 - membered ring (azalides): azithromycin; - with 16 - membered ring: spiramycin, josamycin. Mechanism of action: inhibition of bacterial protein synthesis by interfering with ribosomes of bacteria Action: bacteriostatic (azithromycin taken in high doses, has a bactericidal effect; clarithromycin has bactericidal effect on Helicobacter pylori) Activity: Gr- flora: Neisseria, Bordetella pertussis, Legionella, Helicobacter pylori, Haemophilus; Gr+ flora Str. pyogenes, Str.pneumoniae, Str.faecalis. Also effective against Chlamydia, Mycoplasma, Ureaplasma. It is very important that they act on intracellular organisms. Specific adverse reactions: dyspepsia reactions, QT prolongation, hepatotoxicity (more common in erythromycin) As a first choice drug for: 1. Atypical pneumonia caused by Mycoplasma, Chlamydia, Ureaplasma 2. Whooping cough LINCOSAMIDE ANTIBIOTICS Lincomycin, Clindamycin Mechanism of action: inhibition of bacterial protein synthesis by interfering with ribosomes of bacteria Action: bacteriostatic Activity: Anaerobes: Bacteroides (B. fragilis); Gr+ flora: staphylococci, Bacillus anthracis, Corynebacterium diphtheriae. Side effects : diarrhoea and pseudomembranous enterocolitis due to Clostridium difficile superinfection which is potentially fatal. The drug should be promptly stopped and oral metronidazole or vancomycin given to treat it. GLYCOPEPTIDE ANTIBIOTICS Vancomycin Mechanism of action: inhibition of cell wall synthesis Action: bactericidal Activity: very Gr+ (aerobic+anaerobic) Staphylococcus spp. Streptococcus spp., Enterococcus spp. Clostridium difficile. !!!Reserve drugs for the treatment of infections caused by staphylococci (including MRSA, MRSE)!!!! To treat antibiotic- related pseudomembranous enterocolitis and diarrhoea Specific adverse reactions: nephrotoxicity, ototoxicity, Red man syndrome (red neck syndrome)- Rapid i.v. injection has caused chills, fever, urticaria and intense flushing. Note: In concomitant use with Amphotericin b, Aminoglycosides, Colistimethate sodium – increased risk of development and severity of nephrotoxicity, ototoxicity. The use with furosemide - increased risk of ototoxicity ( for all – OTO - and nephro-toxicity). . Aminoglycosides Mechanism of action :They act by interfering with bacterial protein synthesis. Action: All are bactericidal Activity: All are active against aerobic Gr- bacilli and do not inhibit anaerobes. All exhibit ototoxicity and nephrotoxicity. With cephalosporins may increase the risk of development and severity of nephrotoxicity. With Amphotericin b, Vancomycin, Colistimethate sodium – increased risk of nephrotoxicity, ototoxicity. With furosemide– increased risk of the ototoxic actions. Aminoglycosides Classification I Generation : Streptomycin, Kanamycin, Neomycin Mostly Gr - aerobic flora: Enterobacteriaceae, including Escherichia coli, Klebsiella spp., Salmonella spp. Shigella spp. Proteus spp. Serratia spp. Enterobacter spp. Active against M. tuberculosis (streptomycin - the drug of 1st line, kanamycin – 2nd line drug for the treatment of tuberculosis) and some atypical mycobacteria. NO effect on Pseudomonas aeruginosa. II Generation : Gentamicin Gr - aerobic flora, Active against P. aeruginosa (but at present, many strains are resistant) No effect on M. tuberculosis. III Generation : Amikacin, Netilmicin, Tobramycin Gr - aerobic flora Active against Pseudomonas aeruginosa. A reserve antibiotic in case of resistance to therapy with gentamicin IV Generation : Isepamicin Gr - that are resistant to other aminoglycosides Uses Tuberculosis (only 1st gen) Bacterial endocarditis Plague Tularemia Peritonitis Septicaemias OXAZOLIDINONES Linezolid Mechanism of action: inhibition of bacterial protein synthesis by interfering with ribosomes of bacteria Action: bactericidal against streptococci, C. perfringens, B. fragilis; bacteriostatic against staphylococci and enterococci. Activity: Gr+ flora: streptococci, enterococci (including VRE), staphylococci (including MRSA and MRSE) For treatment of MRSA or VRE infections Specific adverse reactions: depression of bone marrow function, thrombocytopenia, peripheral neuropathy, lactic acidosis POLYPEPTIDE ANTIBIOTICS All are powerful bactericidal agents, but not used systemically due to toxicity. Mechanism of action: violation of the integrity of microbial cell membrane Action: bactericidal Against Gr- bacteria only Polymyxin B: a Very toxic drug (nephrotoxicity, neurotoxicity), however, highly effective for the treatment of diseases caused by Pseudomonas aeruginosa → reserve drug. Colistin (polymyxin E). Practically not absorbed in the intestine, and therefore is used for selective intestinal decontamination of sensitive microorganisms Rifamycins Rifampicin, Rifabutin Mechanism of action: disrupts synthesis of RNA in bacterial cells(inhibits the transcription of RNA). Human RNA does not act. Action: bactericidal Activity: Mycobacterium tuberculosis (rifampicin – a 1st line, rifabutin – 2nd line) Rifampicin is also effective for Brucella spp. Chlamydia trachomatis, Legionella pneumophila, Rickettsia typhi, Mycobacterium leprae, Staph. spp. Str. spp. Clostridium spp. Bacillus anthracis, Neisseria meningitidis, Neisseria gonorrhoeae and Gr - flora. Specific adverse reactions: hepatotoxicity note: Due to the rapid development of resistance, drug’s usage should be limited to tuberculosis. MRSA The drug of choice: Vancomycin Also could be used: Linezolid Ceftaroline Doxycycline Clindamycin (for osteomyelitis)