* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 8.0 Assessment and Care Planning for Mood Disorders.
Survey
Document related concepts
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Abnormal psychology wikipedia , lookup
Spectrum disorder wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Schizoaffective disorder wikipedia , lookup
Postpartum depression wikipedia , lookup
Biology of depression wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Major depressive disorder wikipedia , lookup
Causes of mental disorders wikipedia , lookup
History of mental disorders wikipedia , lookup
Mental status examination wikipedia , lookup
Transcript
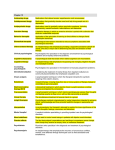
Document Title and Code: Version: Author: Adapted for Local use by: Issue Date: Review date: Authorised by: Policy for Management of Mood Disorders NMA-MD. 2 Prepared by Nursing Matters and Associates. September 2012 September 2014 1.0 Policy Statement: A proactive and person-centred approach to assessment and care planning will be adopted for residents at risk of or who present with mood difficulties. Care will be provided within a framework of promoting health and psychosocial well-being. 2.0 Purpose: The purpose of this policy is to ensure that residents who are at risk of or present with mood problems will be identified and cared for according to their needs, known wishes and preferences. 3.0 Objectives: 3.1 To ensure that nursing staff are aware of the early signs and symptoms of mood disorders for elderly people in residential care. 3.2 To support resident’s needs to find enjoyment and meaning in every day life. 3.3 To ensure that residents presenting with mood problems /disorders will receive the appropriate care according to their individual needs, known preferences and wishes. 4.0 Scope: This policy applies to all nursing and healthcare professionals providing direct care to residents in the Centre. 5.0 Definitions: Page 1 5.1 Mood Disorders: Mood disorders refer to a category of mental health problems that include all types of depression and bipolar disorder. Mood disorders differ from feelings of sadness that may occur occasionally. Mood disorders include major and minor depressive disorders and bi polar disorder. 5.2 Depression: ‘a collective term referring to disorders in which the central feature is a lowering of mood, usually accompanied by reduced ability to enjoy or take interest in one’s usual activities’ (Snowdon, 1998 cited in NHS, Quality Improvement Scotland, 2004). 5.3 Major Depression: To meet criteria for a diagnosis of major depressive disorder, the resident must exhibit at least 1 of 2 symptoms, depressed mood and/or lack of interest, for at least 2 weeks. In the nursing home, older adults are more likely to complain of loss of interest rather than overt depressed mood. For a diagnosis of major depression, the older adult must exhibit an additional 4 or more of the following symptoms for at least 2 weeks. Older adults tend to differ somewhat from middle-aged adults in the presentation of these criteria symptoms: ■ Feelings of worthlessness or inappropriate guilt (guilt is less frequent among older adults than among younger adults) Management of Mood Disorders Policy. September 2012 ■ ■ Diminished ability to concentrate or make decisions Fatigue (a common symptom regardless of age in the moderate to severely depressed and complicated by co morbid Physical illness) ■ Psychomotor agitation or retardation (either can be seen in late life and agitation is frequent in the nursing home) ■ Increase or decrease in weight or appetite (weight loss is very common, whereas weight gain is rarely seen in older patients) ■ Recurrent thoughts of death or suicide (older adults may ruminate about death during a depressive episode although they are not as likely to express suicidal thoughts as younger adults). (Thakur, M and Blazer, D 2008) 5.4 Minor Depression: Minor depression refers to the presence of at least two but not more than four of the symptoms of major depression. It is considered ‘subsyndromal’ but may lead to an increased risk of major depression. Depressive episodes of minor depression may be of two weeks or longer duration but impairment is less severe (Butcher, K and McGonagal-Kenney, M. 2005). 5.5 Psychotic depression is a subtype of major depression that is frequently seen in the elderly patients in long-term care than community samples of the elderly. It is usually characterized by severe depressive symptoms, together with delusions and/or hallucinations. (Thakur, M and Blazer, D. 2008) 5.6 Dysthymic disorder: is a less severe but more chronic variant of depression. To meet criteria the older adult must experience symptoms most of the time for at least 2 years. Although it is rare for dysthymic disorder to start in late life, it can persist into late life from midlife. Therefore, chronic but less severe depression in the nursing home may not so much be secondary to living situation as a pattern laid down many years before admittance to long-term care (Thakur, M and Blazer, D 2008) 5.7 Bipolar Disorder: Previously known as ‘manic depression’ refers a disorder where sufferers have periods (or ‘episodes’) of what is called ‘mania’ and periods of ‘depression’. For this reason, it was once known as ‘manic depression’. It can affect people of any age, from children to older adults (National Institute For Health And Clinical Excellence, 2006) According to the American Geriatrics Society (AGS) any individual over age 60 should be screened for depression periodically. The American Geriatrics Society (AGS) recommends depression screening two to four weeks after admission to a nursing home and then repeated screening at least every six months after admission. In all nursing homes, residents should be screened at least every six months (AGS & American Association for Geriatric Psychiatry [AAGP], 2003; Snowden, Sato, & Roy-Byrne, 2003). In this policy residents should have screening repeated every three months or where there is a significant change in the resident’s condition or where staff suspect that there is a significant change in the resident’s mood. Page 2 Management of Mood Disorders Policy. September 2012 6.0 Management of Mood Disorders -Quick Reference Guide. Screening for Mood Disorders/Problems. Pre admission assessment for presence of mood disorders. Screen the resident on admission using observation and the Centre’s admission assessment form. Ask resident / representative about any history or presence of mood problems/disorders. Where there is a history of or current symptoms suggestive of mood disorders document and discuss with the resident’s GP. Comprehensive Nursing Assessment. o All new residents should have an assessment of mood as part of their comprehensive assessment. o Assessment should be based on resident’s history and updated based on observations during the 5 to 7 days following admission. o Complete Quick Mild Cognitive Impairment Screen (QMCI) or Mini Mental State Exam (MMSE). o Use a formal assessment tool to assess mood status such as the Geriatric Depression Scale or the Cornell Depression Scale. o Geriatric Depression Scale should only be used for residents with an MMSE of 14 or more. o Complete general admission assessment and determine the impact of any mood disorders on the resident’s general health, wellbeing, activities of living and quality of life. Care Planning and Nursing Management. Liaise with resident’s G.P. and/or referring consultant regarding referral to specialist professionals / services. Involve other healthcare professionals involved in resident’s care. Plan care in partnership with resident and /or representative in accordance with resident’s wishes. Identify evidence based strategies in keeping with agreed goals. Develop and document care plan according to resident’s individual needs and preferences. Include strategies to minimise any negative effect of mood disorder on the resident’s level of functioning and improvement in quality of life. Agree review schedule. Communicate care plan to other healthcare staff involved in the resident’s care. Monitoring. Monitor effectiveness of care and adjust care plan as required. Reassess three monthly or more frequently where there is a significant change in care/condition. Liaise with resident’s GP. and other healthcare professionals involved in the resident’s care regarding effectiveness or otherwise of treatment. Amend/ update care plan in accordance with changing needs. Page 3 Management of Mood Disorders Policy. September 2012 7.0 Responsibilities. Actions Responsible Person. This policy will be disseminated to and read by all nursing and healthcare professionals in the facility. Person in Charge/ Director of Nursing. Where a new version of this policy is produced, the previous version will be removed and filed away. Person in Charge/ Director of Nursing. An explanation of this policy will be given on induction to all nursing and care staff. Person in Charge/ Director of Nursing or delegated to another named nurse. Every resident will be assessed on admission for the presence of mood problems /disorders and associated risks factors as part of their initial assessment and every three months or sooner where changes to care or condition indicate. Admitting and/or designated nurse. Assessment and care planning to meet the needs of residents with or at risk of mood disorders will be carried out as per this policy. All registered nurses. For residents with or at risk of mood disorders, a documented care plan will be in place and will include specific nursing interventions to meet the resident’s needs as outlined in this policy. All registered nurses. Nurses will maintain their competence in assessment and care planning and communicate any competency / knowledge deficits to their line manager/Person in Charge. All registered nurses Care given to meet the needs of residents will be in accordance with the plan of care developed and agreed by the resident and / or representative and other healthcare professionals involved in the resident’s care. All healthcare staff providing care to residents. Changes in a resident’s condition will be reported to the senior nurse in charge and changes to care will be communicated to all relevant healthcare professionals. All nurses, care assistants and other healthcare professionals involved in the resident’s care. Page 4 Management of Mood Disorders Policy. September 2012 8.0 Assessment and Care Planning for Mood Disorders. 8.1 Pre admission Assessment: Information regarding any diagnosis of or difficulties with mood disorders will be collected as part of the pre admission assessment. 8.2 Admission assessment. 8.2.1 Each new resident will be screened for the history of or current symptoms of mood problems / disorders as part of the admission assessment. 8.2.2 Information regarding the presence or history of mood disorders will be obtained from: ■ ■ ■ ■ ■ ■ ■ Page 5 The pre admission assessment. Discharge summary. Nursing transfer forms. Referral letters. The resident themselves as far as he / she is able. Family members as appropriate. Observation. 8.2.3 The admitting nurse should listen to what the resident is saying, where possible: Is the resident down-hearted, blue, sad, discouraged, or irritable? Is this resident listless, exhausted, or tired for no apparent reason? Is this resident joyless, feeling hopeless, helpless, and worthless? 8.2.4 The admitting nurse should also observe the residents body language and how he/she behaves or appears: Is the resident slouched with head down or gazing into space? Is the resident slow when answering questions using only one or two words or saying, “I don’t know”? Is the resident giving minimal eye contact? Does the resident have slow body movement, little verbal interaction and difficulty concentrating or thinking clearly? Does the resident display signs of agitation with anxiety e.g. difficulty sitting still; hands wringing; pacing; argumentative? 8.2.5 The resident’s representative should be involved in all assessments where the resident has consented to this. 8.2.6 Where the resident is unable to provide information, the views and observations of the representative should be sought at all stages of assessment. Management of Mood Disorders Policy. September 2012 8.3 Comprehensive assessment. 8.3.1 Comprehensive assessment will take place on admission and will be formally reviewed every three months or where there is a significant change in the resident’s condition. 8.3.2 Where the resident has a previous history of mood disorders, the onset, duration and frequency of symptoms of the condition should be documented on the admission assessment form. 8.3.3 The comprehensive assessment should include a formal assessment for cognitive impairment using the Quick Mild Cognitive Impairment Screen or Mini Mental State Exam. 8.3.4 Comprehensive assessment should also include the use of a formal assessment tool such as the Geriatric Depression Scale (for MMSE scores >14) or the Cornell Scale for Depression in Dementia (MMSE scores<15). For assistance in completing the Geriatric Depression Scale a video demonstrating its use can be found at: http://www.nursingcenter.com/TryThis/Survey.asp?Ep=2&Ch=0 8.3.5 Comprehensive assessment for mood disorders should include the identification of risk factors that may lead to mood problems / disorders. 8.3.6 Conditions related to mood disorders such as systemic and metabolic processes e.g. infection, anaemia, hypothyroidism and so on should be documented as part of the resident’s medical history. 8.3.7 Comprehensive assessment should also identify any nursing problems and needs related to the impact of any mood disorder on the resident’s functional ability and activities of daily living. 8.3.8 Residents with an acquired brain injury may have symptoms directly associated with the injury that can mimic symptoms of depression. These are: Emotional disorders associated with the injury such as apathy, emotional lability may give the appearance of depression in the absence of a depressive illness. Somatic symptoms associated with depression in the normal population such as loss of energy, appetite and libido; altered sleep habits; poor concentration and inability to make decisions. Page 6 8.4 Where a resident has indicators of or diagnosis of depression, the nurse must assess the resident for risk of self harm / suicide as per the Centre’s Policy on Prevention and Management of Self Harm and Suicide. 8.5 The assessing nurse must liaise with the residents’ general practitioner regarding any risks identified and the need for specialist referral. 8.6 If the resident is already attending specialist services, this must be clearly documented in the resident’s care plan. Management of Mood Disorders Policy. September 2012 8.7 Care Planning. 8.7.1 The purpose of care planning is to identify strategies in partnership with the resident to help him/her adapt to health and life changes; support him/her in care transitions such as the move to long-term care and maximise his/her ability to enjoy a meaningful life in the Centre. 8.7.2 The resident’s representative(s) should be encouraged to participate in the care planning process if this is the wish of the resident. 8.7.3 The care planning process should clearly identify agreed goals and wishes of the resident for the future. 8.7.4 Where the resident is unable to participate in the care planning process, this should be documented and the views and observations of the resident’s representative sought. 8.7.5 Care planning should reflect the need for increased support when the resident is faced with any health or life change. 8.7.6 The care planning process should involve other healthcare professionals involved in the resident’s care and address the need for specialist referral where this is indicated. 8.7.7 Where the use of psychotropic medication is indicated the nurse should liaise with the resident’s registered prescriber to agree the lowest starting dose possible, and increasing dosages thereafter until either there is a therapeutic effect, side effects emerge, or the maximum recommended dose is reached. 8.7.8 Where a resident is prescribed psychotropic medication the care plan should include interventions to monitor for potential hypotension, risk of falls, drugrelated cognitive/behavioural function and other adverse effects. 8.7.9 Nurses should liaise with the resident’s prescriber where any of the above mentioned effects are noted. The resident’s psychotropic medication should be reviewed every three months or sooner where any adverse effect is noted. 8.7.10 Where such drugs are prescribed on a PRN as required basis, the indications for giving or withholding the medication, and its effects, must be documented in the resident’s prescription sheet. 8.7.11 The resident’s care plan should address the following aspects of care related to mood disorders: Consent to treatment as far as the resident is able. Any specific safety precautions that may be required, particularly with regard to risk for suicide; psychotic and or violent and aggressive behaviours. Interventions to maximize physical function through a structured exercise/ daily activity plan in accordance with the resident’s ability and preferences. Interventions to enhance social support through encouraging the support of family members; support groups and spiritual support in accordance with his/her religious beliefs. Preventative strategies to address the presence of risk factors that may lead to mood problems / disorders. Page 7 Management of Mood Disorders Policy. September 2012 Interventions to maximise independence and autonomy through active participation in making daily decisions and setting short term goals. Re-inforcement of strengths and abilities. Specific interventions to address loss and any bereavement. This may be related to loss of a loved one, pet, previous lifestyle and roles. Supportive nursing care for assistance with daily activities to include interventions for promoting adequate nutrition; sleep; physical comfort and pain control. Identification of and encouraging involvement in recreational and relaxation activities in accordance with the resident’s needs and known preferences. Provision of emotional support through allowing time to discuss feelings. Administration and monitoring effects of medications and other treatments. (A sample of a simple method of documenting the resident’s mood on a daily basis is provided in the appendices). 8.7.12 The resident’s care plan should be documented and communicated to other relevant healthcare professionals involved in the resident’s care. 8.7.13 Formal reassessment should occur at agreed dates and care amended as required. Page 8 Management of Mood Disorders Policy. September 2012 9.0 Assessment for Risk Factors for and Symptoms of Mood Disorders. Risk Factors: Depressogenic Medications Non-Verbal Cues / Symptoms. Page 9 Current alcohol / substance misuse. Specific co morbid conditions such as dementia; stroke; cancer; arthritis; and other chronic conditions. Functional loss. Social isolation. Hearing, vision and communication difficulties. Recent bereavement. Chronic pain. Incontinence. Transfer to long-term care. Vitamin B12 deficiency. Malnutrition. Sudden onset of disability and life changes associated with acquired brain injury. Altered biochemical balance directly as a result of brain injury. Previous history of mood disorders. Steroids. Narcotics. Sedatives/hypnotics. Benzodiazepines. Anti-hypertensives. Histamine-2 antagonists. Beta-blockers Anti-psychotics. Immunosupressants and cytotoxic agents. Stooped posture. Slowed speech and movement. Lack of interest in self-care. Aggressive behaviour. Unrealistic fears. Repetitive verbalizations such as calling out for help. Agitated shouting, yelling or screaming. Repeated questions. Health related concerns. Foreboding statements. (These are especially common in long-term care facilities). Management of Mood Disorders Policy. September 2012 10.0 References. Health Act (2007) Care and Welfare Of Residents In Designated Centres For Older People) Regulations 2009 Health Information and Quality Authority (2009) National Quality Standards for Residential Care Settings for Older People Brown, El; Raue, PJ; and Halbert, KD (2007) Detection of Depression in Older Adults. University of Iowa Gerontological Nursing Interventions Research Centre. Accessed at www.guidelines.gov Kurlowitcz, L.H. (2003) Depression in Older Adults. In Mezey, M., Fulmer, T., Abraham, I., Zwicker, D.D., editors. Geriatric nursing protocols for best practice 2nd edition. Springer Publishing Company. New York. Mugdha Thakur, MD, and Dan G. Blazer, (2008) Depression in Long-Term Care Journal of the American Medical Directors Association Vol. 9 pp 82– 87. NHS Quality Improvement Scotland, (2004). Best Practice Statement: Working with Older People Towards Prevention and Early Detection of Depression. NHS Quality Improvement Scotland. Butcher, H, and McGonigal-Kenney, M. (2005) Depression and Dispiritedness in Later Life. American Journal of Nursing. December. Vol. 105 (12) pp. 52-61. Hemingway, S. and McAndrew, S. (1997) Acquired Brain Injury: Identifying Emotional and Cognitive Needs. Nursing Standard. Vol. 12(10). Pp. 40-48. Royal College of Physicians Clinical Effectiveness and Evaluation Unit, (2005) National Clinical Guideline. The use of anti-depressant medication in adults undergoing recovery or rehabilitation following acquired brain injury. Page 10 Management of Mood Disorders Policy. September 2012 Appendix 1: Mood and Engagement Chart for Recording Changes in Mood. MOOD Page 11 ME VALUE Very happy, cheerful. Very high positive mood. Content, happy, relaxed. Considerable positive mood. Neutral. Absence of overt signs of positive or negative mood. +5 Small signs of negative mood. -1 Considerable signs of negative mood. Very distressed. Very great signs of negative mood. -3 +3 +1 ENGAGEMENT Very absorbed, deeply engrossed/engaged. Concentrating but distractible. Considerable engagement. Alert and focussed on surroundings. Brief or intermittent engagement. Withdrawn and out of contact. -5 Management of Mood Disorders Policy. September 2012