* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Glycogen
Survey
Document related concepts
Transcript
Glycogen
Glycogen
• Liver
– ~ 4 % 72 g
• Muscle
– ~ 1 % 245 g
• Extracellular glucose
– 0,1 % 10 g
Adult - man 70 kg
His liver 1,8 kg
His muscle mass 35 kg
Blood volume 10 l
2
Glycogen
• Muscle:
– Glucose substrate for
muscle glycolysis
• Liver:
– Glucose store,
– Export of hexose
– Blood sugar
• Glycogenosis
– Deff. Of enzymes
– Muscle weakness N
3
Glycogen level of liver
4
• As a meal containing carbohydrates is eaten and
digested,
• blood glucose levels rise
• pancreas secretes insulin.
• Glucose from the portal vein enters the liver cells
(hepatocytes).
• Insulin acts on the hepatocytes to stimulate the action of
several enzymes, including glycogen synthase.
• Glucose molecules are added to the chains of glycogen
as long as both insulin and glucose remain plentiful. In
this postprandial or "fed" state, the liver takes in more
glucose from the blood than it releases.
• .
5
• After a meal has been digested and
glucose levels begin to fall, insulin
secretion is reduced, and glycogen
synthesis stops.
• About four hours after glycogen begins to
be broken down and converted again to
glucose.
6
Glycogen metabolism
7
Glycogen synthesis
• Muscle
– Hexokinase
• Liver
– Glucokinase
• Phosphoglucomutase
– Glucose-1,6-P cofactor
• Glycogen
– Primer: glycogenin
• 37 kDa glycosilated Tyr
8
Synthesis of glycogen
9
Synthesis of glycogen
glikogenin
10
11
Synthesis of glycogen
12
Glycogenolysis
13
Glycogen
Glygenolysis
Glycogenesis
Glucose-1-P
14
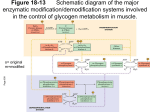
Effect of epinephrin
X
Stimulus
ATP
cAMP
40X
Inakt. Protein Kinase A
Aktive Protein Kinase A
10X
Adrenal cortex
Phosphorylase Kinaseb
Phosphorylase Kinase a
100X
Epinephrin
Glykogen phosphorylaseb
Glykogen phosphorylasea
1000X
Glykogen
Glukose 1 P
10000X
Cent. Nervous syst.
X
R
15
GDP
b
g
a
ATP
GTP
NH2
O
N
H2C
H
O
P
cAMP
N
N
N
O
H
O
OH
O
16
4 cAMP
R
R
R
R
C
C
C
C
18
Protein Kinase Reactions
•Serine-Threonine Kinase / cAMP depentent Protein Kinase
O
O P O
OH
ATP
ADP
O
CH2
CH2
CH
CH
Ser
Serine-Threonine Kinase
Phospho-Ser
O
O P O
OH
ATP
ADP
O
CH3 CH
CH3 CH
CH
CH
Thr
Serine-Threonine Kinase
Phospho-Thr
19
Tein, koffein
cAMP
AMP
PKA
PKA
Phosphorylase-kinase b
Ca2+
Phosphorylase b
Phosphorylase-kinase a
AMP
Phosphorylase a
20
21
Glycogen
Glycogenolysis
Glycogenesis
Glucose-1-P
22
GLYCOGEN SYNTHASE ALSO IS PHOSPHORYLATED
23
Glycogen synthase
• Glycogen synthasea –dephosphorylated
• Glycogen synthaseb –phosphorylated
– 4 identical subunit
– 7 Ser-OH residues/subunit
24
Glycogen synthase
• 6 different protein kinases
–
–
–
–
–
Phophorylase kinase (Ca2+/Calmodulin dep)
Ca2+/Calmodulin dep.
GSK-3:
GSK-4
GSK-5
• Glucose-6-P: allosteric activator of Glycogenesynthase kinaseb
• Insulin/muscle:
– dephosphorylation / activation of Glycogen-synthaseb
25
Protein Kinase
Glycogen Synthase Phosphorylation Site
Phos b Kinase
II
A-Kinase
IA, IB, II, and IV
Ca/Calmodulin - Dependent Protein Kinase
IB, II
Glycogen Synthase Kinase 3
IIIA, IIIB, IIIC
Glycogen Synthase Kinase 4
II
Casein Kinase I
Nearly all sites
Casein Kinase II
V
Protein Kinase C
IA
26
Name
Type
Enzyme Deficiency
Tissues Chiefly
Affected
Clinical Consequences
Von Gierke's Disease
I
Glucose 6-phosphatase
Liver, kidney
Severly enlarged liver, severe
hypoglycemia, lactic acidosis,
ketosis, hyperuricemia,
hyperlipemia
Pompe's Disease
II
1,4-D-Glucosidase (lysosomal)
Liver, heart, muscle
Cardiac failure in infancy
Cori's Disease
III
Amylo-1,6-glucosidase
("Debranching" enzyme)
Liver, muscle
Similar to Type I, but milder
Andersen's Disease
IV
"Branching" enzyme
Liver
Liver cirrhosis, death usually
before 24 months
McArdle's Disease
V
Phosphorylase
Muscle
Muscle cramps, easily fatigued
Hers' Disease
VI
Phosphorylase
Liver
Similar to Type I, but milder
Tarui's Disease
VII
Phosphofructokinase
Muscle
Similar to Type V
VIII
Phosphorylase kinase
Liver
Enlarged liver, hypoglycemia
IX
Glycogen synthase
Liver
27
Von Gierke’s Disease
Glucose 6-phosphatase:
liver and kidney
Here is another liver with a pale, bulging surface. This time the liver is filled
with glycogen in von Gierke's disease, the glycogen storage disease of children.
Severly enlarged liver, severe hypoglycemia, lactic acidosis, ketosis,
hyperuricemia, hyperlipemia
28
POMPE'S DISEASE
Without mannose 6-phosphate
tags, acid maltase
(1,4-D-Glucosidase)
enzyme molecules can't
enter muscle cells from
the bloodstream.
When mannose 6-phosphate
tags are added to acid
maltase enzyme molecules,
the molecules stick to receptors
(docking sites) on the
muscle cells and are
carried deeper inside
the cells, where they're needed.
ENZYME TREATMENT BENEFITS BABIES WITH POMPE'S DISEASE
Babies with a metabolic muscle disorder known as Pompe's disease,
or acid maltase deficiency, usually don't survive infancy because they lack a vital
enzyme that normally breaks down glycogen in the heart and skeletal muscle cells.
Cardiac failure in infancy; liver, heart, muscle
29
Forbe’s disease, Type III glycogenosis
• also called Cori's disease , or glycogenosis
type III rare hereditary disease in which the
the metabolic breakdown of glycogen to the
simple sugar glucose is incomplete, allowing
intermediate compounds to accumulate in the
cells of the liver. Affected persons lack the
enzyme amylo-1,6-glucosidase, one of several
enzymes involved in glycogen breakdown.
Children with the disease have enlarged livers
(which usually…
30
Andersen’s disease
• also called Glycogenosis Type Iv, extremely
rare hereditary metabolic disorder produced by
absence of the enzyme amylo-1:4,1:6transglucosidase (branching enzyme), which is
an essential mediator of the synthesis of
glycogen. An abnormal form of glycogen,
amylopectin, is produced and accumulates in
body tissues, particularly in the liver and heart.
Affected children appear normal at birth but fail
to thrive and later lose…
Liver cirrhosis, death usually before 24 months
31
McArdle's Disease
Phosphorylase stain: Normal
more darkly than type I
Phosphorylase stain: Absent
Muscle fibers stain yellow
Myophosphorylase deficiency: McArdle's disease
32