* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Hyaline cartilage within the trachea:
Survey
Document related concepts
Transcript
Histology lab 2
20/6/2012
Hyaline cartilage within the trachea:
Notice:
The presence of lacunae (both the
cartilage and the bone have lacunae)
At a low magnification the lacunae
appear empty but they are not! During
preparation of the slides the cells shrink, so
we can’t see the chondrocytes (even we can’t see the nuclei of the
chondrocytes because of the low magnification).
The matrix is basophilic (if well stained), the matrix around the lacunae
more deeply stained
In the matrix: we can’t see the fibers why? The ground substance in the
matrix has the same refractive index as the collagen and the few elastic
fibers embedded in it.
Each lacuna contain one,two, three or four chondrocytes (variable number
of chondrocytes), they are called cell nest or isogenous group (because
they came from the same cell).
1
Histology lab 2
20/6/2012
The chondrocytes “inside the lacunae” shrink during the preparation of
the slide, what we see is the nucleui "("بقايا الخليةin this slide we can see the
nuclei inside the lacunae but in the previous one we can’t).
The matrix:
1. Territorial matrix: around the lacuna, more
deeply stained indicating high concentration
of chondroitin sulphate.
perichondrium is present in
2. Interterritorial matrix.
MOST places of hyaline
Able to regenerate if damaged?
cartilage.
Yes, because of the presence of the
perichondrium.
NOTE:
If the perichondrium is
absent, the cartilage will not
Location:
Most of the skeleton of the fetus “the cartilage
will die and be replaced by bone later on”
be able to regenerate if
damaged.
Articular cartilage: doesn’t have perichondrium
so unable to regenerate
Gets its nutrients by diffusion from the synovial fluid
“inside the joint”.
Respiratory canals : trachea, larynx, nose,bronchi…
Costal cartilage
Cartilage growth:
1. Appositional(exogenous): cartilage grows by adding to its
periphery, perichondrium controls this type of growth
2. Interstitial (endogenous): chondrocytes within lacunae produce
matrix they are pushed away from each
other thus enlarging the cartilage from
What is the function of the
inside.
pointed cell “1”?
*** articular cartilage!!! Doesn’t undergo
Production of matrix
both types of growth, doesn’t have
(collagen type 2, GAGs,
proteoglycans, few elastic
2
fibers)
Histology lab 2
20/6/2012
appositional growth and its chondrocytes can’t give matrix (especially
in adults) so can’t have interstitial also.
Chondrogenic cells: in the inner cellular perichondrium
Derived from mesenchymal cells
Differentiate into chondroblasts and osteoprogenitor
cells.
The pointed cell “2” has the following features:
a. Derived from mesenchyme
b. Differentiate into chondroblasts
e is the
correct answer
c. Differentiate into osteoprogenitor cell
d. A+b only
e. All of the above
Hyaline cartilage
(articular)
A section in vertebra
The vertebrae are composed of
spongy bone which is covered by a
thin layer of compact bone then it
is covered by hyaline cartilage.
Between the vertebrae we have the intervertebral disks
3
Histology lab 2
20/6/2012
Elastic cartilage
at low magnification: The lacunae
appear empty because the cells shrink
during preparation
we can see the pericondrium, that
means that elastic cartilage can
regenerate.
On a higher magnification, the matrix
is
full of elastic fibers when stained with
“orcein”, they appear as black masses
Chondrocytes are mostly found single
in
lacunae but that doesn’t mean that we
don’t have isogenous groups
Yellow in the fresh state due to the
presence of elastic fibers
It
never calcify or ossify because that
will reduce its elasticity and it must
remain elastic
Location: external ear, ear pinna, Eustachian tube epiglottis
The black masses are composed of fibers, that will be
clear if we noticed a less condensed place. "elastic fibers" هذه الكتل مكونة من خيوط
4
Histology lab 2
20/6/2012
هذه الكتل هي عبارة عن ألياف مزدحمة
Elastic fibers can form:
Fibers
Bundles
Fenestrated sheets
Here it forms fibers.
Fibrocartilage
vertebra هذه العينة مصورة من ساليد باهت جداً لكنها عبارة عن
The second picture is part of the first one “the fibrocartilage alone”
Fibroblasts differentiate into chondroblasts which differentiate into
chondrocytes.
If the stain was deeper “if it was typically stained”, the matrix should
appear pink because of the presence of type1 collagen and few GAGs.
Location:
Intervertebral disc
TMJ (Temporomandibular joint)
Symphysis pubis
Labrum in the shoulder joint
Sometimes at the end of the tendon
Perichondrium absent
5
Histology lab 2
20/6/2012
Fibrocartilage never exist alone, we can find it next to
Hyaline cartilage “between vertebrae”.
Dense regular connective tissue tendon.
Bone
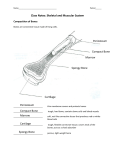
Histological sections of bone can be prepared by 2 methods:
1- Grounding:
We can see haversian systems “osteones”, which are composed of
concentric lamellae.
haversian canals which contain blood vessels and nerves
Canaliculi
The lacunae appear as black spaces, we can’t see the cells because
they are destroyed and the lacunae are filled with debris
** lamella is the space between 2 lacunae
This slide is also prepared by
grounding
When the lamellae are arranged
horizontallyit is called inner or
outer circumferential lamellae( the
layers that surround the inner and the
outer surfaces of compact bone,
6
Histology lab 2
20/6/2012
holding the many haversian canals together).
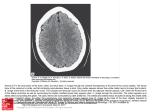
2-
Decalcification:
We can see osteones”haversian
systems”
We can see the osteocytes (their
nuclei) or at least we can see
empty lacunae(remember that in
the grounding method, the
lacunae appear as black spaces)
We can’t see the canaliculi
We won’t see osteoclasts?!
Osteocytes are the most
Compact GROUND bone
numerous cells in the bone
Ink injected
Volkmann’s canal passing perpendicular
to the long axis of the bone provides
communication between the Haversian
canals, provides the osteocytes with the
nutrients they need by way of the tissue
fluid that permeates the canaliculi
Spongy bone
The structural unit of the spongy bone is the trabeculum which is composed of
irregular lamellae
The lamella is the space between two lacunae
7
Histology lab 2
20/6/2012
Its easy to differentiate between the
spongy and the compact bone
Spongy has trabecula
Compact has haversian systems
The cavities between the trabecula is filled
with bone marrow (in adults) but here we
don’t have bone marrow (bone marrow
يظهر كمجموعة مزدحمة من الnuclei)
This section is from an embryo so we have primitive mesenchymal tissue that
will form the bone marrow later on.
Osteocytes inside lacunae between lamellae forming
trabeculum.
Osteocytes are connected with each other by canaliculi
On the surface of the trabeculum:
A cell with one nucleus
osteoblast
A cell with many nuclei
osteoclast “it is a multinuclear
macrophage”
Osteocytes are not completely
inert they can produce matrix ()لتعويض العظم
Osteoblast
Function: synthesis of organic compounds
8
Histology lab 2
20/6/2012
location? On the surface of trabeculum
Surface of calcified cartilage
Derived from osteoprogenitor cells (which are derived from chondrogenic
cells)
Cytoplasm “if stained properly” basophilic because it is a protein
producing cell (producing collagen type1 and proteoglycans)
Have receptors for the parathyroid hormone
Binding with the receptor will cause the activation of osteoblast to produce
osteoclast stimulating factor that will go through the blood to the osteoclasts
where it can bind to its receptors stimulating the osteoclasts to start resorption
The trabeculum contains the following except
a- Lamellae
b- Osteocytes inside lacunae
c- Proteoglycans
The answer is
e
d- Collagen type1
e- Osteoprogenitor cells
Each bone in our body starts as a spongy bone then it may convert to compact
bone or stay a spongy bone.
Where to find spongy bone?
The ends of the long bones (the head of the humerus, femur)
Center of flat and irregular bone(center of scapula and vertebra)
Osteoclasts
Multinuclear macrophages
Monocytes “uninuclear cells” form osteoclasts by:
Fusion of monocytes
9
Histology lab 2
20/6/2012
Division of the nucleus of the monocyte repeatedly without the
division of the the cytoplasm
Function: bone resorption what for?!
Remodeling: in the growth period of the body
Maintain the ionized calcium level in the blood
Osteoclasts have receptors for
Osteoclast stimulating factor
Calcitonina hormone produced from the thyroid gland,
deactivating the osteoclast
Calcitonin : Important for people who have osteoporosis
the bone is changing continuously, but there is balance between the activatity
of the osteoclasts and osteoblasts to keep it within normal limits.
In osteoporosis the activity of the osteoclasts increases and the mass of the
bone decreases
So calcitonin is important to reduce the activity of the osteoclasts.
Notes:
Lamina reticularis contains type 1 and 3 collagen
**remember that wherever type 1 is present there is type 5 but we say
mainly type 1 and 3
Calcitonin is hormone that doesn’t have any function physiologically but
pathologically like in the renal failure for example it decreases the activity
of the osteoclasts
Calcitonin is secreted from special cells in the thyroid gland
The parathyroid hormone is secreted from the parathyroid
gland
10
Histology lab 2
20/6/2012
Osteoclast stimulating factor have high levels in the blood of a patient with renal
failure.
Renal failure causes losing calcium and other materials after a long period of
time the patient will suffer from low calcium concentration in blood (chronic
hypocalcemia) which will activate the parathyroid gland to produce parathyroid
hormone to activate osteoblast to produce osteoclast stimulating factor which
stimulates the octeoclasts to start resorption
And that can affect the strength of bones causing osteoporosis.
Prostaglandins are a large family, some of its members can cause
vasodilation and others can cause vasoconstriction.
Fibrocartilage doesn’t calcify or ossify
Calcification occurs for hyaline cartilage like thyroid cartilage in the
larynx, and that will make it harder
Fibrocartilage and elastic cartilage don’t calcify or ossify.
Epidermal cells are stratified sqamous epithelial cells
Collagen is usually formed by connective tissue cells
Fibroblast collagen type 1
Osteoblast collagen type 2
But type 7 is an exception, it is formed by epidermal cells, scientists used
to think that it is produced by the dermis but it is produced by deep cells
of the epidermis “an exception”.
Anaphylactic reaction: a severe allergic reaction to the degree of shock
Decrease in blood pressure
Excessive vasodilation
The blood will not reach the brain
It may cause death
Adhesive glycoprotein:
They allow the cells to bind to the components of the matrix, there are
many types of adhesive proteins like laminin and entactin(in the lamina
lucida of lamina basialis).
11
Histology lab 2
20/6/2012
Integrins (cell surface proteins that can bind to laminin and entactin)
Laminin and entactin “also other glycoproteins” will adhere cell
membrane “integrins” to the lamina densa).
Done by: Lubna Hamdan
12