* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 7
Survey
Document related concepts
Transcript
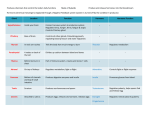
Berthold Endocrine Experiment Removereplacementinjection Objectives 1. Chemical classes of hormones 2. Biosynthesis of a particular hormone 3.Transport of the hormones 4.Recognition & signaling of the hormone 5.Functions of the hormones. 6.Degradation of the hormone. Endocrine Methods • • • • • • • • • Remove-replacement-injection Purification and cloning Synthesis and production of hormone Test biological activity with pure hormones Development of antibodies Localization by immunocytochemistry Establish assays (RIA) Microarray,deep sequencing, proteomics Knock-out/Knock down/mutants Hormone Types/Functions Three structural divisions: 1) Amines--H2O sol. (small--AA) catecholamines and thyroid hormones 2) Steroids--lipid sol. cyclic hydrocarbon derivatives from cholesterol 3) Peptide/protein -- H2O sol. largest, complex Amines • Hormones derived from tyrosine and tryptophan. • Include hormones secreted by adrenal medulla, thyroid, and pineal glands. Thyroid Hormones • Tyrosine derivatives bound together. • Contain 4 iodine atoms (T4). • Contain 3 iodine atoms (T3). • Small, non-polar molecules. – Soluble in plasma membranes. Steroids • Lipids derived from cholesterol. • Are lipophilic hormones. – – – – Testosterone Estradiol Cortisol Progesterone Peptides/Proteins • Chains of amino acids (< 100 amino acids in length). – ADH – Insulin • Long polypeptides (>100) bound to one or more carbohydrate groups. – FSH – LH Biosynthesis of Peptides and Protein Hormones DNA (The gene) RNA (Primary transcript) RNA processing mRNA translation Pre-(Pro)-hormone Proteolysis via signal peptide cleavage Pro-hormone Proteolysis via second modification Glycosylation Hormone phosphorylation Proopiomelanocortin (POMC) gene 5’ 5’ N 1 Signal peptide 3’ 3’ mRNA 2 3 4 4 ACTH 5 6 7 6 C 7 Products in corticotrophic cell of the anterior pituitary b-lipotropin 6 g-MSH a-MSH CLIP g-lipotropin 8 Products in the intermdeiary gland b-endorphin b-MSH MET-enkephalin Classification of chemical communication systems 1) Autocrine--secretion that affects the same cell which the secretion originated Ex: Adrenergic nerve endings 2) Paracrine--secretion that affects neighboring cells Ex: Inflammatory response 3) Endocrine--a secretion of a chemical substance that is released into the blood and affects a distant target 4) Exocrine--secretion of a substance that is released onto surface of animal--including internal structures Exocrine Glands/tissues: --possess ducts --salivary glands, intestinal epithelium, secretory cells in stomach, and secretory cells of the liver and pancreas Endocrine Glands/tissues: --lack a definite duct --Adrenal gland, GI tract, heart, kidney, ovary, pancreas, thyroid, pituitary, placenta, testes, and thymus Hypothalamus Bone Hypothalamus Optic chiasm Anterior lobe of pituitary Connecting stalk (infundibulum) (b) Posterior lobe of pituitary (a) Anterior pituitary Posterior pituitary Fig. 7-8, p.265 Anterior and posterior pituitary glands. Posterior Pituitary • Also called the neurohypophysis. • Formed by down growth of the brain during fetal development. • Is in contact with the infundibulum. • Nerve fibers extend through the infundibulum. Anterior Pituitary • Master gland (also called adenohypophysis). • Derived from a pouch of epithelial tissue that migrates upward from the mouth. • Consists of 2 parts: • Pars distalis: anterior pituitary. • Pars tuberalis: thin extension in contact with the infundibulum. Hypothalamic Control of Posterior Pituitary • Hypothalamus produces: – ADH: supraoptic nuclei. – Oxytocin: paraventricular nuclei. • Hormones transported along the hypothalamohypophyseal tract. • Stored in posterior pituitary. • Release controlled by neuroendocrine reflexes. Posterior Pituitary (neurohypophysis) --releases neurohormones 1) antidiuretic hormone (vasopressin) 2) oxcytocin Larhammar et al, Ann. N.Y. Acad. Sci. 1163: 201–208 (2009) Hypothalamic Control of the Anterior Pituitary • Hormonal control rather than neural. • Hypothalamus synthesizes releasing hormones and inhibiting hormones. • Hormones are transported to axon endings of median eminence. – Delivers blood and hormones to anterior pituitary via portal system. Hypothalamic Control of the Anterior Pituitary • Hormones secreted into the hypothalamohypophyseal portal system regulate the secretions of the anterior pituitary. Feedback Control of the Anterior Pituitary • Anterior pituitary and hypothalamic secretions are controlled by the target organs they regulate. • Negative feedback inhibition by target gland hormones. Feedback Control of the Anterior Pituitary • Negative feedback at 2 levels: – The target gland hormone can act on the hypothalamus and inhibit releasing hormones. – The target gland hormone can act on the anterior pituitary and inhibit response to the releasing hormone. Fig. 7-11, p.269 Fig. 7-12, p.270 Water vs. Lipid Water soluble hydrophilic external (2nd mess.) external receptors short half-life intermediary resp. protein activation Lipid soluble hydrophobic internal cytoplasmic rec. long half-life Long-term resp. gene activation Mechanisms of Hormone Action • Hormones of same chemical class have similar mechanisms of action. – Location of cellular receptor proteins. • Target cell must have specific receptors for that hormone (specificity). • Hormones bind to receptors with high bond strength (affinity). • Low capacity of receptors (saturation). Hormones That Bind to Nuclear Receptor Proteins • Lipophilic steroid and thyroid hormones bound to plasma carrier proteins. • Hormones dissociate from carrier proteins to pass through lipid component of the target cell membrane. • Receptors for the lipophilic hormones are known as nuclear hormone receptors. Nuclear Hormone Receptors • Function within cell to activate genetic transcription. • mRNA directs synthesis of specific enzyme proteins that change metabolism. • Receptor must be activated by binding to hormone before binding to specific region of DNA called HRE (hormone responsive element). – Located adjacent to gene that will be transcribed. Mechanisms of Steroid Hormone Action • Steroid receptors located in cytoplasm. • Bind to steroid hormone. • Translocates to nucleus. • DNA-binding domain binds to specific HRE of the DNA. • Dimerization occurs. • Stimulates transcription. Mechanism of Thyroid Hormone Action • Receptor proteins located in nucleus. • T3 binds to ligand-binding domain. • DNA-binding domain can then bind to the half-site of the HRE. • Other half-site is vitamin A derivative 9-cisretinoic acid. • Two partners can bind to the DNA to activate HRE. Hormones That Use 2nd Messengers • Cannot pass through plasma membrane. • Catecholamines, polypeptides, and glycoproteins bind to receptor proteins on the target cell membrane. • Actions are mediated by 2nd messengers (signal-transduction mechanisms). – Extracellular hormones are transduced into intracellular second messengers. Hormones That Use 2nd Messengers 2nd messenger systems: • Adenylate cyclase • Phospholipase C • Tyrosine kinase • NO • various kinases Adenylate Cyclase-cAMP • Hormone binds to receptor protein. • Dissociation of a subunit of G-protein. • G-protein binds and activates adenylate cyclase. • ATP cAMP + PPi • cAMP attaches to inhibitory subunit of protein kinase. Adenylate Cyclase-cAMP • Activates protein kinase. • Phosphorylates enzymes within the cell to produce hormone’s effects. • Modulates activity of enzymes present in the cell. • Alters metabolism of the cell. • cAMP inactivated by phosphodiesterase. – Hydrolyzes cAMP to inactive fragments. Catecholamines ACTH FSH LH TSH Glucagon PTH Calcitonin ++ Phospholipase-C-Ca • Binding of epinephrine to alpha-adrenergic receptor activates a G-protein, (phospholipase C). • Phospholipase C splits phospholipid into inositol triphosphate (IP3) and diacylglycerol (DAG). • Both derivatives serve as second messengers. ++ Phospholipase-C-Ca • IP3 diffuses through cytoplasm to ER. • Binding of IP3 to receptor protein in ER causes Ca++ channels to open. • Ca++ diffuses into the cytoplasm. • Ca++ binds to calmodulin. • Calmodulin activates specific protein kinase enzymes. • Alters the metabolism of the cell, producing the hormone’s effects. Catecholamines TRH LHRH Oxytocin ADH Two ways to increase cytosol free Ca 2+ 1)By release of Ca2+ from intracellular Calcium storages 2)By influx of Calcium from cell exterior Ca2+ channel Tyrosine Kinase • Receptor protein on cell membrane is tyrosine kinase. • Insulin receptor consists of 2 units that dimerize when they bind with insulin. • Insulin binds to ligand–binding site, activating enzymatic site. • Autophosphorylation occurs, increasing tyrosine kinase. • Activates signaling molecules, altering the metabolism of the cell. GH/PRL signaling mechanism PRLR alpha PRL Extra-cellular PRL PRL D1 D2 Intra-cellular Stat P P R L Circulation P R L D1 D2 JAK2 P R L P R L JAK2 P Box1 Box1 P P P Y Y Y Y Y Y Y Y P P P Legend Stat 1 Kinase Stat 3 Stat 5 Signal Molecule PI3K Fyn Src MAPK Known Not Sure Biological Response AKT ? AKT ERK OVERVIEW Physiological Effects of Hormones 1. Reproduction (Gonads) 2. Stress & Steroids (Adrenal) 3. Metabolism (Pancreas and Thyroid) 4. Electrolyte/Water Balance Gonads and Placenta • Gonads (testes and ovaries): – Secrete sex hormones. • Testosterone. • Estradiol. • Progesterone. • Placenta: – Secretes large amounts of estrogen and progesterone. Sertoli cells: synthesis androgen-binding protein and inhibin. Leydig cells: produce and secrete testosterone Testosterone: key hormone for produce sperm, develop male sex characters, protein synthesis and general growth s Cell type Ploidy/Chro mosomes #N Oogonium diploid/46 2N primary Oocyte diploid/46 4N secondary Oocyte haploid/23 2N Ovum 1N haploid/23 Process Oocytogenesis (mitosis) Time of completion third trimester Dictyate in Meiosis I prophase I until (Folliculogenesis) ovulation Halted in metaphase II until Meiosis II fertilization 1. hypothalamic GnRH control of FSH / LH release, 2. ovarian follicular development to ovulation and subsequent corpus luteum formation 3. the feedback control of FSH / LH secretion by ovarian hormones. •the corpus luteum regresses, •there is a rapid fall in the secretion of oestrogen and progesterone, •the endometrium undergoes shrinkage due to extracellular fluid loss, •the spiral arteries constrict, •the endometrial blood flow decreases with cell death and destruction of blood vessels ` Adrenal Glands • Paired organs that cap the kidneys. • Each gland consists of an outer cortex and inner medulla. • Adrenal medulla: – Derived from embryonic neural crest ectoderm (sympathetic ganglia). – Synthesizes and secretes: • Catecholamines (mainly epinephrine but some norepinephrine). Adrenal Medulla • Innervated by sympathetic nerve fibers. – Increase respiratory rate. – Increase heart rate, cardiac output; and vasoconstrict blood vessels, thus increasing venous return. – Stimulate glycogenolysis. – Stimulate lipolysis. Adrenal Glands • Adrenal cortex: – Does not receive neural innervation. – Must be stimulated hormonally. – Consists of 3 zones: • Zona glomerulosa: – Aldosterone: regulate Na+ and K+ balance. • Zona fasciculata: – Cortisol: regulate glucose metabolism. • Zona reticularis: – Androstenedione and DHEA: supplement sex steroids. Pancreas • Endocrine portion consists of islets of Langerhans. • Alpha cells secrete glucagon. – Stimulus is decrease in plasma glucose concentrations. – Stimulates lipolysis. • Beta cells secrete insulin. – Stimulus is increase in plasma glucose concentrations. – Promotes entry of glucose into cells. Regulating Blood Glucose Two major hormones: 1) insulin 2) glucagon Origin:b cells, a cells-islet of Langerhans Control: BG high--insulin, BG low--glucagon Diabetes Mellitus Two types: 1) Type I (IDDM) --severe, insulin dependant, juvenile onset, --loss of beta cell mass 2) Type II (NIDDM) --less severe, non-insulin-dependant, adult onset, more common --defective insulin receptors untreatedfat metabolism(ketones) ketoacidosis ketoacidosis Thyroid Hormones • Thyroid gland located just below the larynx. • Thyroid is the largest of the pure endocrine glands. • Follicular cells secrete thyroxine. • Parafollicular cells secrete calcitonin. Production of Thyroid Hormones • I- (iodide) actively transported into the follicle and secreted into the colloid. • Oxidized to (Io) iodine. • Iodine attached to tyrosine. – Attachment of 1 iodine produces monoiodotyrosine (MIT). – Attachment of 2 iodines produces diiodotyrosine (DIT). • MIT and DIT or 2 DIT molecules coupled. Production of Thyroid Hormones • T3 and T4 produced. • TSH stimulates pinocytosis into the follicular cell. – Enzymes hydrolyze to T3 and T4 from thyroglobulin. • Attached to thyroid-binding protein and released into blood. T3 Effects • Stimulates cellular respiration by: – Production of uncoupling proteins. – Stimulate active transport Na+/ K+ pumps. – Lower cellular [ATP]. • Increases metabolic heat. • Increases metabolic rate. – Stimulates increased consumption of glucose, fatty acids and other molecules. Hormonal Regulation: H2O, Electrolytes Major organs: kidney, intestine, and bone Antidiuretic hormone (ADH): also vasopressin, regulates H2O turnover in kidney -- premeability of H2O in duct ( urine) Aldosterone: Na+ reabsorption, blood osmolarity Atrial natriuretic peptide (ANP): Na+ , ( urine)