* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular Complications
Baker Heart and Diabetes Institute wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart failure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Coronary artery disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
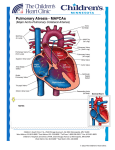
Cardiovascular Complications Liu Wei Department of Ob & Gy Ren Ji hospital General Consideration • Cause of mother death The 2nd cause • Incidence 1%-4% General Consideration • Antenatal cardiovascular changes 1. Blood volume increase by 40%-60% Peaking at 32 –34 weeks the expansion in plasma volume is greater than that expansion of red cell mass. 2. Cardiac output Increase by 40%-50% Peaking at 20-24 weeks General Consideration 3. Blood pressure Decrease in the first trimester Rise to prepregnancy levels in the third trimester 4. Heart size Ventricular chamber size is increased Systolic function is unchanged. General Consideration • Intrapartum cardiovascular changes 1. First-stage labor 300ml –500ml↑(each contraction) Cardiac output↑(maternal pain, anxiety) 2. Second-stage labor Lung circulation↑(bearing-down efforts to expel the fetus) Venous return↓(after fetus is deliveried) Placental circulation is lost (after placenta is deliveried) General Consideration 3. Postpartum Circulating blood volume↑(Placental circulation is lost) Circulating blood volume further↑(mobilization of extravascular fluid into the vascular system) Types of Cardiovascular Complication • Congenital heart disease先心: the most frequent 1. Left to right shunting左向右分流型 1) Atrial septal defect (ASD)房缺: most common asymptomatic (most patients); pulmonary blood flow↑(lesion ≥2cm2) → pulmonary hypertension → Eisenmenger’s syndrome 2) Ventricular septal defect (VSD)室缺 tolerated (small lesion); left ventricular hypertrophy→ pulmonary hypertension→ biventricular hypertrophy Types of Cardiovascular Complication 3) Patent ductus arteriosus (PDA)动脉导管未闭 rare (early surgical repair); hemodynamic consequence are similar to VSD 2. Right to left shunting右向左分流型 1) Tetralogy of Fallot法洛氏四联征 Pulmonary stenosis, right ventricular hypertrophy, large ventricular septal defect and overriding aorta the most common cyanotic lesion complicating pregnancy Types of Cardiovascular Complication 3. Non-shunting 1) Pulmonary stenosis Not usually progressive 2) Aortic stenosis rare; its outcome is bad 3) Marfan’s syndrome (genetic disorder) Myxomatous degeneration of the heart valves; mitral and cystic medial necrosis(囊性中层 坏死) of the aorta (aneurysms动脉瘤) death rate: 4%-50% Types of Cardiovascular Complication • Rheumatic heart disease 1. Mitral stenosis is the most common lesion. 2. Severe lesion with pulmonary hypertension→ pulmonary edema → hear failure: terminate the pregnancy • Heart disease caused by preeclampsia Left heart failure (increased blood pressure and cardiac muscle ischemia) Types of Cardiovascular Complication • Peripartum cardiomyopathy 1. Congestive cardiomyopathy (during the late stage of pregnancy (3 months) or within the first 6 months postpartum) 2. Absence of other causes of heart failure 3. Its etioloty is uncertain 4. Manifestations: symptoms caused by heart failure and embolism 5. The risk of maternal mortality is 30%-50%. Types of Cardiovascular Complication • Myocarditis 心肌炎 1. Manifestation: arrhythmia心律失常 2. Sequelae of myocarditis心肌炎后遗症: more common Effects on fetus • Preterm labor, fetal death, fetal distress • Drug used • Inherited problem Ventricular septal defect (VSD): 22% Marfan’s syndrome: 50% Diagnosis • Etiology diagnosis congenital or rheumatic or preeclampsia or peripartum cardiomyopathy • Anatomy diagnosis ASD or VSD or PDA or mitral stenosis or mitral regurgitation • Pathophysiology diagnosis pulmonary hypertension or Eisenmenger’s syndrome or arrhythmia • Functional classification Class: I—IV Diagnosis • more significant signs 1. History: palpitation(心悸), short breath, heart disease 2. Orthopnea (端坐呼吸), chest pain, expectoration of blood (咯血) 3. Cyanosis紫绀, diastolic murmur舒张期杂音 4. Arrhythmia 5. Enlargement of heart (chest x-ray film) 6. Echocardiogram: chamber enlarge, hypertrophy, abnormality of valve Functional classification of heart disease • 1. 2. 3. New York Heart Association (NYHA) Class I: asymptomatic Class II: symptoms with normal activity Class III: symptoms with less than normal activity 4. Class IV: symptoms at rest • Revised guideline According to the result of objective testing (chest x-ray, EKG, echocardiogram) early diagnosis of heart failure • Palpitation and short breath with less than normal activity • HR>110, R>20 at rest • Orthopnea at night • Persistent wet rale in lung Judgment of safety of pregnancy • 1. 2. 3. 4. 5. 6. 7. 8. 9. Conception should be prevented if: Severe heart disease Functional classification: class III-IV History of heart failure Pulmonary hypertension Right to left shunting Severe arrhythmia rheumatic fever风湿热 Combined valve disease Acute myocarditis Treatment • Antenatal treatment 1. Termination of pregnancy: Terminate before 12 weeks (cases not suitable to pregnancy) 2. Antenatal supervise: regular and intensive and early (early pregnancy) 3. Prevention of heart failure 1) sufficient rest 2) weigh control 3) preventing infection, correcting anemia and arrhythmia Treatment 4. 1) 2) 3) 4) Treatment of heart failure Cardiotonic强心: digoxin Vascular dilation Diuretic利尿 Caesarean section Treatment • Intrapartum treatment 1. Method of delivery: CS 2. First stage calm down, ataractic(镇静剂), oxygen supplement 3. Second stage Operative vaginal delivery 4. Third stage Preventing postpartum hemorrhage 5. Puerperium Preventing infection END