* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download RAD 204 PATHOLOGY
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Heart failure wikipedia , lookup
Aortic stenosis wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
RAD 204 PATHOLOGY
COLLEGE OF MEDICAL SCIENCES/RADIOLOGICAL
SCIENCES DEP’T
LECTURE 5:
CARDIOVASCULAR PATHOLOGY
WEEK OF OCTOBER 6, 2013
DR SHAI’
part 1 of 2
STRUCTURE &
OBJECTIVES
Companion lecture to this lecture: link available on http://health141.yolasite.com/
you are required to have a print or e-version of the companion lecture during this lecture
congenital abnormalities of the heart
atherosclerosis, ischaemic heart disease, hypertension
valve disorders & aneurysms
diseases of the myocardium, pericardium
inflammatory and neoplastic disease
radiological diagnostics in cardiovascular pathology: FORMAL PROJECT 1 Due: November 5,
2013
mid term exam: 2nd week after Hajj holiday, in class, during class time. {mcq, short answer}
the project
http://emedicine.medscape.com/radiology
> CARDIAC
choose from list of cardiac imaging list and use (but do not copy/paste) this site, as ONE OF
MANY credible references > submit a formal report with references on the pathology of the
condition and a COMPREHENSIVE explanation of
imaging techniques used in the condition
DUE NOVEMBER 5, 2013
radiological diagnostic and therapeutic interventions
OR
http://my.americanheart.org/professional/Education/ProfessionalEducation_UCM_426265_WidgetListPage.jsp (MAIN PAGE) CLICK imaging techniques &
application >> register and take this course
http://learn.heart.org/ihtml/application/student/interface.heart2/index2.html?searchstring=56
70
register and complete course> take screen shot of your progress & results > submit
mid term exam
WHEN: 2nd week after Hajj holiday
WHERE: in class, during class time
TOPICS: terminology, basic pathology, cell damage,
repair, & response to injury, inflammation and healing,
CVS pathology
STYLE: Multiple Choice Questions, Short Answer
Questions, Read an Article & answer questions on the
article
TIPS: see the http://health141.yolasite.com/ for
lectures and articles
congenital heart
abnormalities
define congenital
prevalence: 8/1000 live births
aetiology:
idiopathic/sporadic: most cases
maternal: rubella, alcohol abuse, intrauterine radiation, drugs eg thalidomide
genetic/ chromosomal: eg. Trisomy 21 {Down’s Syndrome}
clinical presentation:
apparent at or shortly after birth ~heart failure
sequelae > cyanosis, dyspnoea, feeding difficulties, failure to thrive
types of congenital HD
abnormal shunting of blood b/w LEFT & RIGHT sides of
heart
left - to - right more common b/c high pressure in lt
heart
right - to left shunts from increased resistance to blood
moving out of rt heart
obstruction to blood flow
left
to
right
shunts
malformations > shunting blood from left to right side of
heart
commonest group of congenital heart abnormalities
from high pressure in lt. side
blood does type
NOT bypass lungs%soofno
cyanosis
all CHD abnormalities
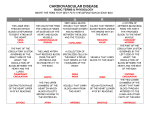
Ventricular Septal Defect
25-30
Atrial Septal Defect
10-15
Patent Ductus Arteriosus
10-15
AV Septal Defect
5
ventricular septal defects
VSD: defect of INTERventricular septum
INTERventricular septum: membranous (fibrous) portion & muscular portion
size & site of defect determines extent of shunt
presents as cardiac failure in infants or murmur in older children/adults
signs:
pansystolic murmur {flow from high pressure left ventricle to low pressure right ventricle
during systole}
tachypnoea (increased respiratory rate)
indrawing of lower ribs on inspiration
Management: small defect : no treatment, close spontaneously. large defects: surgical
repair.
atrial septal defects
females more than males 2:1
defect of INTERatrial causing shunting to RIGHT with enlargement of RT heart &
pulmonary arteries
usually at fossa ovalis (incompletely closed ostium secundum defect)
clinical features: most children are symptom free for years, detected at routine clinical
exam & CXR
some children dyspnoea, chest infections, cardiac failure, arrythmia (eg atrial
fibrillation)
signs: from volume overload of rt ventricle
systolic flow murmur over pulmonary valve
wide splitting of 2nd Heart Sound (delayed closure of pulmonary valve, from
increased stroke volume and Rt Bundle Branch Block)
diastolic rumbling murmur (increased flow across tricuspid valve)
Mgmt: surgical closure otherwise RV hypertrophy & pulm. hypertension
patent ductus arteriosus
persistence of embryological connection between AORTA & pulmonary trunk {Lt.
main pulmonary artery}
OPEN ductus arteriosus in 10% CHD, females more than males
associated with maternal Rubella infection
EMBRYOLOGY: intra uterine life
ductus arteriosus allows Oxygenated Placental Blood to flow from Pulm. Artery
to Aorta (BYPASSING LUNGS)
@ birth: pulmonary vasculature resistance declines, blood is diverted to lungs
for oxygenation and ductus arteriosus closes within 1st few days of life
BUT: if ductus stays patent> blood continually shunted from aorta to pulm
artery
up to 50% LV output may be recirculated through lungs, with increase work on
heart
pda
clinical features:
depends on size of the left - to right shunt
small shunts: asymptomatic , large: retarded growth
& development > cardiac failure
signs: continuous ‘machinery’ murmur at HS2
mgmt: surgical in childhood
atrioventricular septal defect
septal defect with both atrial and ventricular
component
from failure of endocardial cushions to fuse together
AV canal persists resulting in a single heart chamber,
separated by abnormal valve leaflets
right - to - left shunts
result> blood bypasses lungs to enter systemic
circulation > cyanosis
RT
TO
LT
Tetralogy of Fallot
commonest cause of cyanosis in < 1 yr olds, 1/2000 live
births
tetra : FOUR
i) Ventricular Septal Defect
ii) Over riding aorta (receives blood from rt & lt
ventricles)
iii) pulmonary stenosis (from thickening of subvalvar
muscle or stenosis in valve cusps)
Rt Ventricular Hypertrophy
tetralogy of fallot
AETIOPATHOGENESIS: defects from embryological abnormality in bulbar septum, which
normally separates ascending aorta from pulm. artery, and which fuses with
interventricular septum
pulm stenosis> inadequate perfusion of lungs
overriding aorta> receives blood from BOTH ventricles
net result: > systemic circulation w/ DEOXYGENATED blood >
CYANOSIS
cyanosis: esp. after feeding or crying attack, results in growth stunting, digital
clubbing, polycythaemia
children feel RELIEF from squatting
loud ejection systolic murmur: from VSD or PS
MGMT: surgical closure of septal defect, rechannel blood to aorta from LV
COMPLICATIONS: BACterial endocarditis, cerebral infarct/abcess
transposition of great
arteries
malformation whereby connections between RT & LT ventricle,
aorta, & pulm. artery are DISORDERED
aorta emanates from RV, pulm art from LV
prognosis: possible if there IS ONE OR MORE OF:
ASD
VSD
PDA
mgmt: surgical correction
persistent truncus
arteriosus
EMBRYO: aorta & pulm art develop from same single
tube (TRUNCUS ARTERIOSUS)
persistence: by failure of conotruncal RIDGES to fuse and
descend towards ventricles
so, pulm. artery arises away from origin of undivided
truncus
there is always: defective interventricular septum
undivided truncus overrides both ventricles and receives
blood from both sides.
tricuspid
atresia
rare, absent tricuspid orifice , always associated with:
Patent foramen ovale
VSD
Underdeveloped RV
Hypertrophy of LV
pathophysio: blood shunted from RA to LA, then small
amount shunted from LV to RV via defect
some deoxygenated bloodenters systemic circulation >
cyanosis
mgmt: surgical correction
obstructive congenital
defects
COARCTATION OF AORTA
stenosis of aorta, at or just beyond ductus arteriosus
females 2: males 1, 1/4000 live births
clinical features form stricture of aorta
Hypertension (proximal to stenosis) > headache,
dizzy
Hypotension (distal to stenosis) > weakness, low
circulation
coarctation of aorta
BP raised in upper body, normal or low in legs
large pulsations in upper body, lower body weak
pulses
systolic murmur
untreated:
LV failure from HTN, cerebral hemorrhage, bacterial
endocarditis, dissection of aorta
ATHEROSCLEROSIS
ARTERIOSCLEROSIS: thickening & loss of elasticity of
arteries from ANY condition.
commonest type is AtheroSclerOsis {hardening or loss of
elasticity due to atheroma formation}
involves intima of large - medium sized arteries
other type: Monckebergs medial calcific sclerosis: media
of medium muscular arteries, esp in limbs, lumen size
normal
other type: arteriolar sclerosis: thickening of walls of
small arteries and arterioles
consequences of
arteriosclerosis
vessel thickening: narrow lumen> poor tissue
perfusion
inelasticity of vessels: vessel rupture > haemorrhage
altered endothelium: risk thrombosis* * define
arteriosclerosis leads to MI, angina pectoris, stroke,
TIA, ischaemic colitis, claudication
atherosclerosis
degenerative dz. of large & med arteries
accumulation of lipids in intima (tunica intima) of arteries > cell reactions
commonest : aorta (abd. aorta), coronary arteries, cerebral arteries,
iliac/femoral art
risk factors:
constitutional: genetic traits, race, gender (up to 55 males more), age
hard: hypercholesterolaemia (LDL), Hypertension, Diabetes mellitus,
smoking
soft: lack of exercise, obesity, stress & personality traits
pathogenesis
plaques > low grade chronic endothelial injury from
risk factors
atheroma (atherosclerotic plaques) from:
endothelial injury platelet adhesion to endo.,
diffusion of plasma proteins including LDL into
intima of arteries, migration of monocytes into intima
platelets release PDGF > proliferation of smooth
muscle cells
musc cells deposit excess collagen & elastin in
intima
macrophages phagocytose LDL and release free
useful links
http://www.brown.edu/Courses/Digital_Path/systemic_
path/cardio.html
https://web.duke.edu/pathology/Week13/Week13.html
elevated blood pressure: important and treatable cause
of cardiac failure
hypertension
also a risk factor for atherosclerosis & cerebral
haemorrhage
DEFINITION: sustained rise of systemic BP > 160 mmHg
and / or diastolic > 95 mmHg
borderline hypertension: 140-160 mmHg systolic and/or
90-95 mmHg diastolic
AETIOLOGICAL CLASSIFICATION:
PRIMARY: essential / idiopathic: raised BP with age,
90% cases, raise peripheral vascular resistance
(genetic, socio-economic, dietary, hormonal,
neurological sns)
patho classification htn
BENIGN: stable elevation BP/ years
MALIGNANT: dramatic increase BP / short period
time
benign
vessel changes gradually respond to persistent stable elevated BP
histologically:
hypertrophy & thickening of muscular media
thickening of elastic lamina
fibro elastic thickening of intima
hyaline deposition in arteriole wall (hyaline arteriosclerosis)
effects:
reduced vessel lumen leads to tissue iscahemia
rigidity leads to limited expansion
fragility of vessels leads to haemorrhage
malignant
acute destructive changes in walls of small arteries
when BP SUDDENLY rises
effects:
necrosis of vessel wall (fibrinoid necrosis)
infiltration by fibrin in vessels
leads to lack of blood flow to kidney.
COMPLICATIONS OF HTN
VASCULAR
hyaline deposition in arteries
fibrinous deposition in arteries
HEART
LV Hypertrophy
BRAIN
intracerebral haemorrhage: small vessel , microinfarct, fluid lacunae
KIDNEY
ischaemia of nephrons, chronic renal failure, benign hypertensive nephrosclerosis, renal failure
pulmonary hypertension
pulmonary arterial pressuRe > 30 mmHG
precapillary, capillary, post capillary causes
effects: transudation fluid from pulm capillaries INTO
alveoli > dyspnoea, expectoration of blood stained
watery fluid
chronic effects: hyperplastic arteriosclerosis
(muscular hypertrophy & dilation of pulm arteries),
necrotizing arteriolitis: inc pressure in pulm arteries
haemorrhae in alveolar spaces with haemosiderin
laden macrophages
cor pulmonale: RT ventriular hypertrophy from inc
ischaemic heart disease
condition caused by a reduction / cessation in blood supply to myocardium
~myocardial ischaemia
usually
from atherosclerosis, sometimes from coronary emboli
leading cause of death in western world
results in 4 syndromes
stable angina (chronic)
unstable angina (Acute)
myocardial infacrtion (acute)
sudden cardiac death (acute)
angina pectoris
episodic chest pain, from ischaemia to myocardium
following exercise
usually from stenosis of 1> coronary arteries, red. blood
to myocardium
stenotic coronary arteries are either:
eccentric: fibrolipid plaques affect 1 side of wall,
vasodilataory drugs may help
concentric: colagenous plaques affect whole art wall,
circumferential.
stable angina
predictable , occurs at fixed level of exercise from inc.
heart workload
pain relieved in ~ 2 minutes of rest
stenosis of at least 75% need to reproduce angina on
exercise
unstable angina
unpredictable, not related to exercise
reflects reversible ischaemia due to variable luminal
stenosis
caused by variations in vasomotor tone by plaques or
emboli causing occlusion
prinzimental angina
vasospastic angina
at rest
from increase in coronary vasomotor tone
unknown mechanism
common in early morning
severe but self limiting pain
rarely lead to MI
mgmt angina
avoid risk factors
drug therapy ( nitrates, b blockers)
surgery (coronary angioplasty, bypass)
myocardial infarction
=necrosis of myocardium as a result of severe ischaemia
COMMON, 15%
of all deaths worldwide, 60% sudden
deaths.
middle age, 50 +, but 10 % in 35-50 yr olds
features: chest pain, breathlessness, vomitting, collapse or syncope
types:
regional (90%) infarct in are supplied by ONE major coronary artery
diffuse: (10%) cases, relates to overall myocardial poor perfusion
patho features
macro: site of regional infarct shows circumferential
necrosis from ppor perfusion
histo: NECROSIS & Acute Inflammation
necrotic tissue replaced by collagenous scar
process takes ~ 7 weeks, necrosis causes
enzyme release and proteins which are used as
markers CK-MB, troponin T, lactic
dehydrogenase*
outcomes
of
MI
IMMEDIATELY: sudden cardiac death
Short Term:
arrythmias (if involves conduction tissue)
LV Failure: necrotic wall softens, cardiac dilation
rupture: blood bursts into pericardial cavity
papillary muscle dysfunction: 1 > valve leaflets canot
close in systole
mural thrombus: on the inflamed endocardium over
infarcted area
long term
chronic Left hEART FAILURE: inadequate LV
pumping action
ventricular aneurysm: distension of weakened
fibrotic part of LV
recurrent MI: SECONDARY MI
Dressler’s Syndrome: AutoImmune pericarditis,
raised ESR
part 2 will be sent next
week
happy studying!