* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sonographic Evaluation of the Fetal Central
Survey
Document related concepts
Transcript
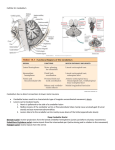
Transventricular Transthalamic Transcerebellar 2 Transventricular Plane • the anterior and posterior portion of the lateral ventricles • the cavum septi pellucidi (CSP): a fluid filled cavity between two thin membranes • late gestation: membranes usually fuse and become the septum pellucidum • CSP becomes visible around 16 weeks and undergoes obliteration near term • Failure to demonstrate the CSP prior to 16 weeks or later than 37 weeks is a normal finding • the posterior portion of the lateral ventricles: a complex formed by the atrium that continues posteriorly into the occipital horn • atrium, characterized by the presence of the glomus of the choroid plexus 3 Transcerebellar Plane • This plane is obtained at a slightly lower level than of the transventricular plane • • • • The frontal horns of the lateral ventricles, CSP, thalami, cerebellum and cisterna magna • the cerebellar hemispheres, more echogenic cerebellar vermis in the middle • cisterna magna: a fluid filled space posterior to the cerebellum • in the second half of gestation the depth of the cisterna magna is stable: 2–10 mm • vermis has not completely covered the 4th ventricle prior to 20 weeks’ gestation. false 4 impression of a defect of the vermis in early gestation Transthalamic Plane The anatomic landmarks: • the frontal horns of the lateral ventricles, • the cavum septi pellucidi, • the thalami and the hippocampal gyruses. • does not add significant anatomic information • easier to identify and in late gestation: more reproducible measurements 5 6 Transfrontal plane • midline interhemispheric fissure (IHF), • the anterior horns of the lateral ventricles, • sphenoidal bone, occular orbits, • rostral part of the genu of the corpus callosum - IHF association Superior sagittal sinus (1), interhemispheric fissure (3), frontal horns of the lateral ventricles (4), genu (5) of the corpus callosum Orbits (O) Coronal views of the fetal head Transarcuadate plane • CC genu/ anterior part – IHF association , • Cavum Septi Pellucidi(CVP), • the lateral ventricles parietal bones and anterior fontanel (2), frontal horns of the lateral ventricles (4), body (6) of the corpus callosum, cavum septi pellucidi (7), caudate nucleus (8) Orbits (O) 7 Transthalamic plane • Thalamus, • III. Ventricule, • Atrium of lateral ventricule frontal horns of the lateral ventricles (4), body (6) of the corpus callosum, cavum septi pellucidi (7), hippocampus (9), cerebellar vermis (10), Sylvian fissure (SF), Coronal views of the fetal head Transcerebellar plane • Occipital horns of lateral ventricules, • Interhemispheric fissur, • Cerebellar hemispheres, • Vermis cerebellar vermis (10), Occipital horns (OH), cerebellar hemispheres (C), cisterna magna (CM) 8 Midsagittal plane Fetal Head Sagittal plane Corpus callosum, Cavum septi pellicidi, Brain stem, pons, vermis, Posterior fossa, Anterior cerebral artery (with Doppler) Pericallosal artery (with Doppler), Vein of Galen (with Doppler) Parasagittal plane The entire lateral ventricle, The choroid plexus, The periventricular tissue, Cortex 9 Acrania • Absent calvarium above orbits • Exposed brain with no cranium • Affects membranous flat bones ( frontal, parietal, temporal and occipital ) • Skull base intact 10 Anencephaly • No calvarium with absence of neural tissue above orbits • Protuberant eyes • Always fatal, and termination of pregnancy should be offered • A part of the cerebral hemispheres sometimes visible in the 1st trimester “exencephaly” 11 Cephalocele • Cranial defects, along bony sutures, in which there is a herniation of the brain or the meninges, or both. • Occipital, parietal, or frontal, most common: occipital • If the cephalocele sac contains brain tissue: encephalocele • If only cerebrospinal fluid (CSF) is present: meningocele. • Incidence: 1 in 3500 to 1 in 5000 live births • Usually isolated, but in a small percentage: a part of a chromosomal or nonchromosomal syndrome. • Hydrocephaly in 80% of occipital encephaloceles, microcephaly (20%) • Approximately 65% of fetuses have at least one major malformation and 35% have 12 isolated cephalocele Cephalocele • Autosomal recessive syndromes that feature a cephalocele : • Meckel (cephalocele, renal cystic dysplasia, and postaxial polydactyly); • Walker-Warburg or HARD ± E (hydrocephaly, agyria, retinal dysplasia, with or without encephalocele); • Knobloch (vitreoretinal degeneration and occipital encephalocele) • Detailed anatomic survey, fetal echocardiography • Genetic counseling, CVS, and/or AS; microarray if chromosomes are normal • Prognosis: High mortality rate 13 Choroid plexus cysts • Well-demarcated, anechoic, fluid-filled structures within the choroid plexus of the lateral ventricles of the brain • Unilateral or bilateral • Usually small , <10 mm in diameter • They regress, spontaneously during the third trimester. • Isolated finding + maternal serum: low risk… AS unlikely to find any abnormality • Associated anomalies are those seen with trisomy 18 • congenital heart disease, clenched hands, single umbilical artery, intrauterine growth restriction, and rocker bottom feet. • if associated with other findings (e.g., VSD, clenched hands) or the maternal serum screen shows increased risk, offer genetic counseling and amniocentesis. 14 Arachnoid cysts • Collections of cerebrospinal fluid on the brain surface • Usually benign, congenital, space-occupying lesions • Mostly sporadic • Commonest over cerebral convexities • One third in the posterior fossa • Remaining brain sonographically normal in majority • Avascular lesion: color Doppler reveals no blood flow in the walls • congenital (primary) or secondary (acquired) (inflammation, hemorrhage, or trauma) • Ventriculomegaly or hydrocephaly—secondarily to pressure • Anatomic survey, fetal echocardiography, genetic counseling andkaryotype 15 Holoprosencephaly • failure of the forebrain to properly divide along the midline • partial or complete failure of division of the prosencephalon into two separate hemispheres between the 18th and 28th day after conception • three “classic forms” arealobar, semilobar, and lobar 16 Alobar Holoprosencephaly • complete lack of division of the forebrain with absent midline structures • fusion of the thalami and cerebral hemispheres • a single primitive ventricle (monoventricle ) • the interhemispheric fissure, falx cerebri, 3rd ventricle and corpus callosum are totally absent • associated with a spectrum of facial abnormalities : • cyclopia (single midline eye), arrhinia (absent nose), synophthalmia, or microphthalmia, severe hypotelorism, midline cleft lip and palate, flat nasal bridge, and single or barely separated nostrils 17 Alobar Holoprosencephaly • isolated HPE often normal karyotype • 25%-45% of newborns with HPE have a karyotype abnormality (trisomy 13, trisomy 18, triploidies) • karyotype all fetuses, • termination offered 18 Semilobar Holoprosencephaly “Partial cleavage of prosencephalon at posterior” • absence of the interhemispheric separation • but posteriorly there is some separation • the anterior horns are fused • the septi pellucidi and the anterior part of the corpus callosum are absent • partial separation of the thalami • a rudimentary third ventricle and facial anomalies • the two cerebral hemispheres are partially separated posteriorly but there is still a single ventricular cavity • degree of developmental disability typically correlates with the severity of the brain malformation • karyotype all fetuses, termination offered Single ventricule Some cleavage of thalami Occipital horns Single ventricule 19 Lobar Holoprosencephaly “lack of separation of the ventral neocortex and agenesis of the corpus callosum” Frontal lobes fused • frontal lobes fused • absence of the septum pellucidum • the interhemispheric fissure is well developed posteriorly and anteriorly • a variable degree of fusion of the cingulate gyrus and of the lateral ventricles • No diagnosis before 18th weeks gestation, as CSP is not visible properly occipital lobes 20 21 Schizencephaly • Gray matter lined cleft extending from brain surface to ventricle • CSP absent in 70% • defect of brain parenchyma extending from inner table of skull to underlying ventricle • probably a neuronal migration disorder • prognosis is poor, and termination of pregnancy should be offered 22 Corpus Callosum Agenesis • Largest midline commissure of the brain connecting the neocortex of the cerebral hemispheres • CC sonographically visible at 18-20 wks • CC forms in midline lamina between 8-20 wks • Develops from anterior to posterior • CC agenesis: partial/ complete … • In partial agenesis, the anterior parts are developed, but the posterior aspects are absent. • Colpocephaly • Absent cavum septi pellucidi • Absent corpus callosum • Absent or abnormal pericallosal artery • Teardrop-shaped, parallel lateral ventricles on the axial section 23 Corpus Callosum Agenesis • Karyotype recommended even if isolated finding • CNS anomalies in up to 85% of cases, non-CNS anomalies in up to 65% of cases • worse prognosis in the presence of additional anomalies. • in cases of isolated ACC, it appears to carry a better prognosis n( eurodevelopmental delay in about 25% of cases at 3 years). • in 10%-17%, ACC is an isolated finding, and these individuals are asymptomatic. • individuals with ACC and other CNS anomalies are more likely to have neurologic symptoms. • neuromotor skills are impaired in almost all individuals with ACC (severe spastic or spastic-dystonia, hypotonia). 24 Dandy-Walker Malformation • marked cystic dilatation of the fourth ventricle, which may fill much of the posterior fossa • hypogenesis or agenesis of the cerebellar vermis • superior displacement of the tentorium 25 Dandy-Walker Malformation • enlargement of the posterior fossa • 70% to 80% of the cases, some degree of ventriculomegaly or hydrocephaly is present, with progressive postnatal ventriculomegaly • large cistern magna that communicates with the fourth ventricle • cerebellar hemispheres splayed apart with varying degrees of dysplasia • elevated tentorium • absent or hypoplastic vermis • cephalad rotation of the vermian remnant • cannot make the diagnosis in the early 2nd trimester, normal development can resemble disease, must repeat US later than 18 wks. • development of vermis: 16-20 wks • vermian disgenesis: dx at 20-22 wks 26 Dandy-Walker Malformation • frequency of associated malformations: 50% to 70%. • CNS anomalies most common: hydrocephaly, CCA or disgenesis, holoprosencephaly, cephaloceles • congenital heart disease, craniofacial, renal, limbs, abdominal wall, diaphragmatic hernia, and ambiguous genitalia. • IUGR • Chromosomal anomalies such as trisomy 9, 21, 18, and 13;triploidy; 6p and 3q22q24 deletion • nonchromosomal syndromes such as Meckel, Walker-Warburg, and Cornelia de Lange 27 DWM management_prognosis Anatomic survey Fetal neuroscan Fetal echocardiography Genetic counseling, karyotype, test for 3q24 deletion, microarray studies • Consider MRI to rule out associated anomalies • Offer termination of pregnancy • Serial scans to monitor ventriculomegaly • • • • • Motor deficits; delayed motor development, hypotonia, and ataxia; about half have mental retardation • IU fetal demise in about 14% • 80% develop hydrocephaly by 3 months • Overall infant mortality:10%-66% • infection, uncontrolled hydrocephaly, and shunt complications • One third of survivors with DWM can develop normally Favorable neurodevelopmental outcome: no associated CNS or extra-CNS anomalies and a normal lobulated vermis 28 Vein of Galen aneurysm • The vein of Galen is located under the cerebral hemispheres; it drains the anterior and central regions of the brain into the sinuses of the posterior cerebral fossa. • Aneurysmal malformation with an AV shunting of blood. • High-output heart failure (decreased resistance and high blood flow) • Cardiomegaly in 64%, enlarged neck vessels in 32% • Ventriculomegaly in 24% • Hydrops in severe cases, • Mass effects, causing progressive neurologic impairment • Cerebral ischemic changes • The cardiac and brain status dictates the long-term outcome. 2D and/or 3D color or power Doppler imaging: • Postnatal: endovascular treatment high-velocity turbulent flow 29 “Calipers positioned at the level of the glomus of the choroid plexus, touching the inner edge of the ventricle wall at its widest part and aligned perpendicular to the long axis of the ventricle” Ventriculomegaly • Mid-trimester average 7 mm ± 2mm • Ventriculomegaly > 10 mm • 10-12= mild ventriculomegaly • 12.1-14.9 = moderate ventriculomegaly • > 15 mm = Hydrocephaly 30 Pilu G, Hobbins JC. Prenat Diagn 2002;22:321-30. Ventriculomegaly VM is 1 : 1000 to 2 : 1000 births <12mm VM: 62% regresses at 24.wks Associated structural and/or chromosomal malformation in about 41% chromosomal aneuploidy 11%; Trisomy 21 was most common , followed by trisomies 18 and 13 • Structural anomalies (with normal karyotype); 43% • • • • – brain anomalies, most common: Chiari II, CCA, microcephaly – heart, diaphragmatic hernia, omphalocele, and limb reduction – cong. inf.; 0.8% (cytomegalovirus, toxoplasmosis) 31 Ventriculomegaly • • • • Anatomic survey Fetal neuroscan; additional anomalies. Fetal echocardiography Genetic counseling and amniocentesis; – esp. if the mild VM is not an isolated finding or – if maternal aneuploidy screening suggests risk • MRI of the brain; additional anomalies • Send amniotic fluid for Toxo, CMV PCR • Serial ultrasound to monitor the progression of the VM In cases of mild VM : associated anomalies influence the prognosis In utero progression of VM= ↑ neurologic sequelae 32 Mega cisterna magna Cisterna Magna>10 mm From cerebellar vermis posterior to the inner edge of occipital bone • • • • • • • Enlarged posterior fossa cerebral spinal fluid (CSF) space Fourth ventricle is normal Cerebellar hemispheres normally formed Cerebellar vermis is complete and normal Usually an incidental finding Part of multiple findings seen with trisomy 18 If isolated likely has no adverse clinical outcome 33 • Cisterna Magna > 10 mm • Intact vermis without rotation • Mega cisterna magna, normal outcome >90% cases 34 • Normal cisterna magna, hourglass shape of 4th ventricle opening • Intact vermis rotated <45° • Usually Blake’s pouch cyst, normal outcome >90% of cases 35 • Large V-shaped cisterna magna • Normal/small vermis rotated >45° rotate • Usually Dandy-Walker malformation, abnormal outcome 50% of cases 36 Thank you 37








































![[11c]altropane, a highly selective ligand for the dopamine](http://s1.studyres.com/store/data/002796836_1-4fb096535d1fa152c20097ed5b47d133-150x150.png)