* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Assessment guide
Saturated fat and cardiovascular disease wikipedia , lookup
Food studies wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Obesity and the environment wikipedia , lookup
Food politics wikipedia , lookup
Malnutrition in South Africa wikipedia , lookup
Malnutrition wikipedia , lookup
Overeaters Anonymous wikipedia , lookup
Gastric bypass surgery wikipedia , lookup
Childhood obesity in Australia wikipedia , lookup
Human nutrition wikipedia , lookup
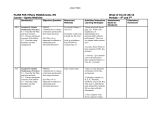
MOUNT CARMEL COLLEGE OF NURSING Assessment Guide: Nutritional Status Assessment I. Appearance Age Long-standing eating habits may be a factor in the appearance of a patient who looks older/younger than his chronological years. Sex Height, weight and sex are used to evaluate condition of normal, over or weight. Weight status is an indication of nutritional status. Overweight is a contributing factor to most illness, e.g. diabetes, heart diseases. Look at high fat intake; total calories; exercise patterns. Suggested weight chart is based on the BMI. Waist measure is another tool to use for weight assessment. Risk is associated with waist measurement greater than 35 inches for women; 40 for men. Height Weight (Compare to weight chart) Body Mass Index Skin-tugor, coloring Eyes and Hair General alertness/level of consciousness II. Significance General appearance, including skin coloring, skin tugor, eyes and hair may be indicators of nutrition and/or hydration status. General alertness – level of consciousness will determine extent of teaching possible or need for special feeding help. Nutritional Adequacy of Food Intake At home – nutrition history Evaluation of the patient’s nutrition history It is the best way to determine usual eating habits which contribute to present nutritional status. In hospital observation of meal intake Types and amount of foods actually eaten in the hospital may be indicators of nutritional status. Food Allergies/Intolerance Food allergies may contribute to present nutritional status and must be considered in teaching, feeding the patient. Previous diet restrictions Previous diet restrictions and the extent of knowledge about the diet must be assessed in order to plan appropriate teaching. -2Alcohol intake III. Alcohol intake contributes empty calories in the diet and may interfere with adequate nutritional intake and the metabolism of certain nutrients. Sociological and Physical Factors Affecting Food Intake Social and emotional Degree of socialization influences eating pattern. Loneliness decreases appetite and general interest in eating. Explore with patient possible ways to increase degree of socialization – e.g., Congregate Meal Program; friends, family. Emotional status influences food choices and quantity eaten. May increase or decrease quantity eaten. Must be resolved before diet restrictions can be followed. Eating-related behavior may be of importance, especially in working with the overweight, e.g. eating when angry, eating when lonely, sampling when cooking. Job related Job related factors such as type of work, hours of work, availability of foods (cafeteria or vending machine) influences food eaten. Ethnic and religious Ethnic and religious and cultural preferences or restrictions influence foods eaten. Economic Economics plays an important role in food choices especially with those on low income. Food Stamps can increase amount of money for food and should be suggested to those likely to qualify. Storage and cooking facilities influence food choices. Physical handicaps Limitation in available transportation and physical handicaps including degree of ambulation affect shopping habits and preparation of food as well as eating habits. Investigation of help available for these purposes should be pursued. Possibility of “Meals on Wheels.” -3Pain Shortness of breath Condition of mouth teeth-dentures IV. Pain will decrease appetite and shortness of breath will interfere with preparation of foods as well as eating. Consider the use of pain medication and rest periods prior to eating. Missing teeth or dentures should be considered. Not having teeth does not necessarily limit selection of foods. Some people “gum” very well. tongue, mucous membrane Presence of lesions in the mouth, dry mucous membranes, swollen, infected gums and coated tongue all decrease appetite for foods. Swallowing ability Swallowing ability must be considered in choices of foods and their consistency. Thickeners may be needed. Swallowing Evaluation by Speech Therapy may be needed Constipation Constipation problems influence food choices and eating habits. Explore with patient ways of increasing fiber and fluid intake. Diarrhea Diarrhea means that nutrients are being lost. Cause needs to be identified. Fluid replacement is especially important. Fiber can be a factor here too. Yogurt with active cultures may be helpful. Digestion Presence of conditions which impair digestive ability Loss of important G.I. secretions (HCL – enzymes) will interfere with degree of digestion. Loss of part of the G.I. tract (gastrectomy, ileostomy) will influence completeness of digestion and absorption. Consider which nutrients are most affected in specific situations. Medications which interfere with digestion. Many medications have G.I. disturbing side effects. -4Anorexia, nausea and vomiting Presence of anorexia, nausea and vomiting will limit availability of foods for digestion. Foods must be digested in order for nutrients to be absorbed. V. Absorption Presence of conditions which impair absorption Loss of part of the absorptive surface of the G.I. tract will limit absorption – (Crohn’s disease, short-bowel syndrome). Increased speed of passage of contents of G.I. tract will decrease absorption (ileostomy, diarrhea). Medications which interfere with absorption Some medications interfere with absorption and others destroy normal intestinal flora which aid in digestion and absorption. Nutrients must be fully absorbed in order to to available for body utilization. VI. Factors Which Alter Nutrient Needs Increase of metabolism Increase in need for calories and other nutrients is present in stress, fever, infections, wound healing, cancer, burns, etc. State of hydration Replacement of losses in fluids and nutrients must be considered in situations such as prolonged diarrhea, burns, hemorrhage, extensive drainage, malnutrition. Medications affecting nutrient needs Many medications have nutrient interactions and influence nutrient metabolism. Altered metabolism Some conditions, such as diabetes, thyroid and parathyroid problems alter normal metabolism of nutrients. Age Consider the difference in needs for the infant, child, teen and for pregnancy and lactation. -5VII. Lab Values Pertinent to Nutrition Hgb Low hemoglobin indicates a need for ironrich foods, along with protein. Note factors that favor/hinder iron absorption. Serum albumin, pre-albumin total iron-binding capacity, transferrin, creatinine Low serum albumin, pre-albumin and T.I.B.C. or transferrin may indicate poor protein status as a result of malnutrition. High creatinine levels indicate body protein being broken down – negative nitrogen balance. Cholesterol, HDL/LDL ration Cholesterol and HDL/LDL ratio are indicators of lipid status and the possible need for diet altered in total fat, saturated fatty acids, and cholesterol. Fasting Blood Sugar (FBS) Blood glucose levels High glucose and Fasting Blood Glucose may indicate altered carbohydrate metabolism, possible diabetes or pre-diabetes. Hg A1c Hemoglobin A1c indicates degree of blood sugar control over time. Total Lymphocytes Must be calculated from total W.B.C., using the percent of lymphocytes indicated on the Differential Test or use Lymph Absolute on lab sheet. Low levels may indicate poor immune status – an indicator of malnutrition. K and Na Low potassium levels may relate to general poor nutrient status, or excessive losses since K is found in most foods. High sodium levels may indicate need for sodium restriction. NOTE: No one lab value indicates malnutrition. Several low or marginal values are used as indicators of poor nutritional status. Blood calcium levels are maintained at the expense of the bone – therefore calcium is not an indicator of nutritional status. -6VII. Medications Affecting Nutritional Status Diuretics Diuretics (depending on type) cause increased retention or loss of sodium or potassium. Dietary need for these minerals may be affected. Iron Medications Iron medications may cause constipation and/or GI upset. Better tolerated in combination with vitamins. Multivitamins Multivitamins may be used to supplement diet. Therapeutic preparations should taken only on doctor’s order. Does the preparation taken by the patient actually contain the nutrients you have found to be low in the patient’s dietary intake? Caution patient about danger of high levels of vitamins and minerals taken as supplements. Herbal Products Concern about these products. No requirement that they are safe or effective!! “Natural” does not always mean better or safe! Others There are many drug-nutrient interactions. Most medications have some effect on the G. I. tract. Note this when looking up drugs that your patient is receiving. IX. Additional Source of Nutrients Standard IV’s If patient is receiving I.V. – what nutrients are provided? How many calories per day? How does this compare with his actual needs? Total Parenteral Nutrition Amino Acids with Dextrose Fatty Acids If patient receiving T.P.N. – what is the order? What nutrients are provided? How many calories per day? How does this compare to actual needs? Tube feeding If patient receiving tube feeding – which one? How does the amount being given the patient in 24 hours compare to actual calorie needs (and to amount needed for 100% RDI/RDA according to label on can)? What is the osmolality of feeding? Does the patient tolerate the tube feeding? -7- Nutritional supplements X. If patient receiving nutritional supplements, Which? Does it provide the nutrients the patient is not receiving in his usual intake? Does it take away appetite for the usual meals? Other Pertinent Information: Based on Learned Concepts Family history of diabetes Is there a family history of diabetes which would be important to note in an individual who is already obese and perhaps has a high FBS? If patient has diabetes, he/she needs to be on a diabetic diet. Patient needs to be referred to a diabetes educator and/or registered dietitian. Family history of heart disease Is there a family history of heart disease which would be important to note in situation where patient is obese and has high serum cholesterol and high fat intake? Refer to a registered dietitian for help. Osteoporosis Is the patient aware of the importance of calcium intake and exercise on the development of osteoporosis? Cancer Note weight status; appetite. Encourage patient to eat as part of his/her treatment, regardless of appetite. Hypertension Refer to dietitian. Consider the effect of obesity, sodium, possibly calcium and potassium on blood pressure. Rev: 12/10