* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Mirobiology 14-15
Neonatal infection wikipedia , lookup
Infection control wikipedia , lookup
Viral phylodynamics wikipedia , lookup
Human microbiota wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Microorganism wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Plant virus wikipedia , lookup
Anaerobic infection wikipedia , lookup
Ebola virus disease wikipedia , lookup
Introduction to viruses wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis C wikipedia , lookup
Social history of viruses wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Marburg virus disease wikipedia , lookup
Marine microorganism wikipedia , lookup
West Nile fever wikipedia , lookup
Hepatitis B wikipedia , lookup
Canine parvovirus wikipedia , lookup
Henipavirus wikipedia , lookup
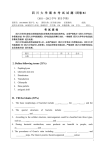
MICROBIOLOGY PROGRAM – MEDICAL FACULTY, SUMMER SEMESTER 2014/2015 1. The basics of the microorganisms differentiation - morphology. Morphology of bacteria and fungi: dimensions, shape, structure of bacterial cell, differences in cell wall structure (Gram- positive and negative bacteria, mycobacteria, other). Key features differentiating bacteria and fungi. General taxonomy of microorganisms: kingdom, phyllum, class, order, family, genus, species (strain, biotype, serotype, serovar). Direct detection of microorganisms: microscopic investigations, demonstrating of antigen directly in the specimen by serological methods or genetic material by molecular biology methods. Methods of microbial morphology examination - microscopic investigations: observation of microorganisms in the living state, stained preparations, the use of different types of microscopes in microbiology. Staining methods: types, practical application (the method of Gram, Ziehl-Neelsen, Neisser, Giemsa, Löffler).Scheme of microbiological examination. The major groups of Gram-positive bacteria – cocci: Staphylococcus, Streptococcus, Enterococcus, Peptostreptococcus; bacilli: Bacillus, Clostridium, Corynebacterium, Listeria, Propionibacterium, Lactobacillus, Actinomyces, Nocardia, Mycobacterium. The major groups of Gram-negative bacteria - cocci: Neisseria, Veilonella; rods: Enterobacteriaceae (Escherichia coli, Klebsiella, Salmonella, etc.), nonfermentative rods: Pseudomonas, Acinetobacter, other bacilli: Vibrio, Campylobacter, Helicobacter, Haemophilus, Bordetella, Gardnerella, Legionella, etc.; anaerobes: Bacteroides, Fusobacterium; the spirochetes: Treponema, Borrelia, etc.; Rickettsia, Chlamydia, Mycoplasma. General features of viruses - size and structure, properties and participation of individual structural elements of viruses in the pathomechanism of infection, in diagnostics, vaccines production. Stages of virus propagation, the influence of type of replication on the viral infection course. Bacteriophages. Prions. Basic virus taxa: dsDNA: Herpesviridae (Human herpesvirus - HHV-1, HHV-2, HHV-3 (VZV), HHV-4 (EBV), HHV-5 (CMV), HHV-6, HHV-7, HHV-8; Adenoviridae (Human adenovirus -HAdV-A, -B, -C, -D, -E, -F); Polyomaviridae (BK polyomavirus - BKPyV, JCPyV); Papillomaviridae (Human papillomavirus - HPV); Poxviridae: (Vaccinia virus - VACV, Variola Variola virus (VARV), Molluscum contagiosum virus (MCV). ssDNA: Parvoviridae (B19 virus - B19V) Reverse transcribing viruses: Hepadnaviridae (Hepatitis B virus HBV); Retroviridae (Human immunodificiency virus - HIV-1, HIV-2, Primate T-lymphotropic virus - PTLV-1, PTLV-2 (HTLV) dsRNA: Reoviridae (Rotavirus A – RV-A, Rotavirus B – RV-B, Colorado thick fever virus- (CTFV) ssRNA(-): Orthomyxoviridae (Influenza A- FLUAV, Influenza B - FLUBV, Influenza C - FLUCV); Paramyxoviridae (Human parainfluenza virus - HPIV-1, HPIV-3, Measles virus – MEV, Mumps virus – MuV, Human respiratory syncytial virus – HRSV); Rabdoviridae (Vesicular stomatitis New Jersey virus – VSNJV, Rabies virus – RABV); Bornaviridae (Borna disease virus – BDV); Filoviridae (Za Seoul virus – SEO; Zaire Ebola Virus, Marburg virus); Bunyaviridae (Hantaan virus – HTNV, Dobrava-Belgrad virus – DOBV, Puumala virus – PUUV, Sin Nombre virus – SNV, Rift Valley fever virus – RVFV); Arenaviridae (Lassa virus - LASV, Junin virus – JUNV, Machupo virus – MACV, Guanarito virus – GTOV, Sabia virus – SABV), Hepatitis delta virus - HDV; Picornaviridae (enterowiruses: Coxackie, Echo Polio; rinowirusy: Human rhinovirus - HRV-A, HRV-B; Hepatitis A virus – HAV, Foot-and-mouth disease virus – FMD); Calciviridae (Norovirus – (Norwalk virus) - NV, Sapporo virus – SV); Astroviridae Human astrovirus – HastV); ssRNA(+): Coronaviridae (Coronavirus, SARS, Torovirus); Togaviridae (Rubella virus - RUBV); Flaviviridae (Tick-borne encephalitis virus –TBEV, Yellow fever virus - YFV, Dengue virus - DENV, West Nile virus-WNV, Hepatitis C virus – HCV); Hepeviridae: Hepatitis E virus – HEV. Practice: Discussion of safety rules in the laboratory microbiological. Hand washing. Preparing and observation a wet mount - hanging drop. Preparing and observation smears made from solid and liquid bacterial cultures - Gram, Löffler and Neisser staining methods. Oil immersion microscopy. Microscopic examination of prepared slides: an assessment of the size and morphology of microorganisms, the differentiation of the various groups of microorganisms. Observation of bacterial motility on solid agar medium, semi-solid agar motility assay. 2. The basics of the differentiation of bacteria and fungi. Part II Microbial physiology - nutritional requirements, carbon and energy sources (autotrophs, heterotrophs, chemolithotrophes, chemoorganotrophs), metabolism - a sources of carbon and energy (autotrophs, heterotrophs, chemolitotrophs, chemoorganotrophs), atmosphere (obligate aerobes, facultative and obligate anaerobes, microaerophils, capnophiles), the influence of temperature, pH, pressure, redox potential on the growth of bacteria. Differences in growth requirements of different groups of microorganisms. The growth and multiplication of bacteria and fungi - development cycles, bacterial growth phases, growth rate on artificial media (typical bacteria, mycobacteria, anaerobes, fungi, yeast, molds, dermatophytes). Variability of bacteria – genotype, phenotype, mutation, recombination (conjugation, transduction, transformation). Biological and medical importance of genotype changes: morphologic and biochemical features, pathogenicity, antibiotic susceptibility. Media for cultivation of microorganisms – classification of bacteriological media (liquid, solid, semisolid, nutrient, simple, enriched, selective, differential, transport media, chromogenic), application of various media in the microbiological diagnostics. Differentiation of microorganisms based on the growth type in liquid media (turbidity) and solid media (colony morphology). The usage of metabolic features (enzyme activity, biochemical characteristics) for the identification and differentiation of microorganisms. Methods of bacteria and fungi identification/ diagnostic kits: API tests, ATB system, Vitek Compact, Maldi-Tof, other. Bacterial identification: colony and microscopic morphology, biochemical tests. Methods of cultivation of viruses (tissue cultures, chick embryos, sensitive laboratory animals). 1 Methods of detection of virus-infected cells: cytopathic effect, plaque assay, hemagglutination, hemadsorption, neutralization test, microscopic, molecular methods. Detection of antigens and genetic material of viruses. Practice: Observation of bacteriologic media before and after an inoculation: liquid media (tryptic soy broth, thioglycollate), solid media (sheep blood agar, MacConkey agar, Sabouraud agar, chocolate agar, Chapman agar, D-Coccosel, Pyacyanosel, chromogenioc media). Bacterial and fungal growth evaluation, colonies morphological (appearance) and "biochemical" (color) characteristics. Demonstration of equipment for the cultivation of anaerobic bacteria (anaerostat) and requiring increased atmospheric carbon dioxide and / or a reduced (5-10%) partial pressure of oxygen (candle jar). Differentiation of bacteria and fungi on the basis of biochemical characteristics - API tests (visual reading), VITEK 2 Compact cards. A visit to the media preparation room and bacteriology lab – glassware and media preparing. Application of media in a routine diagnostics, visual and automatic reading of biochemical features of bacterial strain. Demonstration of specimen collection kits (swabs, transport media, growth media used for transport, etc.). Preparing a specimen swab culture by an individual student (throat, nasal, anal, vaginal, other specimens). 3. Normal human flora (microbiota). Fundamentals of infections detection. The major groups of Gram-positive bacteria. Forms of relationships between microorganisms. Relationships between microorganisms and host. Normal human microbiota and its importance. Pathogenicity (virulence) of microorganisms – infectivity, invasiveness, toxigenicity. Microbial virulence factors: superficial structures (fimbriae, capsules, mucoid substances, adhesive proteins), toxins (exo-, endo-, entero-, neurotoxins, mode of action), enzymes (e.g. coagulase, hyaluronidase, other). Some epidemiological terms connected with infection and the infective diseases epidemiology: adhesion, colonisation, contamination, invasion, evasion, infection (acute, chronic, opportunistic, local, systemic, generalized, asymptomatic, symptomatic, latent, mixed, primary, reinfection, superinfection, nosocomial community-acquired, endo- and exogenous, congenital), anthroponosis, anthropozoonosis, zoonosis, sapronosis, bacteraemia, sepsis, intoxication, contagion, reservoir, entry, source and routes of infection, incubation period, prevalence, outbreak, endemia, pandemia, morbidity and morbidity rate, mortality and mortality rate, fatality, measurements, surveillance. The purpose and importance of bacteriological examination. The rules (procedures) of collection the material for microbiological examination (bacteriological, virological, mycological): the period of collection, types of materials, methods of collection, storage and transportation, request form to microbiological laboratory; pre-analytical and analytical errors. Specimen processing in the bacteriological laboratory - implementation and practical significance of the various stages: • direct examination: microscopic (wet mount, direct smears stained with Gram or other methods, demonstration of antigen or genetic material of microorganism directly in a test sample by serological or molecular biology methods; • inoculation of appropriate bacteriological media, culture under aerobic / anaerobic / other condition; • identification of isolated microorganisms - morphological characteristics (smears from culture, colony morphology), biochemical profile, antigenic characteristics (determination of the serotype/ serovar), other (eg, phage typing, genotyping); • antimicrobial susceptibility testing, detection of resistance mechanisms (phenotypic and genetic methods); • the study of microorganism virulence ( in vivo and in vitro methods); • clinical interpretation of the result of bacteriological examination - normal microbiota, carrier-state, colonization, etiological agent; errors in the interpretation of results (post-analytical error); Indirect diagnostics - determination of serum antibody titer with serological reactions. The major groups of Gram-positive bacteria - occurrence, pathogenicity, the most common clinical presentations of infection, defense mechanisms - the type of inflammatory reaction, microbiological diagnostics. Facultative anaerobic(aerobic) cocci: catalase-positive: Staphylococcus (S. aureus, grupa CNS: S. epidermidis, S. saprophyticus), Micrococcus; catalase-negative: Streptococcus (serological groups: A – S. pyogenes, B – S. agalactiae, C – S. equisimilis, G – different strains), S. pneumoniae,’viridans group’, Enterococcus; Obligate anaerobic cocci: Peptococcus, Peptostreptococcus, Anaerococcus, Peptoniphilus, Finegoldia . Aerobic rods: spore-forming: Bacillus (B. anthracis, B. cereus). nonsporeforming rods: Corynebacterium (C. diphtheriae), Mycobacterium (M. tuberculosis, MOTT), Listeria, Erysipelothrix; weakly acid-fast, branching rods: Nocardia, Streptomyces, Rhodoccocus, Actinomadura. Anaerobic Gram-positive rods: spore-forming bacilli: Clostridium (C. tetani, C. perfringens, C. botulinum). nonsporeforming rods: Actinomyces, Propionibacterium, Eubacterium, Lactobacillus, Bifidobacterium, Mobiluncus. Practice: Differentiation of staphylococci: staphylococcal colony morphology onto ordinary agar, sheep blood and Chapman media, performance of tests for catalase, clumping factor and latex Staphaurex-type, the readout of coagulase tube test, diagnostic sets for biochemical identification (API and ID 32 Staph, VITEK GP). 2 Differentiation of streptococci and: assessment of bacterial colony morphology and hemolysis type on sheep blood agar (α, β, γhemolysis), chromogenic media (e. g. Granada agar – S agalactiae), serological grouping of β-hemolytic streptococci (Streptokit) ASO (ASLO) test, sensitivity to optochin (differentiation of pneumococci from viridans streptococci). Differentiation of enterococci: evaluation of growth characteristics on simple agar, sheep blood, selective-differentiating media (bile esculin and potassium tellurite agars). Comparison of Gram and Neisser smears from cultures of C. diphtheriae and diphtheroids. Observation of coryneform bacteria culture on blood agar, Propionibacterium spp. onto Schaedler medium. Nocardiae: watching the preparations stained with Gram method and culture on ordinary agar (microcolony). Analysis of self-made cultures with from different parts of the body. Diagnostics of mycobacteria: microscopic examination of direct sputum smears for M. tuberculosis (Ziehl-Neelsen and fluorescent methods) and the mycobacterial cultures Lövensteina-Jensen medium, detecting the presence of M. tuberculosis DNA by RealTime PCR. Diagnostics of spore-forming bacilli: examination of a direct smear of wound secretions in case of gas gangrene, watching cultures of Bacillus cereus and Clostridium perfringens. 4. Basic groups of Gram-negative bacteria. Gram-negative bacteria - occurrence, pathogenicity factors, the commonest clinical manifestations, the host defence mechanisms – type of inflammatory response, epidemiology, microbiological diagnostics Facultatively anaerobic(aerobic) cocci: Neisseria, Moraxella Obligately anaerobic cocci: Veilonella. Fermentative Gram-negativ, facultatively anaerobic enteric rods (Enterobacteriaceae): Escherichia coli (EPEC,ETEC,EIEC, EHEC), Salmonella (serotypes: S Typhi [D] – typhoid fever, S Paratyphi [A, B, C] S. Enteritidis, S. Agona, S. Typhimurium, S. Heidelberg...), Shigella (S. dysenteriae, S. flexneri, S. boydii. S. sonnei), Klebsiella (K. pneumoniae, K oxytoca, K rhinoscleromatis, K ozenae), Enterobacter, Citrobacter, Serratia, Proteus, Morganella, Providencia, Yersinia. Non-fermentative, non-fastidious Gram-negative aerobic rods: Pseudomonas aeruginosa, Stenotrophomonas maltophilia, Burkholderia cepacia, Acinetobacter baumannii, Alcaligenes, Flavobacterium. Oxidase-positive, microaerophilic rods Campylobacter jejuni, Helicobacter pylori. Oxidase-positive, fermentative facultatively anaerobic rods: Vibrio (V. cholerae, V. parahaemolyticus), Aeromonas. Fastidious small rods (coccobacilli): Francisella tularensis, Pasteurella multocida, Brucella spp., Bordetella pertussis, Haemophilus influenzae, Legionella pneumophila. Gram-negative obligate anaerobic rods: Bacteroides, Porphyromonas, Prevotella, Fusobacterium, Leptotrichia, Aggregatibacter actinomycetemcomitans. Practice: Differentiation of Neisseria and Moraxella spp.: oxidase test, biochemical tests (API, VITEK NH). Neisseria meningitidis serotyping. Direct examination of gram-stained smears made by students from their own specimens: dental plaque, gingival pocket content, stool. Cultural characteristics of different rods on MacConkey agar: lactose-positive colonies (E. coli), lactose-negative (salmonellae, shigellae, proteus), mucoid (klebsiellae). Evaluation of salmonella’s colony morphology on SS agar and pseudomonas on cetrimide agar. Demonstration of oxidase test.– Differentiation of gram-negative rods on the basis of their biochemical features API. VITEK tests. Demonstration of kits for Salmonella and Shigella serological typing. Visual inspection of anaerobic bacteria cultures. 5. Diagnostics of viral and fungal infections. Infections caused by Candida, Cryptococcus, Malassesia, Pneumocystis, Trichosporon, Geotrichum, Aspergillus, dermatophytes. Factors affecting the development of fungal diseases. Clinical forms (manifestations) of fungal infections. Immune response to fungal agents. Mycotoxins. General scheme of mycological examination: specimen collection, direct smears (invasive forms), cultures, differentiation of morphological and biochemical features, serological diagnostics, skin tests. General indications and principles of viral diagnostics: • specimen collection and transportation (specimen types, optimal period of sampling, storage); • virus isolation - propagation in cell lines, chick embryos, sensitive animals, virus identification (microscopic, serologic and molecular methods); • detection of virus particles (electron microscopy), viral antigen or genetic material in specimen (direct examination) • determination of antibody titer in serum (test: complement fixation, neutralization, hemagglutination inhibition or hemadsorption, immunofluorescence, enzyme immunoassay, radioimmunoassay); Diagnostics of infections caused by hepatitis viruses, HIV, influenza virus, rabies virus, CMV, BKV. Practice: Estimation of fungal colony morphology on Sabouraud agar, chromogenic medium, and Dermasel (dermatophytes). Estimation of fungal cell morphology in slide culture. The readout of germ tube test. 3 Observation of lactophenol cotton blue preparation – estimation the presence of fungal hyphae. Detection of soluble Candida and Aspergillus antigens in patient sera by ELISA. Detection of Aspergillus and Pneumocystis jiroveci DNA in BAL, sputum, bronchial washings by Real-Time PCR. Demonstration of preparation from cell cultures: a cytopathic effect, haemadsorption. Detection of virus by hemagglutination method - slide reaction (qualitative) and tube test (to determine viral titre). Detection of rabies virus antigens in brain tissue of a rabid animal (DIF). Demonstration of the biological activity of bacteriophages (plaques). Detection of specific antibody by hemagglutination inhibition assay (influenza, mumps, measles). The detection of HBsAg by ELISA method. Determination of DNA CMV and BK virus in serum by Real-Time PCR. The quantitative determination of antibodies against Epstein-Barr virus (class IgM and IgG) by Luminex Map. 4 REGULATIONS 2014/2015 Medical microbiology for English speaking students of 2/3rd year of the Medical Faculty PMU The microbiology courses are conducted in the form of seminars (16 hours in the summer semester, 14 h in the winter semester) and practical classes (20 hours in the summer semester, 20 h in the winter semester). The microbiology course finishes with a final theoretical examination in winter exam session. Seminars and classes (labs): 1. Lessons are conducted in groups established by the Dean’s Office. 2. Students are obliged to use protective coats - only those which are available in our Department. Each student is required to keep and leave a classroom clean and tidy. Any wastes, contaminated reusable, objects etc. should be placed in appropriate, labelled containers. 3. Bringing food and drinks into the classroom is prohibited as well as using mobile phones during seminars and labs. 4. The attendance at both all seminars as well as all classes is obligatory. Before each seminar the student must personally sign the attendance list. 5. Students are obliged to be prepared for each seminar and class according to the topic. 6. During seminars current theme is discussed with particular emphasis on issues requiring additional explanations. Seminars complete the textbook knowledge, organise it and interpret inaccuracies and discrepancies possible in some sources. They have a form of a dialogue between students and teacher. The knowledge of discussed topics is essential for the credit for each class and is required during a final examination. 7. Every absence (only exceptional situations) has to be justified and documented. A medical certificate or other documents must be provided within two weeks. More than three absences in microbiology course result in “red condition” - student does not receive a credit and is not allowed to take the final examination. 8. The absences have to be both made up practically as well as passed theoretically. 9. During practical classes in microbiology students are obliged to keep protocols (should be printed by students) - for each topic compulsory practical work will be given to perform by each student. At the end of the class given work will be evaluated by an assistant and accepted or not. Disapproved work needs to be repeated during subsequent classes or during additional classes at the end of semester. 10. Each class begins with test of current topic (10 questions of different kind, short detailed specific question-answer test, a single one best answer questions). To pass the test 60% of correct answers is required. 11. Student has a right to retake every lesson topic twice: the first retake within the next two weeks, the second one, common to all interested students, at the end of the semester. Second retake is not allowed if student have negative marks from a half of classes, in this situation student has no credit from course. 12. The student who did not pass retakes on fixed dates (but not more than half of the subjects) may write “last chance” retake test - negative mark in this retake is equivalent to receiving a “red condition”. 13. Retakes should be taken with the teacher who had carried out given class. 14. Retakes can have oral and written forms. 15. Practical retake can be made up with another group in the same week (according to the topic) or during special retake classes at the end of semester (after the theoretical retake). 16. There is no possibility to correct (upgrade) the marks. 17. Three lateness for seminars will be treated as one absence and has to be made up in the form of paper on a given topic. Microbiology examination. 1. The condition of taking the final credit is credit for all subjects. 2. The examination has a written form (single choice 60-questions test, 60% correct answers for passing). Evaluation of the final exam test (test criteria): 36-40 points - sufficient, 41-45 - satisfactory, 46-50 - good, 51-55 - very good, 56-60 excellent. 3. The first repeat examination has written form (as above), the second one can have written or oral form. 4. Students who have attended seminars and classes (only one justified absence is allowed), obtained an average of marks from classes at least 4,4 and gained a favourable opinion of his teacher have the opportunity to take so-called “zero date” final exam in microbiology. 5. No exemptions from the examinations are provided. 6. After the exam, students have the right to inspect the answer sheet for 1 week from the date of announcement of results. 7. Completion of the final exam results will be announced to students within 5 University working days. All situation not included in this regulation will be considered individually by the Heat of the Department – written application should be applied in secretary’s office. The tutor responsible for the foreign student course of medical microbiology in our Department: Dr Ludmiła Szymaniak Recommended reading – the newest editions of: 5 1. 2. 3. 4. 5. 6. Medical Microbiology - Patrick R., Ph.D. Murray, Ken S., Ph.D. Rosenthal, George S., Ph.D. Kobayashi, Michael A. Pfaller Jawetz, Melnick & Adelberg’s Medical Microbiology – Geo. F. Brooks, Karen C. Carroll, Janet S. Butel, McGraw-Hill Medical; Notes on Medical Microbiology, Including Virology, Mycology and Parasitology. Katherine N. Ward, A. Christine McCartney, Bishan Thakker. Medical microbiology 2nd ed. Edinburgh [etc.]: Churchill Livingstone,: Clinical Microbiology made ridiculously simple Ed. 4, M. Gladwin, B. Trattler Oxford Handbook of Infectious Diseases and Microbiology - Estee Torok, Ed Moran, and Fiona Cooke Antimicrobial Chemotherapy. R. Finch, D. Greenwood, , P. Davey, Ebrary of PMU 6 Protocol No 2 (physiology of bacteria). 1. Blood agar - agar with 5% sheep blood Describe types of hemolysis (cultures of streptococci on the solid sheep blood medium): - alfa ………………………………………………………….give examples…… - beta …………………………………………………………give examples…………. - gamma………………………………………………………give examples…………… 2. Perform the catalase test with bacteria indicated by your teacher. Give the result in a descriptive form:…………………………………………………. Catalase test is used to differentiate ................................... from .................................... 3. McConkey is the …………………………………………….(specify the type of medium) Lactose (+) colonies have……………………… colour. Give examples of bacteria:……… ………………………………………………………………………………………….. Lactose (-) colonies have……………………… colour. Give examples of bacteria:……… ………………………………………………………………………………………….. 4. Chapman medium is used for the detection of....................................... Mannitol (+) colonies have…………….. colour. Give examples of bacteria:……… Mannitol (-) colonies have…………….. colour. Give examples of bacteria:……… 5. Complete: sheep blood agar Chapman’ s medium (MSA) Macconkeya agar chocolate agar Coccosel Pyocyanosel (cetrimide agar) Sabouraud’s medium of medium tive factor rentiating r which oorganisms ible color olonies 6. Specify the type of bacteria growing on chromogenic medium (indicated by your teacher) using the instruction. 7. Read an API biochemical test (indicated by your teacher) using the instruction. 7 8. Describe bacterial or fungal colonies (from plate indicated by your teacher). Give the following features: - name of the medium:………………………………………………………….. - differentiating feature:……………………………………………………………… - colony smell:……………………………………………………………………… - colony appearance:……………………………………………………………….. 9. Bacterial culture in a liquid medium – mark in the picture in which part of the tube gather strictly aerobic, facultatively and obligatively anaerobic, microaerophilic bacteria. 5. Each student collects specimen from the nose, throat, skin, conjunctival sacks, external auditory meatus, etc. and streaks onto growth media and note types of the media. 8 Protocol No. 3 (natural flora, Gram positive) 1. Read all plates which were inoculated by you and your colleagues last week (natural flora cultures), describe by the formula: amount of different colony types on the plate, their color, shape, the presence of hemolysis, other differentiation factors. Specimen e. g. nose e. g. oral cavity e. g. skin (body place) Culture medium Sheep blood agar (COS) McConkey medium Chapman medium (MSA) Saburaud medium Chocolate medium 2. Perform 2 Gram stained smears of selected colonies (suggested by the teacher) and give the result: a)…………………………………………b)………………………………………………….. 3. Examine and compare slides stained by Ziehl-Neelsen and fluorescence methods. Describe the appearance of mycobacteria in preparations. 4. Give culture media for the cultivation of Mycobacterium spp.:…………………………… ………………………………………………………………………………………………………… 5. Examine mycobacterial growth on solid media. Describe the colonies morphology…………………………. ……………………………………………………………………………………. 6 What is the importance of mycobacterial DNA detection in clinical specimens? - Give application of the method, its limitations, examples of results. Analyze prepared plates with microbiological examination of some clinical specimens. Assess: direct smear (prepared in advance or yourself), the growth on media (colonies morphology, smear from culture), presumptive identification 7. Differentiation of staphylococci Specimen type Direct examination Sheep blood culture Chapman culture Simple agar culture Catalase CF, coagulase Biochemical test Other tests 9 8. Differentiation of streptococci Specimen type Direct examination Sheep blood culture – hemolysis type Granada or other chromogenic media Simple agar culture Catalase Optochin test Biochemical test 9. Differentiation of enterococci: Specimen type Direct examination Sheep blood culture – hemolysis type Granada or other chromogenic media Simple agar culture Culture media with esculin / potassium tellurite Catalase Motility test Biochemical test Other tests 10. Observe and describe the direct smear of wound secretions in case of gas gangrene…………………………. 10 11. Describe colony morphology of Bacillus cereus and Clostridium perfringens:………………………………………. 11 Protocol No 4(Gram negative ) 1. Prepare a direct smear of gingival pocket, interdental gap or dental plaque (a technique presented by teacher) - draw and describe the preparation. 2. Find plates with rods listed in the following table and describe their colony morphology, in the description use name of substrate present in the medium -such as lactose (+): Bacterium/ type of medium sheep blood agar MacConkey agar SS agar CPS – chromogenic meduim E. coli Proteus sp. Klebsiella sp. Serratia sp. Citrobacter sp. Enterobacter sp. Salmonella sp. Pseudomonas aeruginosa Acinetobacter baumanii Stenotrophomonas maltophilia 3. Perform oxidase test with strain indicated by your teacher, Make a note of the result. Strain ............................................... oxidase ..................................................... 4. Draw the pattern of positive and negative Hodge test. What is an importance of KPC detection?............................................................................ Which bacteria produce KPC?........................................................................................................ 5. Observe at least 2 preparations from cultures of Gram (-)anaerobes. Give the name of the strain. What can you see? 1…………………………………………………………………………………………… 2………………………………………………………………………………………… 12 5. Differentiation of Moraxella i Neisseria spp. Specimen type Direct examination Sheep blood culture VCA3 medium culture (vancomycin colistin amphotericin ) Oxidase test Biochemical test Antibiogram- method Other tests 13 Protocol No 5 (fungal and viral infections) 1. Interpret serologic of markers of hepatitis B (given in the table) for current infection, reinfection, chronic form of hepatitis B, etc. Test result Interpretation HBsAg (-) anti-HBc(-) Ab anti-HBs(-)Ab HBsAg (-) anti-HBc(+) Ab anti-HBs(+) Ab HBsAg (-) anti-HBc(-) Ab anti-HBs(+) Ab HBsAg (+) anti-HBc(+) Ab anti-HBc (+) IgM Anti-HBs(+) Ab HBsAg (+) anti-HBc(+) Ab anti-HBc (-) IgM anti-HBs(-) Ab HBsAg (-) anti-HBc(+) Ab anti-HBs(-) Ab 2. Complete the table: Virus Test What is detected? Clinical usefulness HIV CMV Influenza virus EBV RSV Rotavirus HPV BK virus 14 Name of disease/ clinical syndrome Treatment - causal (give drug/s), or symptomatic? 3. Diagnosis of dermatophytes - fill in the table after discussions with your teacher. Use available tests. Types of specimens collected for testing Direct examination – how is it made and evaluated? Culture Media: Growth time: Culture conditions (incubation temperature, atmosphere) Identification of species Antifungal susceptibility testing 4. Describe colony morphology (obverse/reverse – colour, texture, size, topography) selected species (at least 2) of dermatophytes in the media -. a. Species name ........................................ Colony morphology: .................................................................... b. Species name ........................................ Colony morphology ........................................................... 5. Diagnosis of Candida infections – fill in the table after discussions with your teacher. Use available tests. Types of specimens collected for testing Direct examination - perform and describe Culture Media: Growth time: Culture conditions (incubation temperature, atmosphere) Species identification – germ tube and biochemical test assessment Antifungal susceptibility testing – methods, reading the test Determination of mannan antigen, results, interpretation 6. Determination of galaktomannan antigen in patient's blood and other clinical specimens – test results, interpretation. 7. Real-time PCR in the diagnosis of fungal infections - examples of the results, the application of the test. 15