* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Congenital Cardiac Abnormalities - Nicole Stevens
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Aortic stenosis wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Congenital heart defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
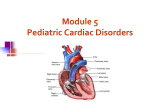
CONGENITAL CARDIAC ABNORMALITIES IN NEONATES BY: NICOLE STEVENS Heart structure Left and right side of heart separated by a septum Left and right atriums are collecting chambers for blood, the right side collects from the body and the left from the lungs The atriums lead into the ventricles, which are the pumping chambers. The left pumps to the body and the right pumps to the lungs. Heart Structure Valves in the heart ensure the correct directional flow of blood. Between the right atrium and right ventricle is the tricuspid valve. Between the left atrium and left ventricle is the mitral valve Between the right ventricle and the pulmonary artery is the pulmonary valve Between the left ventricle and the aorta is the aortic valve Embryology Heart develops between the 3rd and 7th weeks of pregnancy. Heart starts as a hollow tube, as it grows it is forced to bend and rotate – resulting in the formation of all structures At 8 weeks the heart is functioning and looks like a small adult heart In-utero structures In utero nutrients and oxygen are provided via the placenta The lungs are bypassed The foramen ovale is a hole covered by a flap that allows right to left blood flow from the right atrium to the left atrium (avoiding blood going into the right ventricle and pumping to the lungs). The ductus arteriosus also allows shunting away from the pulmonary circuit by moving blood from the pulmonary artery across to the aorta. Congenital heart defects A defect that a baby is born with. Can effect: The chambers The major arteries The heart valves Or a combination of these Congenital defects are caused by a problem in the heart’s development during the first few weeks of pregnancy; exact cause may be unknown, but there are risk factors. Risk Factors Infections (eg German measles) Certain medications can be teratogenic Nicotine Alcohol consumption Diabetes Family history (small risk only) Approx. 1 in 100 babies are born with a heart defect, many defects are minor and can be corrected with medication and/or surgery. Murmurs Caused by turbulence in the flow of blood through the heart valves Can be a sign of heart defects Commonly heard when there are septal defects eg. ASD, VSD A patent ductus arteriosus will also be heard as a murmur. Often the louder the murmur the smaller the defect (creates more turbulence) Arrhythmias Caused by problems in the hearts electrical system, examples: Bradycardia: beating too slowly Tachycardia: beating too fast; SVT unresolved will need emergency management to revert (eg with ice, +/- adenosine Atrial fibrillation: irregular and inefficient beating of the atriums Long QT syndrome: genetic, can be life threatening Diagnosis Pregnancy ultrasounds Medical history Physical examination, auscultation ECG (particularly with arrythmias) CXR (check size and shape of heart; fluid build up in lungs) Echocardiogram (heart ultrasound) Cardiac catheterisation (check pressures, oxygenation in the different chambers; angiography to check flow); also can be used as a treatment option with the balloon angioplasty procedures and insertion of stents. Medications Digoxin: improves contractility Diuretics: increase urine output ACE inhibitors: dilation of blood vessels In neonatal period: Ibuprofen: PDA closure Prostaglandin: keep PDA open, in duct dependent disorders Inotropes: to improve contractility Sildenafil: dilation of pulmonary vessels Nitric: PPHN management Duct Dependent CHD Need flow through PDA to maintain systemic circulation: Coarctation of the aorta Critical aortic stenosis Hypoplastic left heart syndrome Need flow through PDA to maintain pulmonary circulation: Pulmonary atresia Critical pulmonary stenosis Tricuspid atresia (between right atrium and ventricle) Tetrology of fallot Systemic and pulmonary circulations separated: Transpostion of the great arteries Tetrology of Fallot Effects about 5 out of every 10,000 babies Involves 4 heart defects: a large VSD, pulmonary stenosis, right ventricular hypertrophy, an overriding aorta (aorta is located between the left and right ventricles, directly over the VSD, thus allowing oxygen poor blood to flow into the aorta/body) Requires surgery to repair and prolong life Presentation If undiagnosed antenatally you may be caring for these babies on postnatal ward, or visiting on domicillary: Difficulty feeding Increased WOB, increasing cyanosis (largely unresponsive to oxygen therapy) Tachycardia, tachypnoea May or may not be a murmur Collapse, grey appearance, weak or absent peripheral pulses. Assessment Arterial blood gases (preferable from right radial artery Pre and post ductal saturations Four limb BP’s Echocardiogram Management Intubate if necessary Gain x 2 IV access points (eg double lumen UVC, or 2 peripheral cannulas) Commence prostaglandin infusion Bloods (FBE, CRP, Culture, gases) Fluid management Antibiotics Inotropes if required Transfer to a tertiary facility PROSTAGLANDIN INFUSION Used to maintain patency of Ductus arteriosus Side effects include apnoea and hypotension (monitoring and ability to intubate if required essential) Ensure stable on infusion before transfer Other side effects: jitteriness, myoclonic jerks, irritability, fever and diarrhoea Ventricular septal defects Hole between the ventricles One of the most common CHD’s Can occur in different locations and be different sizes. The septum is mainly muscle in one section and mainly fibrous thinner material in another. The location and size will determine the consequence. Untreated, a large VSD can lead to congestive heart failure, as fluid builds up in the lungs Many small lesions will close of their own accord Adequate growth is a positive sign that a baby is relatively unaffected by the VSD Atrial Septal Defect Hole between the 2 atriums Location and size can vary Presence allows flow from high pressure left atrium to low pressure right atrium; increase risk of pulmonary congestion. Symptoms: failure to thrive, fatigue, shortness of breath ASD that don’t close and require intervention may be managed with the placement of a patch via a cardiac catheterisation proceduce Reference List www.heartfoundation.org.au www.neonatal.org.uk/documents www.nhibi.nih.gov www.cincinnatichildrens.org www.childrenscolorado.org