* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
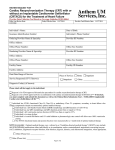
Download CRT Overview - February 2004
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
Cardiac Resynchronization Therapy for Heart Failure Patient Selection and Clinical Outcomes Edited by A kharazi M.D cardiac electrophysiologist Heart Failure (HF) Definition A complex clinical syndrome in which the heart is incapable of maintaining a cardiac output adequate to accommodate metabolic requirements and the venous return. Etiology of Heart Failure What causes heart failure? • The loss of a critical quantity of functioning myocardial cells after injury to the heart due to: – Ischemic Heart Disease – Hypertension – Idiopathic Cardiomyopathy – Infections (e.g., viral myocarditis, Chagas’ disease) – Toxins (e.g., alcohol or cytotoxic drugs) – Valvular Disease – Prolonged Arrhythmias Prevalence of HF by Age and Gender United States: 1988-94 10 8 Percent of Population Males Females 6 4 2 0 20-24 25-34 35-44 45-54 55-64 65-74 Source: NHANES III (1988-94), CDC/NCHS and the American Heart Association 75+ New York Heart Association Functional Classification Class I: No symptoms with ordinary activity Class II: Slight limitation of physical activity. Rest comfortable but ordinary physical activity results in fatigue, palpitation, dyspnea, or angina Class III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary physical activity results in fatigue, palpitation, dyspnea, or anginal pain Class IV: Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency may be present even at rest Poor Quality of Life for HF patients Overall perception of health 70 General population 58 Depression Angina 56 52 AF symptomatic Valve disease symptomatic 48 Chronic Bronchitis 48 55 Heart Failure NYHA Class II 45 Heart Failure NYHA Class III Heart Failure NYHA Class IV 36 Adjusted SF 36 means Hobbs FDR, et al. Eur Heart J 2002;23:1867-1876 Doug Smith: Severity of Heart Failure Modes of Death NYHA II NYHA III CHF CHF 12% Other 26% 59% Sudden Death 24% 64% Other 15% n = 103 Sudden Death n = 103 NYHA IV CHF Other 33% 56% 11% Sudden Death n = 27 MERIT-HF Study Group. Effect of Metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL randomized intervention trial in congestive heart failure (MERIT-HF). LANCET. 1999;353:2001-07. Left Ventricular Dysfunction Volume Overload Pressure Overload Loss of Myocardium Impaired Contractility LV Dysfunction EF < 40% End Systolic Volume Cardiac Output Hypoperfusion End Diastolic Volume Pulmonary Congestion Treatment Approach for the Patient with Heart Failure Stage A Stage B Stage C Stage D At high risk, no structural disease Structural heart disease, asymptomatic Structural heart disease with prior/current symptoms of HF Refractory HF requiring specialized interventions Therapy Therapy Therapy Therapy • Treat Hypertension • All measures under stage A • All measures under stage A • All measures under stages A,B, and C • ACE inhibitors in appropriate patients Drugs: • Mechanical assist devices • Treat lipid disorders • Encourage regular exercise • Discourage alcohol intake • ACE inhibition • Beta-blockers in appropriate patients • Diuretics • ACE inhibitors • Beta-blockers • Digitalis • Dietary salt restriction • Heart transplantation • Continuous (not intermittent) IV inotropic infusions for palliation • Hospice care Hunt, SA, et al ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult, 2001 Diuretics, ACE Inhibitors Reduce the number of sacks on the wagon ß-Blockers Limit the donkey’s speed, thus saving energy Digitalis Compounds Like the carrot placed in front of the donkey Ventricular Dysynchrony • Abnormal ventricular conduction resulting in a mechanical delay – Wide QRS (IVCD); typically LBBB morphology – Poor systolic function – Impaired diastolic function ECG depicting interventricular conduction delay Prevalence of Ventricular Dyssynchrony in Heart Failure Left Bundle Branch Block More Prevalent with Impaired LV Systolic Function Preserved LVSF (1) 8% Impaired LVSF (1) Moderate/Severe HF (2) 1. Masoudi, et al. JACC 2003;41:217-23 2. Aaronson, et al. Circ 1997;95:2660-7 24% 38% Elements of Cardiac Dyssynchrony Atrioventricular Intraventricular Interventricular Cazeau, et al. PACE 2003; 26[Pt. II]: 137–143 Intra-ventricular Dyssynchrony Septal-Posterior Wall Motion Delay • Difference in times from peak excursions of the septum and of the posterior wall at the papillary muscle level • SPWMD 130 ms predicted response (LVEDVi) to CRT in study of 25 pts with QRS 140 ms1 From parasternal short-axis view at papillary muscle level 1. Pitzalis M, et al. JACC 2002;40:1615-1622 septum Posterior wall Parasternal Long-axis View Shown Animation – Ventricular Dysynchrony Click to Start/Stop Etiology of Ventricular Dysynchrony • What Causes Ventricular Dysynchrony?1 – Inter- or intraventricular conduction delays usually manifested as left bundle branch block – Regional wall motion abnormalities with increased workload and stress—compromising ventricular mechanics – Disruption of myocardial collagen matrix impairing electrical conduction and mechanical efficiency 1 2 • Estimated that 15% of all HF patients have dysynchrony2 Tavazziventricular L. Eur Heart J 2000;21:1211-1214. Shenkman et al. Circulation 2000; 102(18):Suppl II, abstract 2293. Clinical Consequences of Ventricular Dysynchrony • • • • Abnormal interventricular septal wall motion1 Reduced dP/dt3 Reduced diastolic filling time1,2 Prolonged MR duration1,2 Click to Start/Stop 1 Grines CL, Bashore TM, Boudoulas H, et al. Circulation 1989;79:845-853. HB, Lee CH, Gibson DG. Br Heart J 1991;66:443-447. 3 Xiao HB, Brecker SJD, Gibson DG. Br Heart J 1992;68:403-407. 2 Xiao, Deleterious Effects of Ventricular Dyssynchrony on Cardiac Function Reduced diastolic filling time 1 + Weakened contractility 2 + Protracted mitral regurgitation 2 + Post systolic regional contraction 3 = Diminished stroke volume Courtesy of Ole-A. Breithardt, MD 1. Grines CL, et al Circulation 1989;79: 845-853 2. Xiao HB, et al Br Heart J 1991;66: 443-447 3. Søgaard P, et al. J Am Coll Cardiol 2002;40:723–730 Cardiac Resynchronization Therapy • The therapeutic intent of atrial-synchronized, biventricular pacing is to restore ventricular synchrony • Complements drug therapy Cardiac Resynchronization Therapy Goals • Improve hemodynamics • Improve Quality of Life Cardiac Resynchronization Therapy • Cardiac resynchronization, in association with an optimized AV delay, improves hemodynamic performance by forcing the left ventricle to complete contraction and begin relaxation earlier, allowing an increase in ventricular filling time. • Coordinate activation of the ventricles and septum. ECG depicting IVCD ECG depicting cardiac resynchronization Cardiac Resynchronization Therapy Increase the donkey’s (heart) efficiency Achieving Cardiac Resynchronization Goal: Atrial synchronous biventricular pacing Transvenous approach for left ventricular lead via coronary sinus Right Atrial Lead Back-up epicardial approach Left Ventricular Lead Right Ventricular Lead Doug Smith: Achieving Cardiac Resynchronization Mechanical Goal: Pace Right and Left Ventricles • Transvenous Approach – Standard pacing leads in RA and RV – Specially designed left heart lead placed in a left ventricular cardiac vein via the coronary sinus Cardiac Resynchronization System Proposed Mechanisms of Cardiac Resynchronization • Improved Contraction Pattern • AV Interval Optimization Click to Start/Stop CRT Improves Cardiac Function at Diminished Energy Cost MVO2/HR (Relative Units) 0.24 p< 0.05 0.22 Dobutamine 0.20 0.18 LV Pacing 0.16 0.14 500 600 700 800 dP/dtmax (mmHg/s) Nelson et al. Circulation 2000;102:3053-3059. 900 1000 CRT Improves Cardiac Function at 6 Months in Moderate to Severe Heart Failure P=0.029 6 LVEF 4 Avg. Change (Absolute %) 2 P<0.001 P=0.12 0 0 MR Jet Area -1 Avg. Change -2 (cm2) -3 P=0.58 Not Reported P<0.001 MIRACLE MIRACLE ICD Contak CD Control CRT Data sources: MIRACLE: Circulation 2003;107:1985-1990 MIRACLE ICD:JAMA 2003;289:2685-2694 Contak CD: J Am Coll Cardiol 2003;2003;42:1454-1459 LV Reverse Remodeling after CRT LV End Systolic and Diastolic Volumes MR area 40 Pacing No pacing † * 200 * 175 Mitral regurgitation (%) Left ventricular volume (mL) 225 * * 150 125 † * * 100 † 35 *† * † 30 * 25 * * 1mo 3mo 20 15 * * 10 Baseline 1wk 1mo 3mo off-immed off-1wk off-4wk Baseline 1wk N = 25 Yu CM, et al, Circulation 2002;105:438-445 off-immed off-1wk off-4wk Mortality/Morbidity Comparison Risk reduction with CRT or CRT + ICD Study (n random.) Follow -up Treatment MIRACLE1 (n=453) 6M CRT JAMA metaanalysis2 (n=1634)* 3-6M CRT Mortality & Hosp. Mortal. & HF Hosp. Mortality 39% 27% 23% HF Mort. HF Hosp. 50% 51% 29% * Includes MIRACLE Date Sources: 1. Abraham WT, et al. N Engl J Med 2002;346:1845-53 2. Bradley DJ, et al. JAMA 2003;289:730-740 P < 0.05 CRT Improves Submaximal Exercise Distance Walked in 6 Minutes Change from Baseline* 60 P=0.004 P=0.003 50 Meters P=0.005 Baseline (meters) 291 ± 101 CRT 40 30 20 Control 10 305 ± 85 0 0 * Paired median change Error bars are 95% CI. 1 3 Follow-up Period (Month) Abraham WT, Fisher WG, Smith AL, et al. N Engl J Med 2002;346:1845-1853 6 CRT Improves Patients’ Quality of Life Minnesota Living with Heart Failure Questionnaire Baseline (score) 59 ± 21 59 ± 20 Score Improvement (points) Change from Baseline* 25 P<0.001 P<0.001 20 CRT 15 Control 10 5 0 0 * Paired median change Error bars are 95% CI. P=0.001 1 3 Follow-up Period (Month) Abraham WT, Fisher WG, Smith AL, et al. N Engl J Med 2002;346:1845-1853 6 CRT Improves NYHA Functional Class P<0.001 Number of Patients 120 52% 100 59% 80 60 30% 32% 40 16% 20 0 4% 6% Improved 2 or more classes Improved 1 class No Change Control Abraham WT, Fisher WG, Smith AL, et al. N Engl J Med 2002;346:1845-1853 CRT 2% Worsened CRT Improves Exercise Capacity in Moderate to Severe Heart Failure P<0.001 60 6 Min Walk 40 Avg. Change (m) 20 P=0.36 P=0.029 P<0.001 0 -20 3 Peak VO2 2 Avg. Change 1 (mL/kg/min) P=0.029 P<0.001 P=0.003 P=0.04 0 0 0 MIRACLE MUSTIC SR Data sources: MIRACLE: Circulation 2003;107:1985-90 MUSTIC SR: NEJM 2001;344:873-80 MIRACLE ICD:JAMA 2003;289:2685-94 Contak CD: J Am Coll Cardiol 2003;2003;42:1454-59 MIRACLE ICD Contak CD Control CRT Optimizing VV Delay Based on Aortic VTI • Obtain Pulsed Wave Doppler of LVOT with several different sequential ventricular paced intervals • Select the setting yielding the largest VTI as the optimal paced interval • CSA is assumed constant, therefore optimal delay is based on VTI alone LV first by 4 ms LV first by 20 ms RV first by 40 ms Relative Cost of CRT Cost per patient Total Annual Expenditures Dialysis CABG PTCA Hip/knee replace CRT CRT+ICD $60 $40 $20 $ thousands Doug Smith: $0 $0 $5 $10 $ Billions $15 $20 CRT: Moderate to severe systolic heart failure with wide QRS Jessup M, Brozena S. Medical Progress--Heart Failure. N Eng J Med 2003; 348: 2007-2018. Copyright 2002 Massachusetts Medical Society. All rights reserved. Cardiac Resynchronization Therapy Patient Indications CRT device: – Moderate to severe HF (NYHA Class III/IV) patients – Symptomatic despite optimal, medical therapy – QRS 130 msec – LVEF 35% CRT plus ICD: – Same as above with ICD indication Conclusions In NYHA Class III and IV systolic heart failure patients with intraventricular conduction delays, cardiac resynchronization therapy: – is safe and well tolerated – improves quality of life, functional class, and exercise capacity – Improves cardiac function and structure – improves heart failure composite response – may have a favorable effect on combined measures of morbidity and mortality Abraham WT, Fisher WG, Smith AL, et al. N Engl J Med 2002;346:1845-1853 Summary • Large number of patients studied in RCTs • Concordant proof that CRT improves quality of life, exercise capacity, functional capacity – Improvements persist through 1 year • CRT reduces the risk of mortality and heart failure due to worsening HF • CRT + ICD reduces risk of mortality • CRT improves cardiac function and structure