* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download THE NEW SIGN GUIDELINES
Survey
Document related concepts
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Coronary artery disease wikipedia , lookup
Transcript
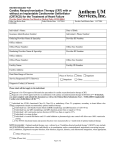
THE NEW SIGN GUIDELINES Malcolm Metcalfe Aberdeen Royal Infirmary SIGN guidelines 6th February 2007 SIGN 93 - ACS Principle recommendations • Patients with NSTEMI at medium or high risk of early recurrent cardiovascular events should undergo early coronary angiography +/- intervention. – GRACE score rather than TIMI recommended • Patients with STEMI treated with thrombolysis should be considered for coronary angiography +/intervention – 4 RCTs. Eg GRACIA -1, at 1 year 12% ARR, 56%RRR combined end point. Risk assessment using the TIMI score (JAMA 2000; 284: 835-) GRACE score www.outcomes-umassmed.org/grace The in-hospital GRACE model was based upon data from 11,389 patients with either an STEMI or a non-ST elevation ACS (1). This model was then validated based upon data from an additional 3972 patients from GRACE and 12,142 patients from the GUSTO IIb trial. Eight independent risk factors were found to account for almost 90 percent of the prognostic information: Killip class Age Class I - no evidence of HF Killip class Class II - findings consistent with mild to moderate HF (S3, lung rales less than one- half way up the posterior lung fields, or jugular venous distension) Class III - overt pulmonary edema Class IV - cardiogenic shock Systolic blood pressure Presence of ST segment deviation Cardiac arrest during presentation Serum creatinine concentration Presence of elevated serum cardiac biomarkers Heart rate Point scores were assigned for each predictive factor and are added together to arrive at an estimate of the risk of inhospital mortality. Pharmacological highlights • Clopidogrel in NSTEMI for only 3 months (saves £2M) • All patients with established vascular disease should be on ACEI • Patients with MI, LVD (LVEF <40%) with either heart failure or diabetes should be given eplerenone SIGN 94 - Arrhythmias • Defibrillation in patients with VF or pulseless VT should be administered without delay in witnessed cardiac arrests and following 2 minutes of CPR in unwitnessed cardiac arrests [B]. • Automated external defibrillators should be sited in locations which have a high probability of cardiac arrests [B]. • IV amiodarone should be considered for the management of refractory VT/VF [A] SIGN 94 - Arrhythmias • In AF rate control is the recommended strategy for asymptomatic patients [A] • Ventricular rate in AF should be controlled with B blockers, rate-limiting Ca antagonists or digoxin [A]. • Ablation and pacing should be considered for patients with AF who remain severely symptomatic or who have LV dysfunction in association with poor rate control or intolerance of rate-limiting medication [B]. SIGN 94 - Arrhythmias • Patients 1 month after MI with symptomatic LV dysfunction (<35%) should be considered for ICD [A]. • Patients with NSVT (esp if inducible), LVEF < 25% or prolonged QRS should be offered ICD [B] • Patients with above but also NYHA III-IV and QRS >120 should be considered for CRT-D [A] • Patients surviving cardiac arrest in absence of ischaemia or other treatable cause should be considered for ICD [A] SIGN 95 Management of CHF • BNP and/or ECG should be used to indicate the necessity for echocardiography in patients with suspected heart failure [A]. • A CXR is still recommended early in the diagnostic pathway to investigate other potential causes of SOB [B]. Pharmacology • ACEIs recommended for all grades of LVSD [A] • B Blockers recommended for all stable LVSD patients [A] • Patients intolerant of ACEI should be given ARB [A] • Patients with LVSD who are still symptomatic despite above can be considered for an ARB as additional therapy [B] • Digoxin should be considered as add on therapy [B] Devices • For patients in SR with drug refractory symptoms due to LVSD and who are in NYHA III or IV with a QRS duration >120ms - CRT should be considered [A]. • Caveats – benefit may be greatest for NYHA II-III – RBBB does not appear to benefit CARE-HF Extension Study Effect of CRT on All-Cause 1.00 Hazard Ratio 0.60 Mortality (95% CI 0.47 to 0.77; P<0.0001) 0.75 Survival CRT Medical Therapy 0.50 0.25 Mean Follow-up 36.4 months (range 26.1 to 52.6) CRT Deaths = 101 (24.7%) (cross-over 4.6%) 0.00 Medical Therapy Deaths = 154 (38.1%) (cross-over 23. 0 Number at risk CRT 409 Medical therapy404 400 800 1200 Time (days) 383 372 358 331 338 298 209 178 85 63 1600 9 6 CARE-HF Extension Study Time to Sudden Cardiac Death 1.00 0.75 CRT P=0.006 Survival HR 0.54 (95% CI 0.35 to 0.84) Medical 0.50 Therapy Medical = 54 sudden deaths (13.4%) 0.25 CRT = 32 sudden deaths (7.8%) Absolute difference = 22 (5.6%) 0.00 0 Mean Follow-up 400 800 1200 (range 1600 36.4 months 26.1 to 52.6) Time (days) SIGN 96 - Stable angina • • • • • • • B blockers first choice [A] Rate-limiting Ca antgonists 2nd choice [A] All patients should receive statin and aspirin LMS - CABG [A] 3VD - CABG preferred [A] Other disease either PCI or CABG [A] B Blockers are recommended in high-risk patients with cad undergoing non-cardiac surgery [A] RISK FACTORS (SIGN 97 RISK ESTIMATION & PREVENTION OF CORONARY DISEASE) • Change in emphasis to embrace social deprivation (ASSIGN) – classical risk factors – FH if <60 years – SIMD (by postcode) • Calculation will be via computer desktop and value expressed as continuous variable. RISK FACTOR MANGEMENT – – – – – – – – – – – age sex smoking status BP DM waist/Hip ratio dietary pattern physical activity alcohol consumption lipid levels psychosocial factors (“stress”) Framingham factors underestimate risk in high risk individuals (eg social deprivation) PREDICTED AND OBSERVED HEART DEATHS IN RENFREW PAISLEY (MIDSPAN) CVD mortality % 25 Observed Predicted 20 15 10 5 0 1 2 3 4 5 Quintiles of Framingham risk Is it feasible, will it do any good? • Whilst good evidence that deprivation score is proportional to risk little evidence that targeting it will gain advantage (level D evidence) • Makes things more complex • Expensive – statins £43M, better BP control £2.8M Avoid bad habits... TREATMENT THRESHOLD • Individuals should be considered to be at high risk if the chance of an initial major vascular event is >20% over 10 years. What level to treat to? Absolute Reduction in LDL-Cholesterol (mmol/l) and Absolute Reduction in Risk of 20% Intervention/Primary Intervention/Secondary Intervention/Both .Control/Primary .Control/Secondary .Control/Both 4S PROSPER LIPID A TO Z 10% CARE Post-CABG HPS MIRACL GREACE LRC-CPPT PROVE-IT WOSCOPS LIPS CARDS ASCOT AF/Tex-CAPS 0% Major Cardiac Event (%) 30% Major Cardiac Event (MCE) 1 2 3 4 LDL-Cholesterol (mmol/l) 5 Adapted from Joint British Societies’ Guidelines1 STATIN EXPENSE • The more aggressive the policy the more expensive the treatment. • Benefits unclear. • Recommendation therefore to keep to existing standards of achieving TC <5mmol/l (LDL <3) This however is the minimum standard and for certain high risk patients a more aggressive policy may be appropriate ASPIRIN • Despite widespread belief of benefit still controversial. – no dispute re secondary prevention – more complex for primary prevention • • • • reduces MI by 30% in males, 0% in females increases haemorrhagic CVA by 40% increases gi bleeding by 70% generally no overall benefit • however when cvs risk >15% may be of net benefit. • Consider use for high risk individuals ACEIs for patients with vascular disease but not LV systolic dysfunction • Good evidence for benefit in higher risk patients (level A) – PVD – CVD – Diabetes • No evidence of significant benefit for low-risk individuals HOPE study And finally...