* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Resynchronization Therapy (CRT): Expanding the role of
Survey
Document related concepts
Transcript
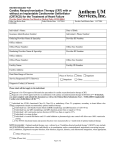
Cardiac Resynchronization Therapy Martin Green, MD, FRCPC Professor of Medicine University of Ottawa Heart Institute Ottawa, Ontario Canada Cardiac resynchronization therapy (CRT) or biventricular pacing is now demonstrated to be effective therapy for both improvement in cardiac function as well as mortality in certain groups of patients with LV dysfunction. First studies in surgical patients were performed by Cazeau et al in 1994. Since then the techniques, technologies and indications have evolved considerably. Studies have shown benefit in ventricular remodeling and performance and more recently in heart failure events and mortality. Patients likely to benefit include those with Class 2-3 NYHA heart failure and wide LBBB. These generally are patients with QRS > 130 msec and LVEF < 0.35. There are still many patients (20-30%) who do not respond to CRT. Some factors predicting nonresponse are amount of scar, LV lead position, RBBB, and narrower QRS. Detailed results of large clinical trials of CRT will be presented. The COMPANION study compared patients with CRT and CRT-D with patients randomized to Optimal Pharmacologic Therapy. Results are shown below: The CARE-HF study was the first to show mortality benefit in patients with more severe CHF (mostly NYHA class 3): MADIT-CRT randomized patients with less severe CHF (mostly NYHA class 2-3) but included heart failure therapy change in the primary endpoint. There was no significant mortality reduction. RAFT included patients with NYHA 2-3 CHF and showed a reduction in mortality as well as heart failure hospitalizations: Death at Any Time During the Study Ev en t‐ fre e Su rvi va l ICD‐CRT (5‐yr survival rate 0.714) HR (95% CI) 0.75 (0.62, 0.91) P=0.003 ICD (5‐yr survival rate 0.654) In conclusion CRT benefit is now well-documented for patients with NYHA class 2-3 CHF, LBBB QRS > 130 msec, and LVEF < 0.35. Issues related to nonresponse will require continued evaluation. References: 1. Cleland JGF et al; The Effect of cardiac Resynchronization Therapy on Morbidity and Mortality in Heart Failure (CARE-HF). N Engl J Med 2005; 352. 2. Linde C et al; Randomized Trial of Cardiac Resynchronization in Mildly Symptomatic Heart Failure Patients and in Asymptomatic Patients with Left Ventricular Dysfunction and Previous Heart Failure Symptoms (REVERSE). JACC vol 52, No. 23, 2008. 3. Moss AJ et al; Cardiac-Resynchronization Therapy for the Prevention of HeartFailure Events. N Engl J Med 2009; 361. 4. Bristow MR et al; Cardiac-Resynchronization Therapy with or without an Implantable Defibrillator in Advanced Chronic Heart Failure. N Engl J Med 2004;350:2140-2150. 5. Bilchick KC et al; Bundle Branch Morphology and Other Predictors of Outcome after Cardiac Resynchronization Therapy in Medicare Patients. Circulation 2010;122;2022-2030. 6. Tang ASL et al; Cardiac-Resynchronization Therapy for Mild-to-Moderate Heart Failure (RAFT). N Engl J Med; November 14, 2010. 7. van der Wall EE et al; Cardiac Resynchronization Therapy; Evaluation by Advanced Imaging techniques. Int J Cardiovasc Imaging (2010) 26:199-202.











![Cardiac Resynchronization Therapy [CRT]](http://s1.studyres.com/store/data/003757028_1-b5efba3cd498dd5814d5097964e81faf-150x150.png)