* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Herpes viruses
Innate immune system wikipedia , lookup
Globalization and disease wikipedia , lookup
Infection control wikipedia , lookup
DNA vaccination wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Neonatal infection wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Molecular mimicry wikipedia , lookup
West Nile fever wikipedia , lookup
Henipavirus wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Marburg virus disease wikipedia , lookup
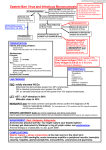
Dr Vidya Pai Naked ,icosahedral capsid viruses are- i. Parvo ii. Papova & iii. Adeno viruses Enveloped viruses are - i. Hepadna ii. Herpes iii. Pox virus - Largest & with complex symmetry. Herpes virus Group has about eight important pathogens. Are ubiquitous and cause disease in plants and animals and are of economic importance. Cause spectrum of diseases Have ability for latency Have ability for periodic activation Also a vesicular rash is common except in CMV & EB viral diseases. These are distinguished by a. Antigenicity b. Location of lesion Lesion of HSV-1 above waist, HSV – 2 below waist [abnormal behavior – may change location] HSV-1 – Acute gingivo stomatitis. Recurrent herpes labialis – Cold sores. Keratoconjunctivitis Encephalitis. HSV-2 - Genital herpes Neonatal herpes Aseptic meningitis Morphology and structure of both are same. Differentiation is by i. Restriction endonuclease patterns of the genomic DNA. ii. Using types specific monoclonal antisera iii. On chick embryo CAM type 2 strains form larger pocks resembling variola. iv. Types 2 strains replicate well in chick embryo fibroblast cells, while type 1 strains do so poorly. v. The infectivity of type 2 is more temperature sensitive than that of type 1. vi. Type 2 strains are more neurovirulent in laboratory animals than type 1. vii. Type 2 strains are more resistant to antiviral agents like IUDR and cytarabine in culture. Humans are natural host for both, but experimental infections can be transmitted into rabbits and mice. enveloped virion – 200 nm. Envelope is derived from the modified host cell nuclear membrane. Envelope has 8 nm long surface spikes. Icosahedral capsid has 152 capsomers. In between envelope and capsid is the amorphous tegument [structural viral proteins]. Linear ds DNA HSV-1 by saliva i.e., direct contact. HSV-2 by sexual contact. The virus is easily inactivated at room temp. and drying, aerosol and Fomite spread are unusual means of transmission. Special situation – oro- genital sex and auto inoculation is not uncommon mode - HSV-2 in oral cavity – 10-20%. HSV-1 in infection of genital tract. Transmission occurs actively if there is active lesion. It also occurs in asymptomatic cases where virus shedding is present. Spread of HSV – 1 infection from oral secretions to other skin areas is an occupational hazard – dentists, respiratory care unit staff, wrestlers. Laboratory acquired, Nosocomial out breaks in hospital and neonatal nurseries can occur. Most primary HSV-1 is thought to occur in child hood because antibody is present in most of us. HSV-2 – occurs during phase of sexual activity – antibody seen during that age. Initial site of infection – i.e. skin or mucous membrane, replication occurs, Migrate in neuron – latent in sensory ganglion cells HSV-1 – trigeminal ganglia HSV-2 - lumbar and sacral ganglia Precise mechanism unknown – may be by lysogeny. Induced by sunlight hormonal changes, trauma, stress, fever, U-V light. Migrate down the neuron and replication in skin causing lesions. Skin lesion – vesicle – [serous fluid with virus particles, cell debris]. When rupture - vesicle release virions and can be transmitted to others Multinucleated giant cell [can be seen by Tzanck smear – fluid with toluidine blue] are typical at the base of lesion. Also there is type specific immunity which can give some cross protection. But immunity is incomplete because reinfection and reactivation can occur in presence of circulating IgG. CMI is important for defense because if suppressed reactivation and severe disease. . 1. Gingivostomatitis – children, fever, irritability and vesicular lesion in the mouth. These heal by 2-3 weeks. But children may be asymptomatic also. 2. Herpes labialis – milder recurrent form of HSV Infection. Also called fever blisters, cold sores – crops of vesicles seen. Recurs frequently at the same site as previous one. Gingivo-stomatitis Herpes labialis Corneal ulcer, lesion of conjunctival epithelium scarring and blindness following recurrence. 4. 5. Encephalitis– Temporal lobe involved frequently, high mortality severe neurologic sequelae with those who survive. Herpetic whitlow - Pustular lesions of finger or hand. Usually in medical personal as a result of contact with patients lesion. 6. Disseminated – Oesophagitis, pneumonia usually seen in immunocompromised because of defect in the T cell. Causes 1. primary and recurrent infection. Genital – painful vesicular lesion – in both sexes. -Lesion in genital, anal area -Primary disease is severe and protracted than in recurrent disease -There is inguinal lymphadenopathy & fever Asymptomatic disease also seen – In men prostate, urethra In female cervix. They Also are source for others. many people have antibody to HSV-2 but no history of disease. 2. Neonatal herpes – Contact of vesicular lesions in birth canal during delivery. Some cases have no visible lesions but still asymptomatic shedding of virus by mother can occur leading to child being infected. Lesion in child – asymptomatic or mild local lesions or severe encephalitis or generalized disease. Caesarian section advised if lesions are seen and positive viral culture of mother. Both HSV-1 & 2 can cause severe neonatal infection after birth through carriers handling the child. It does not cause congenital abnormalities alone. Aseptic meningitis – by HSV-2 is usually mild, self limiting and with few sequelae following recovery. 1. Isolation of virus – Fibroblast cell culture CPE observed in 1-3 days Followed by fluorescent Ab staining of infected cells or detection of virus specific glycoprotein by ELISA. 2. Rapid diagnosis –Giemsa or Toluidine blue -multinucleated giant cell with Cowdry type A inclusion body. PAP stain also for HSV-2. 3. Rapid diagnosis of encephalitis – Fluorescent Ab staining of brain biopsy material, because culture is not useful as virus is rarely recovered. DNA detection in CSF has replaced brain biopsy. MRI scan can detect encephalitis. CSF shows lymphocytic pleocytosis, protein increase and sugar is normal. 4. Serology – Neutralization test used in diagnosis of primary infection ELISA, CF - by observation of increase in Ab titer by paired sera examination. Not useful in recurrent infection because adults already have circulating Ig and recurrences rarely cause rise in Ab titer. 1. Acyclovir [zovirax] – encephalitis and systemic disease of HSV-1 recurrent or primary genital herpes, neonatal herpes by HSV-2 But mutants resistant to acyclovir seen Foscarnet used in these cases. 2. Trifluridine topical [a nucleoside analogue] used for eye infection. 3. Penciclovir for orolabial, recurrent infection and in immunocompetent. No drug treatment prevents recurrences No effect on latent state. Prophylactic acyclovir may help to suppress recurrences. VARICELLAZOSTER VIRUS Disease: Varicella–chickenpox –primary disease Zoster – Shingles – recurrent form. VZV structurally and morphologically similar but antigenically different from HSV. There is a single serotype- same virus causes both type of disease. Humans are the natural host. Replicative cycle – same as HSV. By respiratory droplets, direct contact with lesion. Highly contagious disease of children– population has Ab by 10 years of age. World wide in distribution. 90% VZV infect mucosa of upper respiratory tract. Enter blood skin Vesicular rash [typical] having multinucleated giant cell and intranuclear inclusions in cells of base of lesion. Recovery Latency in dorsal root ganglion. Later in life especially if decrease in CMI, trauma etc. – reactivation leads to vesicular skin lesion and also nerve pain. Immunity But following Varicella is life long Zoster can occur despite varicellar immunity. Zoster can also occur once but frequency increases with age because of waning immunity. Varicella Brief – incubation period 14-21 days. prodromal period of fever and malaise. Followed Crops by papulo vesicular rash of them on trunk and later spreading to head and extremities [centripetal rash] Leads to papules, vesicles, pustules, crusting with severe itching. Usually varicella is mild in children but severe in adults. In adults- severe symptoms, profuse rash, which may be sometimes hemorrhagic and bullous. Complications in aged are varicella pneumonia and encephalitis, myocarditis, nephritis, cerebellar ataxia, meningitis, erythema multiforme. Reyes syndrome – encephalopathy, liver degeneration is associated with VZV, influenza B virus especially with children given aspirin [unknown pathogenesis]. painful vesicles along the course of a sensory nerve of the head or trunk. Pain lasts for weeks and post zoster neuralgia can occur and is very debilitating requiring ganglion surgery often as treatment. It can also cause Bell’s palsy - Zoster of facial nerve. If there is tympanic involvement and Bell’s palsy -it is called Ramsay Hunt Syndrome. In immunocompromised – systemic dissemination – pneumonia which is life threatening. Clinically chicken pox or shingles can be diagnosed Presumptively by Tzanck smear – similar to HSV. Definitive diagnosis by isolation in cell culture and use of specific antiserum to identify growth inside the cell line. Rise in titer of antibody [paired sera] useful for diagnosis of chickenpox. Not useful for zoster because antibody already present. Normal persons no need of antiviral therapy. In immunocompromised Acyclovir can be given in systemic disease. Foscarnet for resistant mutants. In zoster for accelerating healing of lesion – Acyclovir, famciclovir, valacyclovir cure – but these do not cure latent state. No effect on post zoster neuralgia which usually effects old people. Acyclovir in immunocompromised useful. VZIG – high titer of antibody virus – passive immunization. VZV virus – live attenuated [varivax] prevent varicella – oka strain by Takahashi. One dose for 1-12 yrs,Teenagers 2 doses. For zoster not useful Diseases – Cytomegalic inclusion disease [especially congenital abnormalities] in neonates. Pneumonia and other diseases in immunocompromised Heterophile negative mononucleosis in immuno competent. Properties – Structurally & morphologically similar to HSV. Antigenically Humans different, single serotype. are natural host, animal strains do not infect. Giant cells are formed hence the name Replication – Similar to HSV. Unique feature – some of the immediate early proteins are translated from mRNAs brought into the infected cell from the original virion and not from the mRNA synthesized in the newly infected cell. Variety of modes. Early in life – across placenta, within birth canal, mothers milk Common mode – saliva in children Later in life – sexually – present both in semen and cervical secretion Blood transfusion and organ transplants. World wide in distribution – 80% of adults have antibody. Cytomegalic inclusion disease. Multinucleated inclusions. giant cells and ‘owl’s eye’ Many organs effected – congenital abnormalities results. Commonly fetal infection is due to mother who contracts the virus during 1st trimester and also this mother has no antibodies to neutralize the virus. Infection in children and adults – asymptomatic except in immunocompromised. CMV enters latent state also in leucocytes and reactivated if decrease in CMI. It can persist in kidneys for years. CMV reactivation from cervical cells leads to infection during birth CMV causes immunosuppression by inhibiting T cells. Host defense is circulating antibody and CMI – this is important because its suppression leads to systemic disease. Approximately 20% of infected infants – cytomegalic inclusion disease – microcephaly, seizures, deafness, jaundice and purpura. Hepatosplenomegaly is very common. Cytomegalic inclusion disease is one of the leading causes of mental retardation Infected infants can continue to excrete CMV, especially in the urine, for several years. In immunocompetent adults, CMV can cause heterophile negative mononucleosis, which is characterized by fever, lethargy and the presence of abnormal lymphoctyes in peripheral blood smears. Systemic CMV infections, especially pneumonitis and hepatitis, occur in a high proportion of immunosuppressed patients, eg. those with renal and bone marrow transplants. In AIDS patients, CMV commonly infects the intestinal tract and causes intractable diarrhea. CMV also causes retinitis in AIDS patients, which can lead to blindness. The usual approach- culturing in special tubes called shell vials Later immunofluorescent antibody used to detect growth Diagnosis In in 72 hours. cell cultures virus remains cell associated and CPE is slow [1-2 weeks]. Immunofluorescence with specific antibody will detect the virus in cultures. If available, PCR-based assays that detect viral nucleic acids are also useful. Others - fluorescent antibody and histologic staining of inclusion bodies in giant cells - urine and in tissue [samples]. The inclusion bodies are intranuclear and have an oval owls eye shape. A 4 fold or greater rise in antibody titre is also diagnostic. PCR based assays for CMV DNA or RNA in tissue or body fluids, such as spinal fluid, are also very useful. IgM in serum by ELISA – can also be employed. Treatment Ganciclovir [Cytovene], Cidofovir [Vistide], Fomiversin [Vitravene] is used in the treatment of CMV retinitis and pneumonia in patients with AIDS. Fomiversin – antisense DNA approved for intraocular treatment of CMV retinitis [latest drug and the only antisense DNA approved for human use]. Foscarnet CMV is also good but many side effect. is resistant to acyclovir. Prevention No vaccine Ganciclovir can suppress progressive retinitis in AIDS – so prophylactic drug. Isolation Blood of infants shedding virus in urine transfusion to new born or to anyone should be CMV negative. As for as possible CMV antibody negative donors or organs should be used to transplant to antibody negative individuals requiring transplantation. Named after Epstein and Barr They observed the virus under electron microscope from cultures of lymphoblasts derived from Burkitt’s lymphoma. It is implicated in Burkitt’s lymphoma, other B cell lymphomas, nasopharyngeal carcinoma. It is also associated with a whitish nonmalignant lesion on the tongue called hairy leukoplakia – especially in AIDS patients. Commonly it causes infectious mononucleosis [IM] or kissing disease or glandular fever commonly in teenagers. Important properties EBV is structurally and morphologically identical to other herpesvirus but is antigenically different. Has a VCA antigen - it is used most often in diagnostic tests. The early antigens [EA] produced prior to DNA systhesis. EB DNA – nuclear antigen located in the nucleus bound to chromosomes. All these help in diagnosis. Others – Lymphocyte determined membrane antigen. Viral membrane antigen. Neutralizing activity is directed against viral membrane antigen. EBV replicates in the nasopharyngeal epithelial cells, salivary glands [Parotids] Lyses the cells and are released in the saliva When B cell is infiltrated it is also a target and gets infected. Here latency is seen – forms a hybrid with B cell Multiple copies of EBV DNA is found in cytoplasm of infected B cell. Some of these genes are transcribed and only a subset of them is translated into proteins. The latently infected cells can also be activated – B cell then can secrete IgM. It has glycoprotein envelope gp350/220 which mediates attachment to CD21 receptor on susceptible cell – C3d receptor of the cell. Humans are natural host. Infection in oropharynx [epithelium or lymphoid tissue?] – Spread to blood – Infect B lymphocyte – Cyto T cell attack infected B lymphocytes. The T cells are atypical lymphocytes[Downey cells] seen in blood smear. EBV can remain latent in B lymphocytes, few copies of EBV DNA integrated to cell genome. Many copies of circular EBV DNA also found in the cytoplasm. Immune response to EBV – first IgM antibody to VCA. IgG antibody to VCA follows and persists for life. IgM useful for diagnosis of acute infection IgG – reveals prior infections. Life long immunity to second episodes of IM is based on antibody to the viral membrane antigen. Non specific - Heterophile antibodies are found. Heterophile antibody of IM agglutinate sheep or horse RBC in laboratory [Forssman antibody is human serum can cross react with these antigens So it is removed by adsorption with guinea pig kidney extract prior to agglutination]. These antibody do not react with any component of EB virus. Likely explanation is EBV infection modifies a cell membrane constituent so that it be comes antigenic and induces heterophile antibodies. Usually heterophile antibody disappears within 6 months after recovery. These are not specific for EBV as they can also be found in Hep B and serum sickness. Most shedding of virus occur in the oral cavity. So contact with saliva – kissing, contaminated eating utensils transmit. Commonest world wide During childhood most infection are asymptomatic In adolescents it causes infectious mononucleosis or glandular fever. In immunocompromised it has oncogenic potential and causes Burkitts lymphoma, naso pharyngeal carcinoma [China], thymic carcinoma [USA]. 15-25 age group Incubation period 4-7 weeks. Sore throat exudative tonsillitis, generalised lymphadenopathy, fever, malaise headache, sweating, fatigue, G-I discomfort. Sometimes liver, spleen enlarged A maculopapular rash follows treatment with ampicillin This is due to immune complexes with antibody to Ampicillin. So contraindicated. Lasts for 2-3 weeks Complication – Guillain Barre syndrome, Bells Palsy, meningo encephalitis, transverse myelitis, hemolytic anemia, thrombocytopenia, carditis, nephritis, pneumonia and splenic rupture. 1. Burkitt’s lymphoma – malignant B cell lymphoma seen in equatorial Africa, New Guinea where malaria is hyperendemic. EBV is usually acquired early in life. Malaria is the co-factor which potentiates the oncogenic potential of virus from B cell. EBV genome DNA has been found as an episome in the African Burkitt’s, lymphoma cells. The cells themselves do not produce virions. But if grown, in vitro virions are produced. 2. Nasopharyngeal carinoma – Racial and geographical. Seen in Chinese, Eskimos, Green landers. Virions have been isolated form the malignant epithelial cells. 3. B cell lymphoma – Immunodeficient patients eg. patients, transplant recepients may develop lymphomas. HIV these 4. Oral hairy leukoplakia – In HIV patients, capsid of EBV seen in affected tissues. 5. Thymic carcinoma – seen in USA. Hematological approach – absolute lymphocytosis 10,000 – 20,000 cells/ cumm Mainly lymphocytes and monocytes 20-30% or more ‘atypical lymphs’. These are large pleomorphic blasts with deeply basophillic vacuolated cytoplasm and globulated nuclei. These are present in blood for 2 weeks or months [these are cyto - Tcell] 2. Immunological approach – Infectious mononucleosis is accompanied by heterophile aggluttinins. These are IgM elicited by EBV infection. These appear during acute phase in about 90% of patient sera. Peak levels in 2 weeks after onset. Titer decrease rapidly by 4th week and not persists after 3 months. Agglutination of sheep or horse red cells by patients serum adsorbed with guinea pig kidney cell to remove Forssman antibody is basis of test. Tube Not agglutination test – Paul Bunnel test. useful to detect prior infection. Monospot test – Commercial more sensitive, more specific, cheaper than tube agglutination test. Treatment: No EB vaccine. Acyclovir It reduces EBV shedding during administration. does not prevent immortalisation of EBV- B cells. No use in lymphomas or IM Adoptive transfer of EBV reactive T cell is promising treatment For EBV associated lympho proliferative disease Malaria eradication associated with decreased incidence of Burkitt’s lymphoma. Mass screening in China for IgA antibody to EBVAg was useful in early diagnosis of nasopharyngeal carcinoma. 20% of Chinese with elevated IgA were biopsied and found to have carcinoma. Other Herpes viruses Human HSV-6 – Same features of HSV. Infects dividing CD4 + T lymphocytes. Infected cell show ballooning with nuclear or cytoplasmic or both inclusions. Macrophages Isolation are also infected so act as reservoir. from saliva. Culture done on transformed B lymphocytes, NK cell, Glial cells, fibroblasts, epithelial cells. Infection is asymptomatic – in immunocompromised pneumonia. Exanthem subitum or Roseola infantum. Mononucleosis with cervical lymphadenopathy. Lab diagnosis: Peripheral Isolated blood mononuclear cells – used from the co-cultivation with cord blood lymphs Viral PCR Ag then detected by IF using monoclonal Ab. – to amplify viral genome. ELISA – detect virus Ag & Ab Virology and clinical features similar to CMV. HHV – 7 - Discovered is 1990. Roseola infantum, Also infects T lymph using same CD4 receptor. HSV – 8 – 1994 – Lymphotrophic rather than neurotrophic. Kaposi These DNA 2% sarcoma associated in HIV infected. people have Ab. a aplification by PCR is method of choice of general population have Ab. Herpes B – simian virus – Occasionaly infect man Usually fatal encephalitis. Occupational risk in zoo keepers and cell culture technicians. Latent infection in monkeys. Herpes B and HSV-1 cross react antigenically but HSV-1 does not protect from encephalitis from Herpes B. HSV-1 Ab confuse serologically – increase in Ab titer difficult to interpret. Recovery of virus is specific diagnosis. Acyclovir beneficial. Prevention – monkey bite, mask, clothing. Immunoglubulin containing Ab to Herpes B to be given after monkey bite Macrophages Isolation are also infected so act as reservoir. from saliva.