* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular System
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
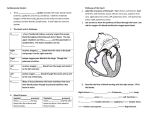
6 THE HEART Heart – an organ the size of your fist and weighing less than a pound that rests on the diaphragm; 2/3 of the heart lies on the left of the midsternal line: Lungs flank the heart: The pointed apex of the heart points toward the left hip and the base (from which the great vessels emerge) points toward the right shoulder 7 1. Pericardium - double walled sac that encloses the heart a) Fibrous Pericardium – outer layer around heart that is tough Connective Tissue i. Protects the heart ii. Anchors it to the surrounding structures (i.e. diaphragm and great vessels) iii. Prevents overfilling of heart - because it does not stretch b) Serous Pericardium – thin slippery 2 layer serous membrane separated by serous fluid i. Parietal pericardium– internal surface of fibrous pericardium ii. Visceral pericardium (epicardium) – external surface of the heart Pericarditis – inflammation of the pericardium resulting in decreased serous fluid and increase in friction and sticking of the pericardial layers, inhibiting heart function 2. Layers of the Heart Wall (all three layers are richly supplied with blood vessels) a) Epicardium – visceral serous pericardium often infiltrated with fat b) Myocardium – middle; cardiac muscle (contracts) c) Endocardium – most internal layer of glistening endothelium that lines chambers (this layer lines the heat cavities and is continuous with blood vessels, capillaries, etc) 8 9 3. Four Chambers (2 atria and 2 ventricles) and associated Great Vessels a) Atria (2) – small, thin walled receiving chambers on the top of the heart, they continue little to the contraction of the heart i. Blood enters the right atrium through three veins Superior Vena Cava – returns blood from body regions superior to the diaphragm Inferior Vena Cava – returns blood from body regions inferior to the diaphragm Coronary Sinus – collects blood from cardiac veins that drain from the myocardium itself ii. Blood enters the left atrium through four pulmonary veins . Pulmonary veins return O2 rich, CO2 poor blood back to the heart. b) Interatrial septum – tissue that separates the atria c) Ventricles (2) –the larger chambers in the bottom of the heart that are responsible for pumping or discharging blood from the heart i. Blood is pumped from the right ventricle into the pulmonary trunk which splits into the pulmonary arteries and routes the blood to the lungs for gas exchange. ii. Blood is pumped from the left ventricle into the aorta, the largest artery in the body which delivers oxygenated blood to the body’s tissues d) Interventrical Septum – tissue that separates the ventricles 4. Blood Flow a) Pulmonary Circuit – the blood vessels that carry blood to and from the lungs (Veins in this system carry O2 rich, CO2 poor blood back to the heart) b) Systemic Circuit – the blood vessels that carry blood to and from all other parts of the body (Veins in this circuit carry CO2 rich, O2 poor blood back to the heart) c) Blood returning from the body (systemic system) that is CO2 rich and O2 poor enters the right atrium and passes into the right ventricle, which pumps the blood to the lungs d) Freshly oxygenated blood from the lungs then is carried though the pulmonary veins back to the left atrium. It then passes to the left ventricle, which pumps it into the aorta. Blood is then transported into smaller systemic arteries to the body tissues e) The walls of the left ventricle (feeds systemic circuit) are three times thicker than the walls of the right ventricle (feeds pulmonary circuit) 10 Bronchial Arteries – blood pumped into lungs to “feed” lungs; these arteries come off the aorta (oxygen rich blood comes from the aorta) Coronary arteries – arteries that come off aorta and “feed” heart (oxygen rich blood) – blood can only “feed” the cells of the myocardium when the heart is not contracted. When the heart beats at a very rapid rate the myocardium may become deprived of oxygen resulting in crushing chest pain called “angina pectoris” which if ignored results in death of myocardial cells and may result in a myocardial infarction or “heart attack” Pulmonary arteries – Do Not “feed” lungs; Do Not carry oxygen rich blood; push blood through lungs to pick up oxygen Heart pumping by the numbers! There are six quarts of blood in an average human In one day the heart pumps the six quarts of blood over 1000 times Meaning that is actually pumps 6000 quarts of blood in a single day! 11 12 5. Microscopic anatomy of the heart – multinucleate, striated, branched and interconnected thru intercalated discs a) Intercellular space: loose Connective Tissue matrix and many capillaries b) Plasma membrane of adjacent cardiac cells interlock at intercalated discs i. Prevent adjacent cells from separating during contraction (prevent tearing of muscles) ii. Ions pass from one cell to the next = depolarize entire heart (allows the heart to contract as a cohesive unit) c) Large amount of mitochondria = 25% of the total volume of a cardiac cell = resists fatigue 6. Heart Valves (4 total) a) Atrioventricular (AV)Valves (2) i. Located between the atrium and ventricle, prevent back flow from contracting ventricles ii. Right AV Valve is the tricuspid valve (has three flexible flaps “cusps” of connective tissue) iii. Left AV Valve is the bicuspid valve or mitral valve (has two flexible flaps of connective tissue) iv. Chordae Tendineae – “heart strings” that anchor the cusps to the walls of the ventricles b) Semilunar Valves (2) i. Aortic Semilunar Valve = guards the base of the aorta and prevents backflow into the left ventricle ii. Pulmonary Semilunar Valve = guards the base of the pulmonary trunk and prevents backflow into the right ventricle Leaky Valves – forces the heart to pump and re-pump the same blood doing more work than necessary and decreasing heart function 13 14 7. Conduction System – noncontractile cardiac cells that will initiate and distribute impulses throughout the heart to contract orderly and sequentially (In other words, the heart does not depend on the nervous system in order to contract. The contractile property is a function of the heart muscle itself) 8. Innervation – although the heart sets its own pace, the autonomic nervous system can control the force and pace at which the heart beats a) Sympathetic = increase rate and force of heart beat b) Parasympathetic = slow rate c) Cardiac centers are located in the medulla oblongata 9. The intrinsic conduction system or nodal system – composite of muscle and nervous system found only in the heart that creates and action potential that passes throughout the heart The Action Potential (Electrical Charge) of the heart passes (from a-e) as follows a) Sinoatrial (SA) node – also called the “pacemaker” located in the right atrial wall and sets the pace for the heart as a whole, initiates signal and determines the heart rate. b) Atrioventricular (AV) node – from the SA node, the depolarization passes through the internodal pathway to the AV node located in the interatrial septum. The AV node delays the signal for a fraction of second before triggering the ventricles to contract. c) Bundle of His = (AV bundle) – also located in the interatrial septum d) Right and left bundle branches – branch into the interventricular septum e) Purkinje fibers – completes the depolarization process 15 CARDIAC CYCLE AND HEART SOUNDS Blood Pressure (BP) – force per unit area exerted on the wall of a blood vessel by its contained blood, expressed in millimeters of Mercury (mm Hg) As blood is pumped from the heart, the Systemic Circuit is under greater pressure than the Pulmonary Circuit. Also, arteries closer to the heart are under greater pressure than those close to the heart. 1. Systolic Pressure – blood pressure during ventricular contraction, averages 120mm Hg 2. Diastolic Pressure – blood pressure during ventricular relaxation, averages 70-80mm Hg Diastole = period when either the atria or ventricles are relaxing Systole = period when either the atria or ventricles are contracting Cardiac Cycle – refers to events of one complete heartbeat (average 75 beats per minute) Heart Sounds: “lub” and “dup” Lub – the closing of the AV valves Dup – the closing the semilunar valves Cardiac output (CO) – the amount of blood pumped by each ventricle in one minute (HR x SV) Stroke Volume (SV) – the amount of blood pumped by each ventricle during one heartbeat Regulation of Stroke Volume – Amount of venous return: if venous return increases the walls of the heart will stretch farther and therefore contract more intensely and they will also increase in speed of contraction 16 Electrocardiography 1. EKG – ECG (Electrocardiography) Electrocardiograph –Electrocardiogram b) See Page 334 c) Electrocardiograph – illustrates the action potential of the heart d) P wave = atrial depolarization (contraction) e) Q, R, S Complex = (act as a Unit) = ventricular depolarization (contraction) f) T wave = ventricular repolarization (movement back to resting state) g) We do not see a wave of atrial repolarization because it is obscured by ventricular repolarization h) Enlarged R wave = enlarged ventricles i) Flat T wave = ischemia = dead tissue j) Prolonged Q-T interval = risk of ventricular arrhythmia