* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download THE INFLAMMATORY RESPONSE
Neuropharmacology wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Hyaluronic acid wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
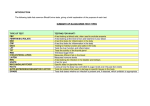
NSAIDs (non steroidal antiinflammatory drugs) THE INFLAMMATORY RESPONSE 1. The inflammatory response is a normal (desirable) defense mechanism. 2. The side effects are undesirable. 3. Normal inflammatory response has an on/off switch. 4. In chronic inflammation something has gone wrong with the OFF switch 5. Therefore we need drugs to control the inflammatory reaction. Mediators of the inflammatory response Complement system histamine serotonin bradykinin - major contributors to symptoms of inflammation leukotrienes - increase vascular permeability - increase mobilization of endogenous mediators of inflammation prostaglandins PGE2 - promote edema and leukocyte infiltration PGI2 - increase vascular permeability, enhance pain producing properties of bradykinin INFLAMMATORY SITE Sensitized lymphocytes release soluble factors ( which recruit & mobilize macrophages to the inflammed tissue.) Additional activated macrophages produce enhanced levels of enzymes and mediators Thereby involving macrophages in the defense against microorganisms and foreign antigens BUT remember that the inflammatory cells have the potential to destroy surrounding tissue. Mediators of inflammation 4 signs of inflammation Redness - due to local vessel dilatation Heat - due to local vessel dilatation Swelling – due to influx of plasma proteins and phagocytic cells into the tissue spaces Pain – due to local release of enzymes and increased tissue pressure Major pathways Eicosanoids Eicosanoids – a family of compounds that are the products of three main pathways which use oxygen as a major cosubstrate. The three pathways are: the cyclooxygenase pathway the lipoxygenase pathway the epoxygenase pathway. COX 1 and COX 2 The key enzyme in the cyclooxygenase pathway is the enzyme cyclooxygenase (COX). There are two forms of cyclooxygenase, COX1 (the predominant form) and COX2. ANTI-INFLAMMATORY DRUGS salicylates e.g., ASA phenylpropionic acids e.g., ibuprofen, ketoprofen pyrazalone derivatives e.g., phenylbutazone indole derivatives e.g., indomethacin Remission inducing / disease modifying drugs: e.g. chloroquine, aurothioglucose, penicillamine, prednisolone Prostaglandin inhibitory activity correlates to antiinflammatory effect MECHANISM OF ACTION Non-steroidal anti-inflammatory drugs (NSAIDs) All NSAIDs inhibit the cyclooxygenase required for conversion of arachidonic acid to endoperoxide intermediate (PGG2 and PGH2). NSAIDs inhibit prostaglandin and thromboxane synthesis, they are potent inhibitors of cyclooxygenase and eliminate all prostaglandins and thromboxanes in every cell they reach Recall that prostaglandins and thromboxanes play crucial roles in: Pain, Inflammation, Fever , Excessive blood clotting Salicylate structure Pyrazolone structure Indole structure Due to the adverse effects of Aspirin (esp. GI and antiplatelet), many newer NSAIDS have been developed. Ibuprofen: PROPIONIC ACID DERIVATIVE -same potency as ASA . -better tolerated (fewer side effects) -ex. Advil; Motrin Available over the counter (OTC) Indomethacin: INDOLE DERIVATIVE -more potent than ASA but inferior at doses tolerated by rheumatoid arthritis patients. -quite toxic -PDA Phenylbutazone: PYRAZOLONE DERIVATIVE -powerful anti-inflammatory drug -usefulness is limited by its toxicity -chiefly short-term therapy Piroxicam: -half-life = 45 hours -administer once a day ( increased convenience) -some GI disturbance Sulindac: -inactive pro-drug closely related to indomethacin -must be metabolized by hepatic microsomal enzymes to active form -long duration of action (half-life = 8h) -adverse effects less severe than other NSAIDS (ex. GI and renal) -ex. Clinoril Ketoprofen: -inhibits both cyclooxygenase and lipoxygenase (decreases PGs, TXs, and LTs) *recall LTs: bronchospam;bronchoconstriction -may be desirable for asthmatics or inflammation plus allergic response -ex.Orudis COX-2 INHIBITORS Cyclooxygenase-1 (COX-1): -constitutively expressed in wide variety of cells all over the body. -"housekeeping enzyme" -ex. gastric cytoprotection, hemostasis Cyclooxygenase-2 (COX-2): -inducible enzyme -immediate-early gene product in inflammatory and immune cells -dramatically up-regulated during inflammation (10-18X) Adverse effects of NSAIDS are theorized to be due to inhibition of COX-1 (ex. GI complications via decreased PGE2 and potentially altered blood flow) In some instances cytoprotectives e.g., misoprostol (PGE2 analogue) may be taken with NSAIDS to reduce GI effects. Selective COX-2 inhibitors were developed e.g., Celecoxib (Celebrex); Roficoxib (Vioxx) which was withdrawn in 2004 due to serious CV effects and in Sept. 2007 Merck agreed to pay 4.8 billion dollars settlement. Nitric Oxide-Releasing NSAIDS NO-NSAIDS Less GI effects than parent NSAID from which they are derived. Comparable anti-inflammatory effect and superior analgesic effect Example: NO-naproxen Parent NSAID: naproxen Possible mechanism: nitric oxide would improve gastric blood flow DIETARY MANIPULATION OF INFLAMMATION Arachidonic Acid (AA) -eicosatetraenoic acid (4 double bonds) Eicosapentaenoic acid (EPA) -5 double bonds EPA EPA is found in fish oil It acts as a substrate for cyclooxygenases and lipoxygenases (thus it competes with arachidonic acid for the enzymes) The prostaglandins, thromboxanes, and leukotrienes produced from EPA are less active than AA metabolites. EPA continued These products can then compete with products of AA metabolism for shared target receptors. Macrophages with a high content of EPA produce less TNF and IL-l (key pro-inflammatory cytokines) Thus, • Dietary EPA supplementation can reduce tissue injury due to PGs, TXs, LTs, and cytokines!! EPA continued Clinical studies have shown decreased morning stiffness and joint pain in rheumatoid arthritis patients with EPA supplementation Potency approximates NSAIDS, with negligible side effects!! Inflammatory events in the gouty joint GOUTY ARTHRITIS: inflammatory mechanism Body fluids supersaturate with urate and urate crystals precipitate in tissues. Resulting in pain and inflammation Phagocytosis of crystals by polymorphs and the migration of leukocytes to the inflamed area Release inflammatory mediators into joint ANTI-INFLAMMATORY DRUGS AND GOUTY ARTHRITIS Colchicine indomethacin adrenal steroids new NSAIDS e.g. sulindac (acute gout) probenecid, sulfinpyrazone allopurinol Mechanism of action of Allopurinol Allopurinol inhibits synthesis of uric acid by competing for the enzyme xanthine oxidase. Hypoxanthine xanthine oxidase xanthine xanthine oxidase Uric acid Allopurinol xanthine oxidase Alloxanthine Glucocorticoids - inhibit phagocytosis inhibit synthesis of IL-1, TNF, PGs LTs. inhibit antigen processing by macrophages stabilizes lysosomal membranes inhibits accumulation of neutrophils and monocytes at inflammation site. inhibit phospholipase A2. Glucocorticoids examples: prednisone dexamethasone Side effects: osteoporosis impaired wound healing edema, hypertension, congestive heart failure CNS effects (euphoria - psychosis) Cushingoid Syndrome