* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Corrected Transposition of the Great Arteries
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Aortic stenosis wikipedia , lookup
Cardiac surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Back
2
Corrected Transposition
of the Great Arteries
Contents
◙◙ Introduction 54
◙◙ Anatomy 55
◙◙ Ventricular Septal Defect 57
◙◙ Conduction System 57
◙◙ Coronaries 58
◙◙ Anatomical Correction of Corrected Transposition of the Great Arteries 59
◙◙ Indication for Anatomical Correction 59
◙◙ Approach and Cardiopulmonary Bypass Strategy 60
◙◙ Modified Senning Operation 61
◙◙ The Goal of Surgery 61
◙◙ Modified Half-Mustard Operation 62
◙◙ The Goal of Surgery 62
◙◙ Arterial Switch Operation for Corrected Transposition of the Great Arteries 62
◙◙ The Goal of Surgery 62
◙◙ Rastelli Operation for Corrected Transposition of the Great Arteries 62
◙◙ The Goal of Surgery 62
◙◙ Bex–Nikaidoh Procedure for Corrected Transposition of the Great Arteries 63
◙◙ The Goal of Surgery 63
◙◙ Double Switch Operation for Corrected Transposition of the Great Arteries {SLL},
with Resection of the Subpulmonary Obstruction in Situs Solitus and Levocardia 64
◙◙ Patient Characteristics 64
◙◙ Specific Steps of Operation 64
◙◙ Closure of the Ventricular Septal Defect During the
Double Switch Procedure 73
◙◙ Senning–Rastelli Operation for Corrected Transposition of the Great Arteries {SLL}
with Ventricular Septal Defect, Pulmonary Atresia, and Dextrocardia 74
◙◙ Patient Characteristics 74
◙◙ Specific Steps of Operation 74
◙◙ Senning–Rastelli Operation for Corrected Transposition of the Great
Arteries {IDD} with Noncommitted Ventricular Septal Defect,
Pulmonary Stenosis, Situs Inversus, and Levocardia 79
◙◙ Patient Characteristics 79
◙◙ Specific Steps of Operation 79
V. Hraška, P. Murín, Surgical Management of Congenital Heart Disease I,
DOI:10.1007/978-3-642-24169-7_2, © Springer-Verlag Berlin Heidelberg 2012
53
54
V. Hraška, P. Murín
◙◙ Modified Half-Mustard and Rastelli Operation for Corrected Transposition
of the Great Arteries {SLL} in Situs Solitus with Dextrocardia 85
◙◙ Patient Characteristics 85
◙◙ Specific Steps of Operation 85
◙◙ Modified Senning and Bex–Nikaidoh Procedure for Corrected
Transposition of the Great Arteries {IDD} with an Inlet Ventricular
Septal Defect in Situs Inversus and Mesocardia 87
◙◙ Patient Characteristics 87
◙◙ Specific Steps of Operation ◙◙ Recommended Reading 88
92
Introduction
Congenitally corrected transposition is a rare condition, characterized by atrioventricular and ventricular–arterial discordance. The clinical presentation and
indication for surgery generally depends on the associated cardiac lesions such
as ventricular septal defect, obstruction of the outflow tract from the morphologically left ventricle, abnormalities of the morphologically tricuspid valve,
and problems with the conduction system.
Operations for congenitally corrected transposition fall into four categories:
1.Temporary palliative procedures (arterial–pulmonary shunt, stenting of the
patent ductus arteriosus, or pulmonary artery banding)
2.“Physiological correction,” preserving the right ventricle as a systemic ventricle and correcting only the associated lesions
3.“Anatomic correction,” utilizing the left ventricle as the systemic pumping
chamber and the mitral valve as the systemic atrioventricular valve
4.Single-ventricle pathway that leaves both ventricles connected to the systemic circuit, providing systemic venous to the pulmonary arterial circuit by
modified Fontan procedure
The long-term outcomes of patients after physiological correction have clearly
demonstrated that the tricuspid valve and right ventricular function is the Achilles heel of the physiology of congenitally corrected transposition. Anatomic
2 Corrected Transposition of the Great Arteries
correction has therefore been proposed in the hope that it might serve patients
better in the long run. At present, the midterm outcomes after anatomical correction are encouraging. However, long-term outcomes show that anatomical
correction has only a slight advantage over other types of surgical treatment.
The long-term survival and functional benefits after anatomic correction have
been demonstrated, particularly in patients with preoperative tricuspid valve
regurgitation.
Anatomical correction represents a group of procedures in which the atrioventricular discordance is “corrected” by an atrial switch (Senning or Mustard), and ventricular–arterial discordance is “corrected” either by an arterial
switch operation, by the Rastelli procedure, or by translocation of the aortic
root (Bex–Nikaidoh operation), depending on the underlying anatomy of the
left ventricular outflow tract and/or morphology of the ventricular septal defect. Three different types of anatomical correction are therefore recognized:
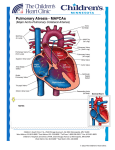
(1) double switch – Senning plus arterial switch operation (S-ASO), (2) Senning and Rastelli (S-R), and (3) Senning and Bex–Nikaidoh (S-BN) (Fig. 2.1).
Ventricles+GAs
Atria
Senning +
Rastelli
ASO
BN
Fig. 2.1
Anatomy
l-Looping of the cardiac tube during embryonic development leads to an abnormal connection between the atrial, ventricular, and arterial segments of the
developing heart. In congenitally corrected transposition, the systemic venous
atrium (right atrium) is connected to the morphologically left ventricle, and
the pulmonary venous atrium (left atrium) is connected to the morphologically right ventricle. The connection of the great arteries is also abnormal, i.e.,
there is a right ventricular origin of the aorta and a left ventricular origin of the
55
56
V. Hraška, P. Murín
pulmonary artery. The ventricles carry their usual inlet valve to their inverted
location, and coronary artery distribution is also abnormal.
The malformation can occur in a situs solitus arrangement {SLL}, or in situs
inversus {IDD}.
In congenitally corrected transposition situs solitus {SLL}, the outflow
tracts of the ventricles are most often in a parallel position, although other relationships do exist (crisscross or inferosuperior position). The entire ventricular
mass is frequently abnormally located within the thorax, the location ranging
from levocardia to meso- or dextrocardia. The right-sided, morphologically left
ventricle gives rise to the pulmonary trunk, and there is usually fibrous continuity between the leaflets of the pulmonary and mitral valves. The subpulmonary
outflow tract (the left ventricular outflow tract) is wedged between the mitral
valve and the interventricular septum. A hemodynamically significant obstruction of the outflow tract of the morphologically left ventricle is a common
finding, occurring in about 40% of patients, particularly in the presence of a
ventricular septal defect.
Apart from pulmonary atresia, the mechanism of obstruction is multifactorial, the factors including valvar stenosis, annular hypoplasia, and a variety
of subpulmonary obstructions (muscular tunnel-like obstruction, membranous
stenosis, an aneurysmal dilation of the fibrous tissue derived from the interventricular component of the membranous septum, or accessory tissue from
atrioventricular valves, etc). The right-sided morphological mitral valve is supported by posteromedial and anterolateral papillary muscles. Overriding and/or
straddling of the mitral valve can be seen in combination with a double outlet
from the right ventricle.
The left-sided morphologically right ventricle empties into the aorta, which
is supported by a complete infundibulum. The aorta is typically located anteriorly and to the left, relative to the pulmonary trunk. The left-sided morphologically tricuspid valve is frequently dysplastic. This abnormality is described
as an Ebstein-like deformity with short, thick chordae tethering the valve, but
unlike Ebstein’s anomaly, apical displacement of the septal leaflet with failure
of delamination is rare. Clinically important insufficiency of the valve is seen
in up to 40% of adults with congenitally corrected transposition. The tricuspid
valve can also override and straddle, causing hypoplasia of left-sided morphologically right ventricle.
2 Corrected Transposition of the Great Arteries
Ventricular Septal Defect
A ventricular septal defect is detected in at least 50% of patients. Due to the
wedged position of the subpulmonary outflow tract in the morphologically left
ventricle, there is gross malalignment between the atrial septum and the inlet
part of the ventricular septum. If this malalignment gap is not filled, a perimembranous ventricular septal defect develops. Such perimembranous defects
occupy a subpulmonary position, extending posteriorly and inferiorly toward
the crux of the heart. The defect opens primarily into the inlet of the morphologically left ventricle; therefore, the posterior margin is formed by an extensive area of fibrous continuity between the leaflets of the pulmonary, mitral,
and tricuspid valves. In rare instances, the defect can be subpulmonary but with
exclusively muscular rims.
If there is pulmonary atresia or subpulmonary obstruction, the malalignment
gap is not so prominent, and usually a large, nonrestrictive conoventricular
defect, naturally committed to the aorta, is found. Defects can also be found
in a doubly committed position, with absence of the septal component of the
infundibulum.
Conduction System
In situs solitus {SLL}, the wedging of the pulmonary valve between the septum and the mitral valve diverts the atrial septum from the ventricular septum,
making penetration of the atrioventricular bundle, which originates from the
regular atrioventricular node, impossible. Instead, the atrioventricular conduction axis originates from a second (anterior) anomalously located atrioventricular node lodged between the annulus of the mitral valve and the superior and
anterior aspect of the limbus of the fossa ovalis. After penetrating the fibrous
trigone (pulmonary to mitral fibrous continuity) the conduction bundle runs
superficially underneath the pulmonary valve, and then descends along the anterior septal surface of the subpulmonary outflow tract before diverging into
the bundle branches. The cord-like right bundle branch extends leftward to
reach the morphologically right ventricle, and a fan-like left bundle branch
cascades down the smooth left ventricular septal surface. When there is a perimembranous ventricular septal defect, the conduction system travels along the
anterosuperior margin of the defect.
57
58
V. Hraška, P. Murín
However, the variability of the conduction system is probably significant.
If there is minimal or no wedging of the pulmonary artery (severe obstruction
within the morphologically left ventricular outflow tract, double outlet from the
right ventricle or pulmonary atresia), better septal alignment is achieved. Then,
both the regular and the anterior nodes (dual atrioventricular nodes) can give rise
to penetrating bundles, producing a sling of conduction tissues. How mesocardia
and dextrocardia in situs solitus effect the alignment of the septum remains to be
seen. From a surgical perspective, the close relationship between the nonbranching bundle and the pulmonary valvar orifice complicates both closure of the
ventricular septal defects, relief of the obstruction within the morphologically
left ventricular outflow tract, or ventricular septal defect enlargement. The position of the atrioventricular node should be anticipated with respect to the degree
of misalignment between the atrial and ventricular septae and the direction of
the enlargement of the ventricular septal defect should be guided accordingly.
In situs inversus {IDD}, there is no septal malalignment, and the atrioventricular conduction axis originates from a posterior atrioventricular node to follow a conventional path along the posteroinferior margin of the ventricular
septal defect.
Coronaries
The Leiden convention is used to describe the origin of the coronary arteries.
For the most common coronary pattern in congenitally corrected transposition {SLL}, sinus 1 (right-hand sinus), which is anatomically the leftward and
posterior sinus, gives origin to the right coronary artery, and the sinus 2 (lefthanded sinus), which is rightward and anterior, gives origin to the main stem
of the left coronary artery. The usual coronary artery pattern is labeled as 1R;
2AD, Cx.
The ventricular topology determines the epicardial distribution of the arteries. The right-sided coronary artery is therefore a morphologically left coronary artery, with a short main stem dividing into the anterior descending and
circumflex coronary arteries. The circumflex artery encircles the mitral orifice,
and the anterior descending artery labels the position of the ventricular septum.
The left-sided coronary artery is a morphologically right coronary artery. It has
infundibular and marginal branches, while encircling the left-sided tricuspid
orifice.
2 Corrected Transposition of the Great Arteries
In situs inversus {IDD}, the epicardial arrangement of the coronary arteries
is completely mirror imaged. The usual coronary artery pattern is labeled as
1AD, Cx; 2R.
natomical Correction of Corrected
A
Transposition of the Great Arteries
Indication for Anatomical Correction
The indications, timing, and type of anatomical correction of congenitally corrected transposition with associated lesions vary according to the clinical state
of the patient, the morphology of the heart, and the patient’s age. There is a
trend toward performing the final correction at about 2 years of age.
Development of cyanosis due to severe left ventricular outflow tract obstruction requires either placement of a modified Blalock–Taussig shunt or stenting
of the patent ductus arteriosus. The definitive operation is usually performed
between the first and second years of life. The type of operation is determined
by the position and size of the ventricular septal defect and morphology of
the atrioventricular valves. A Senning–Rastelli correction with intraventricular rerouting is possible if there is a committed and nonrestrictive ventricular
septal defect. A Senning–Bex-Nikaidoh operation is indicated if creation of a
straight intraventricular tunnel is impossible due to an inlet and/or restrictive
ventricular septal defect. Pulmonary artery banding is placed either to control
congestive heart failure or to prepare the left ventricle for systemic function. In
that case a “loose” pulmonary artery banding should be placed to achieve 50%
of systemic pressure in the left ventricle and to allow patients to “grow into”
the pulmonary artery banding. This policy simplifies the postoperative course
after pulmonary artery banding, and training of the left ventricle is gradual.
Excessive pulmonary artery banding tightening leads to reduced left ventricular function and edema of the myocardium. Occasionally, retraining of the left
ventricle can be achieved only by sequential pulmonary artery banding. The
cutoff for retraining the morphologic left ventricle is about 15 years of age. A
ratio of left to right ventricular systolic pressure of 0.8 or greater, in the presence of a well-preserved left ventricular function, with the indexed left ventricular mass to left ventricular volume ratio >1.5, is considered to be adequate
for anatomical correction.
59
60
V. Hraška, P. Murín
The double switch procedure is indicated as primary surgery between 3 and
6 months of age or when the left ventricle, after the banding, is properly trained
for systemic function.
The modified Senning operation is applicable regardless of the situs, the
position of the apex of the heart and the age of the patients.
Approach and Cardiopulmonary Bypass Strategy
The heart is approached through a median sternotomy. The standard technique
of cardiopulmonary bypass with full flow and mild to moderate hypothermia
(32–28°C) is used. The aortic cannula is positioned high, close to the base of
the innominate artery.
High cannulation of the superior vena cava or cannulation of the innominate
vein is preferable, using an angled venous cannula.
Clip1
Back
The inferior vena cava is cannulated as low down as possible and somewhat
laterally to preserve the Eustachian valve. Myocardial protection is provided by
crystalloid antegrade cardioplegia.
2 Corrected Transposition of the Great Arteries
Modified Senning Operation
The Goal of Surgery
The technique of a modified Senning procedure differs from the original concept, being adapted to the specific atrial morphology of the corrected transposition of the great arteries with underdevelopment of the free right atrial wall,
especially in situs solitus with mesocardia or dextrocardia, or in situs inversus
with levocardia.
There are several important technical points to keep in mind:
1.Dissection and mobilization of the superior vena cava–right atrium junction
is abandoned to preserve pericardial reflection around the right upper pulmonary vein.
2.The initial incision of the right atrium should be close to the atrial–ventricular groove to preserve the anterior free wall of the right atrium for the
systemic venous baffle.
3.The interatrial septum should be completely resected.
4.The superior aspect of the limbus of the fossa ovalis must be effectively cut
off to avoid baffle obstruction from the superior vena cava to the contralateral
tricuspid valve. At the same time, the trapezoid-shaped patch, which is used
for the posterior wall of the systemic baffle, must be seated low, beneath the
superior vena cava–right atrium junction, and should be kept away from the
left pulmonary vein to avoid a purse-string effect on their entrance points.
5.During construction of the pulmonary venous atrium, with pericardium in
situ, care is taken to avoid the sinus node and phrenic nerve.
6.It is important to provide adequate capacity of the pulmonary venous atrium
and to prevent distortion and tension on the atrial–ventricular groove, thus
keeping the mitral valve in an optimal position.
With the technical aspect of the modified Senning procedure well accomplished, the operation is feasible, regardless of age, and allows an earlier indication for correction. The operation is simple, highly reproducible, and applicable, regardless of the situs and position of the apex of the heart. Furthermore,
this technique has the potential to provide adequate capacity of the pulmonary
venous atrium, to preserve optimal geometry of the mitral valve, to minimize
damage to the sinus node, and to make the coronary sinus accessible for electrophysiological studies or intervention.
61
62
V. Hraška, P. Murín
Modified Half-Mustard Operation
The Goal of Surgery
Baffle rerouting of the inferior vena cava to the contralateral tricuspid valve is
indicated if a bidirectional Glenn anastomosis is already in place, or when one
and half ventricle anatomic repair is considered. After resection of the interatrial
septum, the inferior vena cava entrance is connected to the tricuspid valve annulus using an appropriately shaped and longitudinally opened GORE-TEX©
prosthesis. The coronary sinus is incorporated into the baffle.
rterial Switch Operation for Corrected
A
Transposition of the Great Arteries
The Goal of Surgery
The goal and technique of the arterial switch operation for corrected transposition of the great arteries is the same as for complete transposition of the great
arteries. The arterial switch is the procedure of choice if the left ventricle has
been exposed to sufficiently high blood pressure and is therefore able to take
over acutely at systemic pressure, and if the left ventricular outflow tract is free
or surgical relief of obstruction on any level is amenable.
astelli Operation for Corrected
R
Transposition of the Great Arteries
The Goal of Surgery
The goal and technique does not differ from a Rastelli correction of complete
transposition of the great arteries with left ventricular outflow tract obstruction.
The Rastelli operation is chosen in the case of a nonresectable left ventricular
outflow tract obstruction and adequate capacity of the right ventricle. Construction of an obstruction-free and straight intraventricular tunnel is essential
for preserving left ventricular function. In corrected transposition of the great
arteries with pulmonary atresia, the ventricular septal defect is not restrictive
and usually is naturally committed to the aorta, thus allowing the creation of a
straight intraventricular tunnel. In theory, this should be the best morphology
for intraventricular rerouting. The enlargement of a borderline ventricular sep-
2 Corrected Transposition of the Great Arteries
tal defect, while achieving better commitment of the ventricular septal defect
toward the aorta, is a significant risk for surgically acquired heart block. An
anterior position of the conduction system in {SLL} and a posterior position
in patients with {IDD} is to be generally expected, and enlargement of the
ventricular septal defect is performed accordingly. An unfavorable anatomy,
such as a noncommitted and/or restrictive ventricular septal defect or significant straddling of the atrio-ventricular valve, can preclude a Rastelli operation.
Under these circumstances, consideration should be given either to conversion
to the Fontan procedure, or in suitable patients, to aortic translocation.
ex–Nikaidoh Procedure for Corrected
B
Transposition of the Great Arteries
The Goal of Surgery
The goal and technique of the Bex–Nikaidoh procedure for corrected transposition of the great arteries is the same as for complete transposition of the
great arteries. Aortic translocation results in better-aligned outflow tracts. The
divided outlet septum offers excellent visualization of the atrio-ventricular
valve’s attachment as well as the ventricular septal defect borders. Enlargement of the left ventricular outflow tract with the patch can be performed easily
despite the atrio-ventricular valve straddling. The translocated aorta is directly
committed to the left ventricle. The anatomy of the right ventricular outflow
tract is favorable for placement of an oversized pulmonary conduit, and orthotopical placement minimizes the risk of sternal compression. This can result in
improved longevity of the conduit.
However, aortic translocation in corrected transposition of the great arteries
with complex left ventricular outflow tract obstruction is a challenging procedure that should be considered only if the anatomy is inadequate for an intraventricular baffle. The specific issue in corrected transposition of the great arteries is the risk of damage to the conduction system during the division of the
outlet septum. In {IDD} conduction, the atrioventricular bundle arises from the
posterior node to follow the conventional path along the posteroinferior margin
of the ventricular septal defect, which allows the risk-free transection of the
outlet septum. In contrast, in {SLL} the atrioventricular conduction axis runs
anteriorly and cephalically to the pulmonary valve, and then descends along the
anterior margin of the ventricular septal defect before diverging into the bundle
63
64
V. Hraška, P. Murín
branches. Other issues are related to the transfer
of the coronary arteries, which in corrected transposition of the great arteries must be detached and
extensively mobilized, and to progressive aortic
valve regurgitation. Usually, aortic regurgitation is
apparent immediately after surgery, confirming the
importance of the technical aspects of aortic root
transfer.
ouble Switch Operation for Corrected Transposition
D
of the Great Arteries {SLL}, with Resection of the Subpulmonary
Obstruction in Situs Solitus and Levocardia
Patient Characteristics
Age at surgery: 16 months
Diagnosis:
1.Corrected transposition of the great arteries
(2LC; 1R)
2.Left ventricular outflow tract obstruction due
to accessory tissue from the mitral valve
3.Secundum atrial septal defect
4.Situs solitus
History:
1.Prenatal diagnosis
2.Elective surgery
Procedure:
1.Modified Senning
2.Arterial switch operation
3.Resection of accessory tissue obstructing the
left ventricular outflow tract
5.Levocardia
Specific Steps of Operation
Clip1
Preoperative findings.
Back
2 Corrected Transposition of the Great Arteries
65
Clip2
Back
After subtotal removal of the thymus and harvesting of the pericardium, the external anatomy is
examined closely.
Clip3
Back
The right atrium is opened in an oblique fashion.
66
V. Hraška, P. Murín
Clip4
Back
Resection of the subpulmonary obstruction.
Clip5
Back
Evaluation of the left ventricular outflow tract.
2 Corrected Transposition of the Great Arteries
67
Clip6
Back
Excision of the interatrial septum and opening of
the entrance of the right pulmonary veins. Evaluation of the intra-atrial anatomy.
Clip7
Back
Development of the posterior wall of the systemic
venous baffle with a trapezoid-shaped GORETEX© patch.
68
V. Hraška, P. Murín
Clip8
Back
The anterior wall of the systemic venous baffle is
developed.
Clip9
Back
Development of the pulmonary venous atrium using pericardium in situ (Shumaker modification).
2 Corrected Transposition of the Great Arteries
69
Clip10
Back
Both great vessels are transected.
Clip11
Back
Harvesting of the buttons of the right and left coronary arteries.
70
V. Hraška, P. Murín
Clip12
Back
Implantation of the left coronary artery button.
Clip13
Back
Implantation of the right coronary artery button.
2 Corrected Transposition of the Great Arteries
71
Clip14
Back
Lecompte maneuver and reconstruction of the
ascending aorta.
Clip15
Back
Reconstruction of the neopulmonary trunk with an
autologous pericardial patch that has been pretreated with glutaraldehyde for 15–20 min.
72
V. Hraška, P. Murín
Clip16
Back
Final result.
Clip17
Postoperative echocardiogram findings.
Back
2 Corrected Transposition of the Great Arteries
73
fullversion
Back
losure of the Ventricular Septal Defect During
C
the Double Switch Procedure
Clip1
Back
As part of the double switch procedure, when the
systemic venous baffle is completed, the ventricular septal defect is approached by working through
the mitral valve. All sutures should be placed from
the left side of the septum due to the variability of
the conduction system, and one never knows if the
conduction system travels along the anterosuperior
margin of defect only or if there is a conduction
sling. Alternatively, one could consider closing
the ventricular septal defect by working through
the right ventriculotomy or through the aorta, thus
eliminating undue tension on the crux cordis.
74
V. Hraška, P. Murín
enning–Rastelli Operation for Corrected Transposition
S
of the Great Arteries {SLL} with Ventricular Septal
Defect, Pulmonary Atresia, and Dextrocardia
Patient Characteristics
Age at surgery: 14 months
8. Status post-stenting of the left pulmonary artery
Diagnosis:
1.Corrected transposition of the great arteries
History:
1.Postnatal diagnosis
{SLL}
2.Palliation with a Blalock–Taussig shunt at the
2.Pulmonary atresia
age of 1 week and placement of the stent into
3.Ventricular septal defect
the left pulmonary artery
4.Left pulmonary artery stenosis
3.Elective surgery
5.Dextrocardia
6.Secundum atrial septal defect
Procedure:
1.Modified Senning procedure
7.Status post-Blalock–Taussig shunt
2.Rastelli operation
Specific Steps of Operation
Clip1
Preoperative findings.
Back
2 Corrected Transposition of the Great Arteries
75
Clip2
Back
External anatomy of the heart.
Clip3
Back
Opening of the right atrium and development of the
systemic venous baffle.
76
V. Hraška, P. Murín
Clip4
Back
Completion of the systemic venous baffle.
Clip5
Back
Development of the pulmonary venous atrium using in situ pericardium.
2 Corrected Transposition of the Great Arteries
77
Clip6
Back
Creation of the intraventricular baffle.
Clip7
Placement of the conduit.
Back
78
V. Hraška, P. Murín
Clip8
Back
Postoperative findings.
fullversion
Back
2 Corrected Transposition of the Great Arteries
79
enning–Rastelli Operation for Corrected Transposition of the
S
Great Arteries {IDD} with Noncommitted Ventricular Septal
Defect, Pulmonary Stenosis, Situs Inversus, and Levocardia
Patient Characteristics
Age at surgery: 15 months
7.Patent ductus arteriosus
Diagnosis:
1.Corrected transposition of the great arteries
8.Secundum atrial septal defect
{IDD}
9.Levocardia with left isomerism
2.Noncommitted, inlet ventricular septal defect
History:
1.Patent ductus arteriosus stenting after birth
3.Pulmonary atresia
2.Elective surgery
4.Stenosis of the right-sided pulmonary artery
5.Azygos continuation of the inferior vena cava
Procedure:
1.Modified Senning operation
6.All pulmonary veins are connected with the
2.Rastelli operation with enlargement of the
left-sided right atrium, creating the appearance
of total anomalous pulmonary venous drain-
ventricular septal defect
3.Right pulmonary artery plasty
age, while the interatrial septum with restrictive foramen ovale is “shifted” to the right.
Specific Steps of Operation
Clip1
Preoperative findings.
Back
80
V. Hraška, P. Murín
Clip2
Back
External anatomy of the heart.
Clip3
Back
Transection of the stented duct and mobilization of
the pulmonary arteries.
2 Corrected Transposition of the Great Arteries
81
Clip4
Back
Oblique opening of the left-sided atrium and resection of the interatrial septum.
Clip5
Back
Development of the posterior wall of the systemic
venous baffle with a trapezoid-shaped GORETEX© patch.
82
V. Hraška, P. Murín
Clip6
Back
The anterior wall of the systemic venous baffle is
developed.
Clip7
Back
Development of the pulmonary venous atrium using pericardium in situ.
2 Corrected Transposition of the Great Arteries
83
Clip8
Back
Evaluation of intracardiac anatomy.
Clip9
Creation of the intraventricular baffle.
Back
84
V. Hraška, P. Murín
Clip10
Back
Stent resection and placement of the conduit.
Clip11
Back
Postoperative findings.
fullversion
Back
2 Corrected Transposition of the Great Arteries
85
odified Half-Mustard and Rastelli Operation
M
for Corrected Transposition of the Great Arteries
{SLL} in Situs Solitus with Dextrocardia
Patient Characteristics
Age at operation: 5 years
Diagnosis:
1.Corrected transposition of the great arteries
{SLL}
History:
1.At a different institution, the single-ventricle
pathway had been chosen:
a. After birth, a Blalock–Taussig shunt
2.Pulmonary atresia
operation, with transection of the duct and
3.Ventricular septal defect
ligation of the left superior vena cava, was
4.Straddling and partial overriding of the mitral
performed.
valve
5.Secundum atrial septal defect
6.Patent ductus arteriosus
b. At the age of 6 months, a bidirectional
Glenn anastomosis was performed.
2.At the age of 5 years, the patient was referred
7.Left superior vena cava
to our institution for possible anatomical
8.Dextrocardia
repair.
Procedure:
1.Modified Half-Mustard
2.Rastelli Operation
Specific Steps of Operation
Clip1
Preoperative findings.
Back
86
V. Hraška, P. Murín
Clip2
Back
The interatrial septum is resected. Using a short,
longitudinally opened GORE-TEX© prosthesis, the
inferior vena cava is tunneled toward the left-sided
tricuspid valve, incorporating the coronary sinus
inside the tunnel.
fullversion
Back
2 Corrected Transposition of the Great Arteries
87
odified Senning and Bex–Nikaidoh Procedure for Corrected
M
Transposition of the Great Arteries {IDD} with an Inlet
Ventricular Septal Defect in Situs Inversus and Mesocardia
Patient Characteristics
Age at operation: 2 years
History:
Diagnosis:
1.Corrected transposition of the great arteries
Semi-elective operation at the age of 2 years due
{IDD}
to progressive cyanosis
2.Inlet type of ventricular septal defect
Procedure:
1.Modified Senning procedure
3.Valvar and long segment subvalvar pulmonary
2.Bex–Nikaidoh operation
stenosis
4.Straddling of the tricuspid valve
5.Atrial septal defect
3.Reposition of the anomalous chordal attachment of the tricuspid valve
4.Reconstruction of the right ventricular outflow
tract with a pulmonary homograft
A cyanotic, 2-year-old girl was referred to our
center with a diagnosis of congenitally corrected
transposition of the great arteries {IDD} and severe subpulmonary obstruction. The echocardiogram revealed an inlet type of ventricular septal
defect, with straddling of the tricuspid valve and
valvular and subvalvular pulmonary stenosis.
Catheterization confirmed a long segment of left
ventricular outflow tract obstruction, with sys-
temic pressure in the left-sided, morphological left
ventricle, and good architecture of the pulmonary
artery, with low pulmonary artery resistance. Because of the inlet-type of ventricular septal defect,
the long segment of subpulmonary narrowing, valvar pulmonary stenosis, and straddling of tricuspid valve, aortic translocation was considered as
a treatment option instead of a Rastelli operation
combined with a Senning.
88
V. Hraška, P. Murín
Specific Steps of Operation
After finishing the Senning procedure, the Bex–Nikaidoh procedure was performed with the following steps:
1.Dissection and mobilization of the left coronary artery
2.The aorta and pulmonary artery are transected.
2 Corrected Transposition of the Great Arteries
3.The left and right coronary arteries are excised and extensively mobilized.
The left coronary artery, in particular, is mobilized with all the ventricular
branches that supply the right ventricular outflow tract. The aortic root is
harvested from the right ventricle with an 8- to 10-mm cuff of muscle.
4.The pulmonary valve is excised, and the outlet septum is transected into the
superior corner of the ventricular septal defect. A vessel loop passes through
the ventricular septal defect from one inlet to another. One of the primary
chordal attachments of the tricuspid valve to the ventricular septal defect has
to be detached because of straddling (this cannot be seen).
89
90
V. Hraška, P. Murín
5.The aortic root is seated into the left ventricular outflow tract using a continuous suture technique. At this point, there is a large anterior defect in
the left ventricular outflow tract from the margin of the ventricular septal
defect to the aortic root. This area is covered with a Dacron patch, using
interrupted pledgeted sutures. The rest of the aortic root is attached to this
newly created interventricular septum by continuous suture technique. Half
of the anastomosis is reinforced by another suture line using the remnant of
the pulmonary artery wall. The detached chordae of the tricuspidal valve is
re-attached to the appropriate position.
6.The right coronary artery is implanted into the harvest site (not shown). The
left coronary artery is implanted anterior and to the right of the harvest site.
The harvest site is covered by pericardium. After the Lecompte maneuver,
the aortic root is anastomosed with the ascending aorta.
2 Corrected Transposition of the Great Arteries
91
7.The aortic cross clamp is released. During rewarming, a 22-mm diameter
pulmonary homograft is placed into the right ventricular outflow tract. The
bifurcation of the pulmonary artery is partially closed, moving the anastomosis between homograft and pulmonary artery to the right.
8.Angiography 1 year after surgery
Clip1
Back
92
V. Hraška, P. Murín
Recommended Reading
Anderson RH, Arnold R, Wilkinson JL (1973) The conduction tissue in congenitally corrected transposition. Lancet
1:1286–1287
Hu SS, Liu ZG, Li SJ et al (2008) Strategy for biventricular outflow tract reconstruction: Rastelli, REV, or Nikaidoh procedure?
J Thorac Cardiovasc Surg 135:331–338
Bautista-Hernandez V, Marx GR, Gauvreau K et al (2006) Determinants of left ventricular dysfunction after anatomic repair
of congenitally corrected transposition of the great arteries. Ann
Thorac Surg 82:2059–2065
Ilbawi MN, DeLeon SY, Backer CL et al (1990) An alternative
approach to the surgical management of physiologically corrected transposition witch ventricular septal defect and pulmonary stenosis or atresia. J Thorac Cardiovasc Surg 100:410–415
Brawn WJ, Barron DJ (2003) Technical aspects of the Rastelli
and atrial switch procedure for congenitally corrected transposition of the great arteries with ventricular septal defect and
pulmonary stenosis or atresia: results of therapy. Semin Thorac
Cardiovasc Surg Pediatr Card Surg Annu 6:4–8
Jacobs ML, Pelletier G, Wearden PD et al (2006) The role of
Fontan’s procedure and aortic translocation in the surgical management of patients with discordant atrioventricular connections, interventricular communication, and pulmonary stenosis
or atresia. Cardiol Young 16:97–102
Brawn WJ, Jones TJJ, Anderson RH et al (2010) Congenitally
corrected transposition. In: Anderson RH, Becker EJ, Penny D
et al (eds). Pediatric cardiology, 3rd edn. Churchill-Livingstone,
Philadelphia, pp 818–835
Langley SM, Winlaw DS, Stumper O et al (2003) Midterm results after restoration of the morphologically left ventricle to
the systemic circulation in patients with congenitally corrected
transposition of the great arteries. J Thorac Cardiovasc Surg
125:1229–1241
Brawn WJ (2005) The double switch for atrioventricular discordance. Semin Thorac Cardiovasc Surg Pediatr Card Surg Ann
8:51–56
Davies B, Oppido G, Wilkinson JL et al (2008) Aortic translocation, Senning procedure and right ventricular outflow tract augmentation for congenitally corrected transposition, ventricular
septal defect and pulmonary stenosis. Eur J Cardiothorac Surg
33:934–936
Ly M, Belli E, Leobon B et al (2009) Results of the double
switch operation for congenitally corrected transposition of the
great arteries. Eur J Cardiothorac Surg 35:879–84
Mee RB (2005) The double switch operation with accent on the
Senning component. Semin Thorac Cardiovasc Surg Pediatr
Card Surg Ann 8:57–65
Duncan BW, Mee RB, Mesia CI et al (2003) Results of the double switch operation for congenitally corrected transposition of
the great arteries. Eur J Cardiothorac Surg 24:11–19
Morell VO, Jacobs JP, Quintessenza JA (2005) Aortic translocation in the management of transposition of the great arteries
with ventricular septal defect and pulmonary stenosis: results
and follow-up. Ann Thorac Surg 79:2089–2092
Gaies MG, Goldberg CS, Ohye RG et al (2009) Early and intermediate outcome after anatomic repair of congenitally corrected transposition of the great arteries. Ann Thorac Surg
88:1952–1960
Nido PJ del, Hraška V, Mayer JE Jr (1998) Congenitally corrected transposition of the great arteries. In: Kaiser LR, Kron IL,
Spray TL (eds) Mastery of cardiothoracic surgery. LippincottRaven, New York, pp 800–804
Helvind MH, McCarthy JF, Imamura M et al (1998) Ventriculoarterial discordance: switching the morphologically left ventricle into the systemic circulation after 3 months of age. Eur J
Cardiothorac Surg 14:173–178
Quinn DW, McGuirk SP, Metha C et al (2008) The morphologic
left ventricle that requires training by means of pulmonary artery banding before the double-switch procedure for congenitally corrected transposition of the great arteries is at risk of late
dysfunction. J Thorac Cardiovasc Surg 135:1137–1144
Hosseinpour AR, McCarthy KP, Griselli M et al (2004) Congenitally corrected transposition: size of the pulmonary trunk
and septal malalignment. Ann Thorac Surg 77:2163–2166
Hraška, V (2008) Anatomic correction of corrected transposition {IDD} using an atrial switch and aortic translocation. Ann
Thorac Surg 85:352–353
Hraška V, Duncan BW, Mayer JE et al (2005) Long-term outcome of surgically treated patients with corrected transposition
of the great arteries. J Thorac Cardiovasc Surg 129:182–191
Hraška V, Mattes A, Haun C et al (2011) Functional outcome of
anatomic correction of corrected transposition of the great arteries. Eur J Cardiothorac Surg. 40:1227–1235
Hraška V, Murín P, Arenz C et al (2011). The modified Senning
procedure as an integral part of an anatomical correction of congenitally corrected transposition of the great arteries. MMCTS.
doi:10.1510/mmcts.2009.004234
Shin’oka T, Kurosawa H, Imai Y et al (2007) Outcomes of definitive surgical repair for congenitally corrected transposition
of the great arteries or double outlet right ventricle with discordant atrioventricular connections: risk analyses in 189 patients.
J Thorac Cardiovasc Surg 133:1318–1328
Weyand K, Haun C, Blaschczok H et al (2010) Surgical treatment of transposition of the great arteries with ventricular septal
defect and left ventricular outflow tract obstruction: midtermresults. World J Pediatr Congenital Heart Surg 2:163–169
Wilkinson JL, Cochrane AD, Karl TR (2000) Corrected (discordant) transposition of the great arteries (and related malformation). Annals 69(Suppl):S236–S248